Search
- Page Path
- HOME > Search
Original Article
- Diagnostic Utility of the Sysmex UF-5000 Flow Cytometer in Acute Bacterial Prostatitis: A Retrospective Pilot Study
- Young Kyu Han, Jeong Woo Lee, Hae-Il Park, Jin Bong Choi
- Urogenit Tract Infect 2025;20(2):107-113. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550022011
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader - Purpose
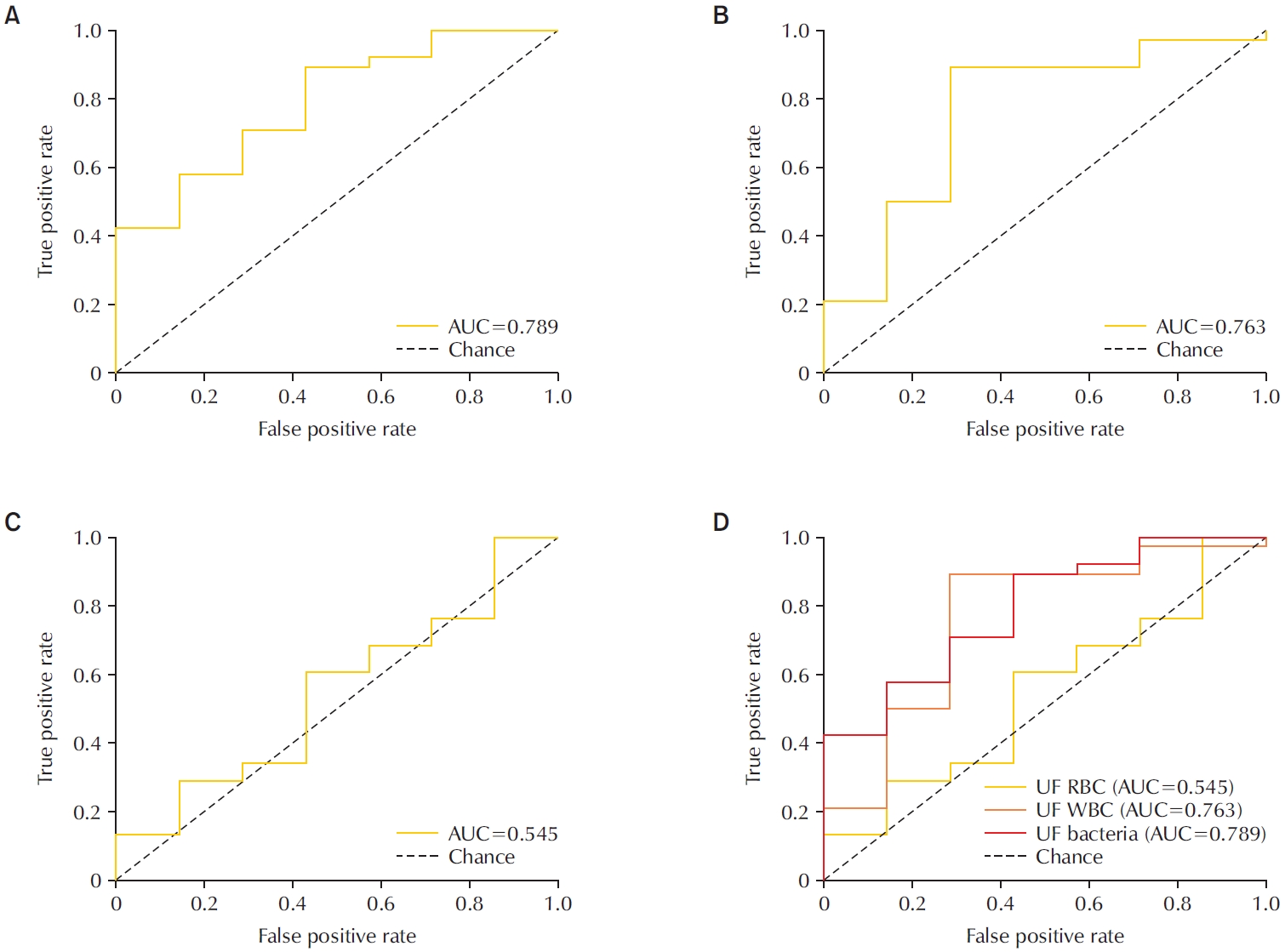
To evaluate the diagnostic performance of the Sysmex UF-5000 flow cytometer in detecting acute bacterial prostatitis (ABP) compared to standard urine culture. Materials and Methods: This retrospective study analyzed 45 urine samples from patients with a clinical diagnosis of ABP. Each sample was evaluated using the UF-5000 to measure red blood cells (RBC), white blood cells (WBC), and bacterial counts, and the results were compared with those from standard urine culture and Gram staining. Receiver operating characteristic curves were generated, and sensitivity, specificity, positive predictive value (PPV), and negative predictive value were determined. Concordance between Gram classification by the UF-5000 and conventional Gram staining was also evaluated.
Results
Of the 45 patients, 84.4% had positive urine cultures. The bacterial count parameter demonstrated the highest diagnostic performance (area under the curve [AUC]=0.79; sensitivity, 89.5%; PPV, 91.9%), outperforming WBC (AUC=0.76) and RBC (AUC=0.55). The Gram classification flag showed an overall concordance of 85.7% with conventional Gram staining, with a concordance rate of 88% for Gram-negative organisms.
Conclusions
The Sysmex UF-5000 exhibited good concordance with urine culture for patients with ABP, particularly through the bacterial count parameter. Although it does not replace culture, the UF-5000 may serve as a rapid adjunctive tool to support early clinical decision-making in suspected ABP cases. -
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef - A Commentary on “Diagnostic Utility of the Sysmex UF-5000 Flow Cytometer in Acute Bacterial Prostatitis: A Retrospective Pilot Study”
Dong-Hoon Lim
Urogenital Tract Infection.2025; 20(3): 173. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 1,463 View
- 30 Download
- 2 Crossref

Review Articles
- Molecular Mechanisms of Antibiotic Resistance in Uropathogenic Escherichia coli: A Narrative Review
- Nakjun Choi, Dong Uk Kim, Eun-Jin Lee
- Urogenit Tract Infect 2025;20(2):96-106. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550018009
-
 Abstract
Abstract
 PDF
PDF PubReader
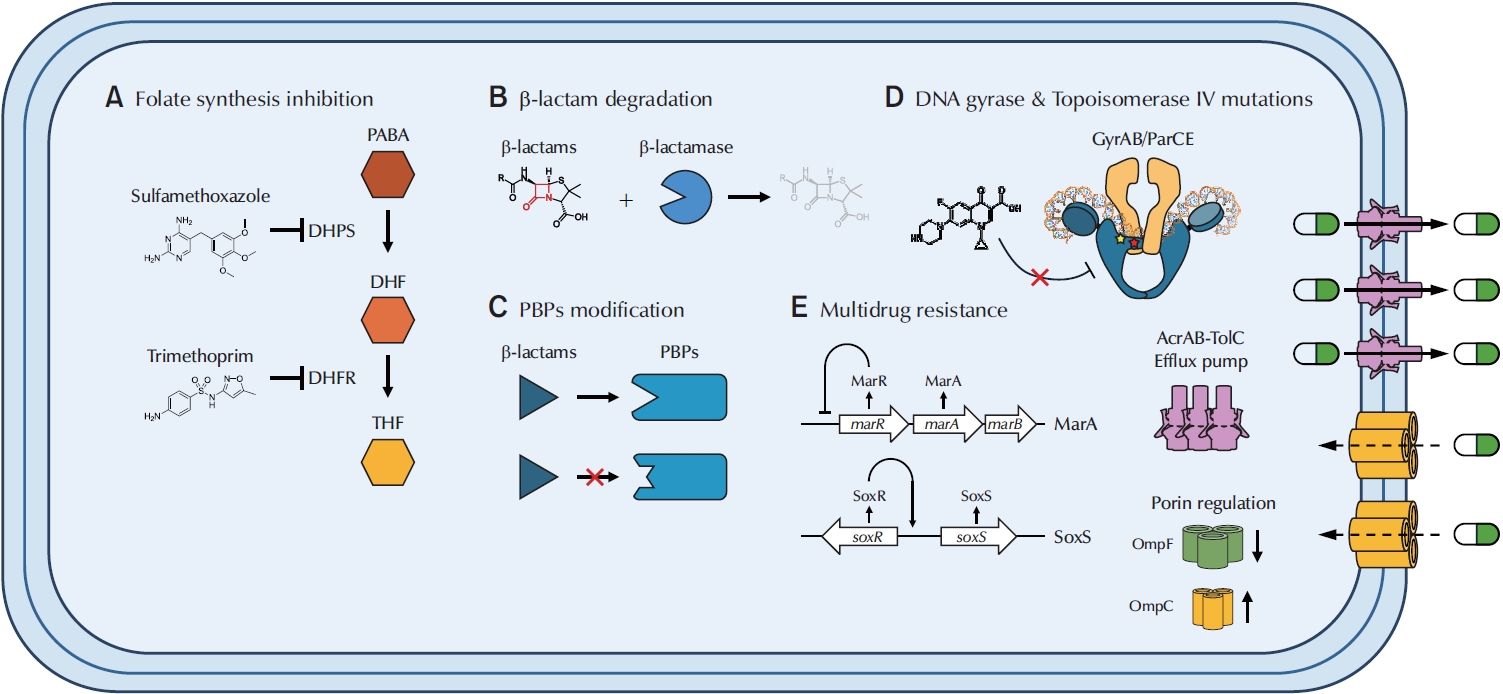
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections worldwide, with uropathogenic Escherichia coli (UPEC) serving as the primary causative agent. Although antibiotic therapy remains the standard of care for UTI treatment, the increasing prevalence of antimicrobial resistance has substantially reduced the effectiveness of commonly prescribed antibiotics. Resistance to trimethoprim-sulfamethoxazole (TMP-SMX), β-lactams, and fluoroquinolones is particularly concerning, as these agents constitute the principal therapeutic options for UTIs. This review examines the molecular mechanisms underlying UPEC resistance to these three classes of antibiotics, including target site modifications, efflux pump overexpression, porin regulation, and enzymatic degradation. Furthermore, it explores how these resistance determinants contribute to the development of multidrug-resistant (MDR) UPEC strains, which demonstrate cross-resistance to multiple antibiotics and present significant challenges for clinical management. Novel therapeutic strategies, such as efflux pump inhibitors, bacteriophage therapy, and genomic-guided precision medicine, are under investigation as potential solutions to address the growing global burden of MDR UPEC, alongside alternative non-antibiotic treatments. This review aims to provide a comprehensive overview of the genetic and regulatory pathways driving antibiotic resistance in UPEC, offering insights that may guide the development of effective treatment strategies and help mitigate the ongoing spread of antimicrobial resistance.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,951 View
- 111 Download
- 1 Crossref

- The Role of the Urinary Microbiome in the Prevention of Pediatric Urinary Tract Infections: A Narrative Review
- Byeongdo Song
- Urogenit Tract Infect 2025;20(2):82-95. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550016008
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader - Urinary tract infections (UTIs) are a common condition in children and often lead to hospitalization. A considerable proportion of children with UTIs (up to 30%) experience at least one recurrence, placing them at risk for long-term complications such as renal scarring. Since the concept of the microbiome was first introduced in 2001, increasing attention has been given to the role of the urinary tract microbiome in maintaining urinary tract homeostasis. Dysbiosis of the urinary microbiome has been recognized as a factor associated with an increased risk of various urinary tract diseases, including UTIs. However, the specific role of the urinary microbiome in the pathophysiology of pediatric UTIs remains incompletely understood. The present review examines recent studies on the urinary microbiome in children and summarizes current strategies for modulating the urinary microbiome to prevent UTI recurrence in the pediatric population.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 3,964 View
- 57 Download
- 1 Crossref

- Beta-Lactamase-Mediated Antibiotic Resistance in Urinary Tract Infections: Mechanisms and Therapeutic Strategies
- Fanglin Shao, Dengxiong Li, Jie Wang, Zhouting Tuo, Zhipeng Wang, Wuran Wei, Ruicheng Wu, Dechao Feng
- Urogenit Tract Infect 2025;20(2):67-81. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550012006
-
 Abstract
Abstract
 PDF
PDF PubReader
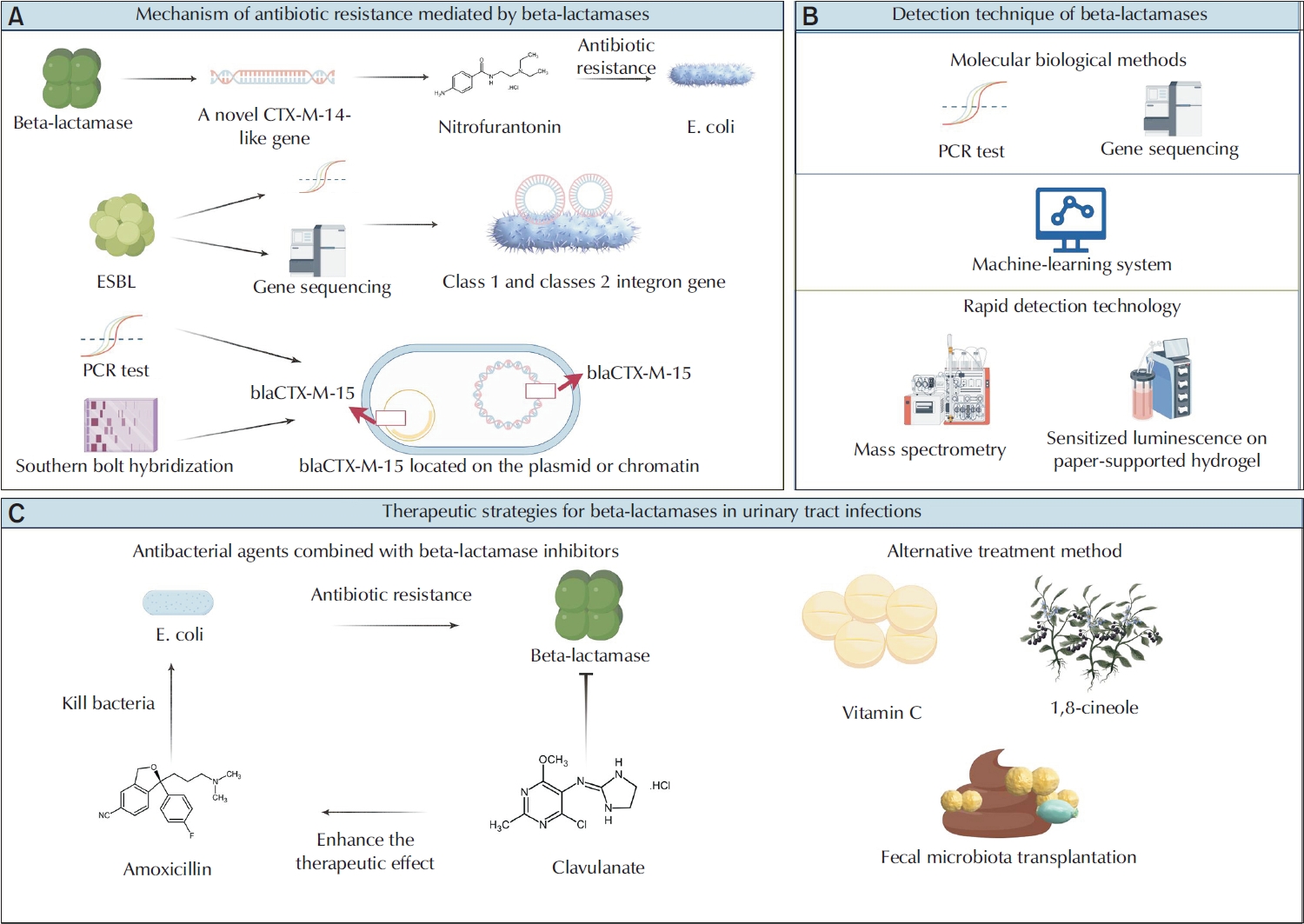
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections globally, and are primarily caused by Escherichia and Klebsiella. The overprescription and inappropriate use of antibiotics have accelerated the emergence of multidrug-resistant bacteria. Beta-lactamases play a critical role in mediating antibiotic resistance in UTIs. These enzymes promote bacterial resistance through multiple mechanisms, including gene mutation, plasmid-mediated horizontal gene transfer, and the involvement of integrons. Comprehensive knowledge of the ways in which beta-lactamases contribute to resistance in UTIs is essential for improving treatment strategies. Advances in detection technologies, such as gene sequencing and mass spectrometry, have greatly enhanced the ability to monitor and predict bacterial resistance. Current therapeutic strategies include the application of beta-lactamase inhibitors, the development of novel antibiotics, and alternative treatments that have shown efficacy against beta-lactamase-mediated antibiotic resistance. This paper reviews the mechanisms of beta-lactamase-mediated resistance in UTIs and provides an in-depth overview of several detection methods and therapeutic approaches.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 6,488 View
- 73 Download
- 1 Crossref

- Asymptomatic Bacteriuria in Older Adults – Diagnosis, Management, and Future Directions: A Narrative Review
- Ki Hong Kim, Hee Jo Yang
- Urogenit Tract Infect 2025;20(2):58-66. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550002001
-
 Abstract
Abstract
 PDF
PDF PubReader
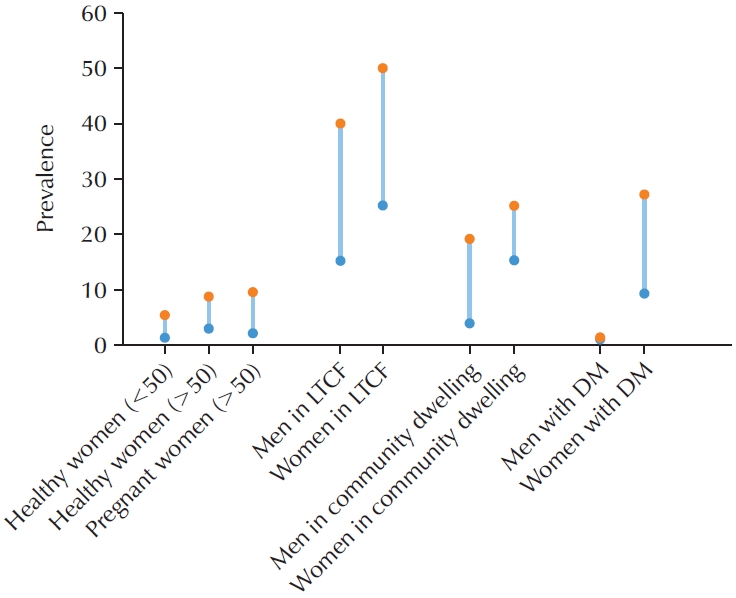
PubReader - Asymptomatic bacteriuria (ASB) is defined as the presence of bacteria in the urine in the absence of urinary tract infection (UTI) symptoms. The prevalence of ASB increases with advancing age, particularly among older patients with underlying health conditions. ASB is especially common among residents of long-term care facilities; however, distinguishing ASB from symptomatic UTI in this population remains a significant clinical challenge. The frequent occurrence of ASB often results in unnecessary antibiotic administration, thereby contributing to the development of antibiotic resistance. Current clinical guidelines recommend screening for and treating ASB only in certain circumstances, such as prior to urological procedures or in pregnant women. There is a pressing need for improved diagnostic approaches to differentiate ASB more accurately from UTI, particularly in older adults. Reducing unnecessary urine testing and inappropriate antibiotic use may help prevent over-treatment and minimize associated risks, including Clostridium difficile infection and increased antimicrobial resistance.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 11,535 View
- 116 Download
- 1 Crossref

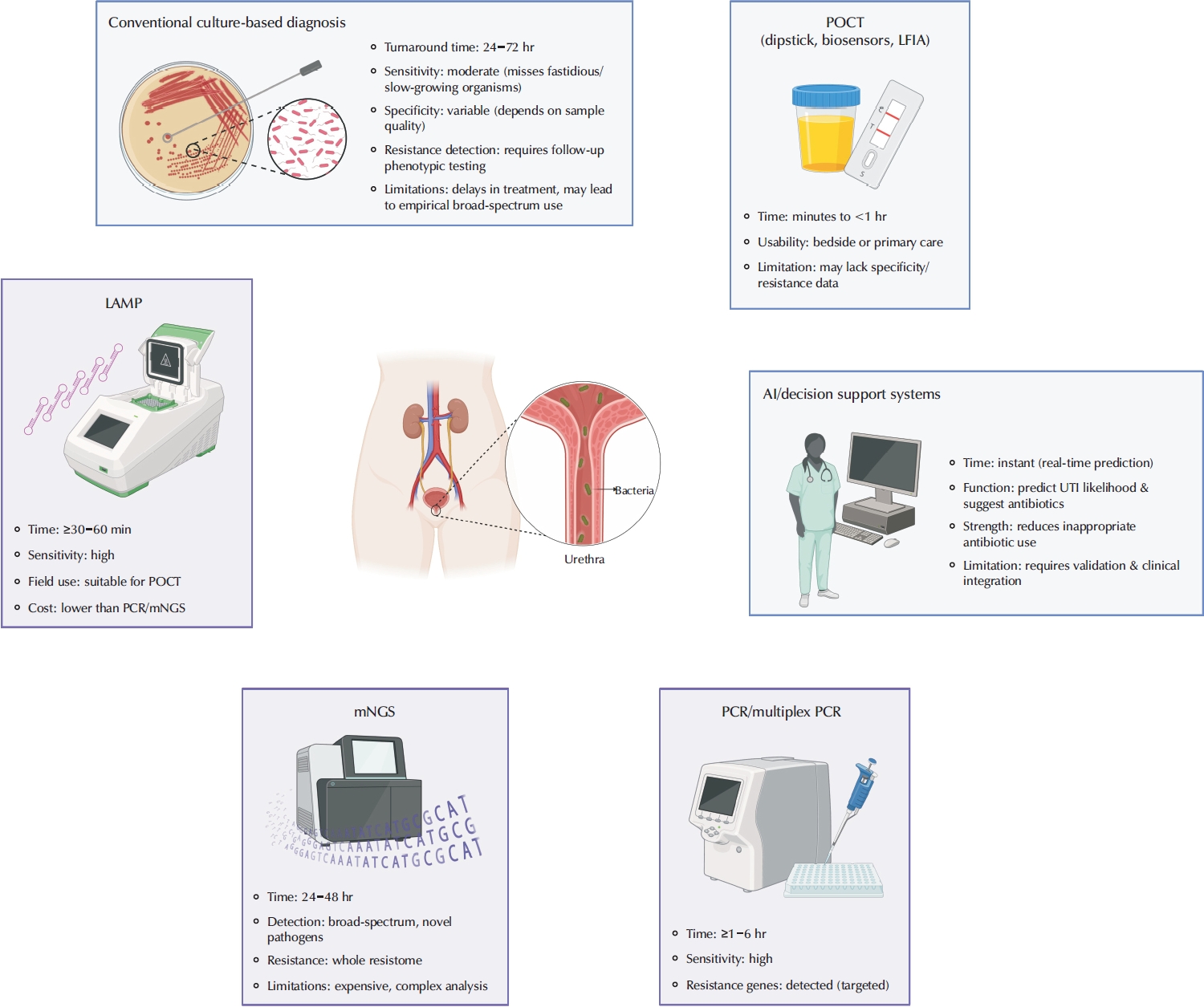
- Advances in the Diagnosis of Urinary Tract Infection: A Narrative Review
- Juan Victor Ariel Franco, Nicolás Meza
- Urogenit Tract Infect 2025;20(1):17-27. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550020010
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary tract infections are among the most frequent bacterial infections, significantly impacting patient morbidity and healthcare resources. Prompt and accurate diagnosis is crucial to ensure effective treatment, prevent complications such as pyelonephritis or sepsis, and reduce inappropriate antibiotic use, contributing to antimicrobial resistance (AMR). Despite consensus across international guidelines from organizations, challenges persist, particularly in distinguishing true infections from asymptomatic bacteriuria or nonspecific symptoms, especially in older adults. Recent advancements in diagnostic technology have emerged to address these limitations, including molecular diagnostics, point-of-care testing (POCT), and artificial intelligence (AI)-driven predictive models. Molecular techniques, notably polymerase chain reaction, loop-mediated isothermal amplification, and metagenomic next-generation sequencing, offer enhanced sensitivity and specificity, rapid detection times, and comprehensive identification of pathogens and resistance profiles. POCT innovations, such as lateral flow immunoassays, enzymatic-based rapid tests, and novel biosensors, facilitate prompt bedside diagnosis, although specificity challenges remain. Meanwhile, AI and machine learning models demonstrate significant potential for risk stratification, prediction of infection, and improving antibiotics prescription practices yet face barriers related to validation, practical integration, and clinical acceptability. Despite promising developments, significant gaps remain, including limited real-world implementation evidence, high costs, and insufficient data from diverse populations. Further rigorous clinical studies, economic evaluations, and practical implementation assessments are urgently required. Addressing these research gaps could substantially improve patient outcomes, optimize antibiotic stewardship, and reduce the global burden of AMR.
-
Citations
Citations to this article as recorded by- Diagnosis of urinary tract infections in the pediatric population – current practices, advances and progress
Maria Bitsori, Roza-Ioanna Poulaki, Emmanouil Galanakis
Expert Review of Anti-infective Therapy.2026; : 1. CrossRef - Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
- Diagnosis of urinary tract infections in the pediatric population – current practices, advances and progress
- 10,121 View
- 302 Download
- 2 Crossref

- Emerging Insights Into Microbiome Therapeutics for Urinary Tract Infections: A Narrative Review
- Hoonhee Seo, Md Abdur Rahim, Indrajeet Barman, Mohammed Solayman Hossain, Hanieh Tajdozian, Fatemeh Ghorbanian, Md Sarower Hossen Shuvo, Jiho Choi, Sukyung Kim, Heejo Yang, Ho-Yeon Song
- Urogenit Tract Infect 2025;20(1):4-16. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2448034017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary tract infections (UTIs) are among the most common bacterial infections worldwide, affecting millions annually and posing a significant global health concern. Traditional therapies for UTIs are becoming increasingly ineffective due to rising drug resistance and their tendency to disrupt the host's healthy microbiota, leading to further side effects. Consequently, there is an urgent need to develop alternative therapeutic agents that differ from conventional regimens and have fewer or no side effects. In this context, microbiome therapeutics offer a promising solution, given their demonstrated efficacy against various infectious diseases. Advances in scientific technology, particularly next-generation sequencing, have deepened our understanding of urinary microbiome dynamics, revealing a complex interplay within the urobiome that influences the onset and progression of UTIs. Uropathogenic bacteria do not solely cause UTIs; shifts in the composition of the urinary microbiome and interactions within the microbial community, known as host-microbiota interactions, also play a significant role. Although recent studies underscore the potential of targeting the urinary microbiome to manage UTIs and related complications, this field is still emerging and faces numerous regulatory and technical challenges. Further in-depth and comprehensive research is required to advance this pioneering concept into clinical practice.
-
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Efficacy and safety of N-acetylcysteine vs. probiotics in in-vivo biofilm prevention on ureteral stents: a prospective randomized controlled pilot in vivo study
Iqbal Singh, Himanshu Agrawal, Shailender Maurya, Himanshu Tanwar, Sanjay Gupta, N. P. Singh
International Urology and Nephrology.2025; 58(3): 811. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 14,185 View
- 168 Download
- 2 Crossref

Original Article
- Outbreak of Cystoscopy-Related Urinary Tract Infections With Pseudomonas aeruginosa in South Korea, 2022: A Case Series
- Beomsoo Kim, Young-Sin Choi, Jun-Koo Kang, Yun-Sok Ha, Seock Hwan Choi, Bum Soo Kim, Hyun Tae Kim, Eun Sang Yoo, Tae Gyun Kwon, Jae-Wook Chung, Tae-Hwan Kim
- Urogenit Tract Infect 2024;19(3):97-103. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448028014
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
This study conducted an epidemiological investigation of Pseudomonas aeruginosa urinary tract infections (UTIs) following cystoscopy at Chilgok Kyungpook National University Hospital. Materials and Methods: From May 16 to July 15, 2022, among 353 patients who underwent cystoscopy, 6 patients reported febrile UTIs following cystoscopy. They were admitted to the urology department of the hospital after visiting the Emergency Department. P. aeruginosa was found in the urine cultures of 4 of the 6 hospitalized patients. During the epidemiological investigation, no changes were observed in factors such as the reprocessing procedures for endoscopic equipment. Therefore, microbiological tests were performed using environmental samples derived from the endoscopic equipment and cleaning process.
Results
P. aeruginosa was identified in a dual-enzymatic detergent (EmPower) used during the endoscope cleaning process. After changing the disinfectant and cleaning process, no further bacterial growth was observed in subsequent microbiological tests.
Conclusions
This study highlights the potential of cystoscopes to serve as reservoirs for bacteria due to inadequate cleaning during the disinfection process. To minimize the risk of infections following cystoscopy, it is important to pay close attention to the reprocessing and cleaning of cystoscopes. -
Citations
Citations to this article as recorded by- A Commentary on “Outbreak of Cystoscopy-Related Urinary Tract Infections With Pseudomonas aeruginosa in South Korea, 2022: A Case Series”
Byoungkyu Han
Urogenital Tract Infection.2025; 20(1): 52. CrossRef
- A Commentary on “Outbreak of Cystoscopy-Related Urinary Tract Infections With Pseudomonas aeruginosa in South Korea, 2022: A Case Series”
- 3,954 View
- 70 Download
- 1 Crossref

Review Article
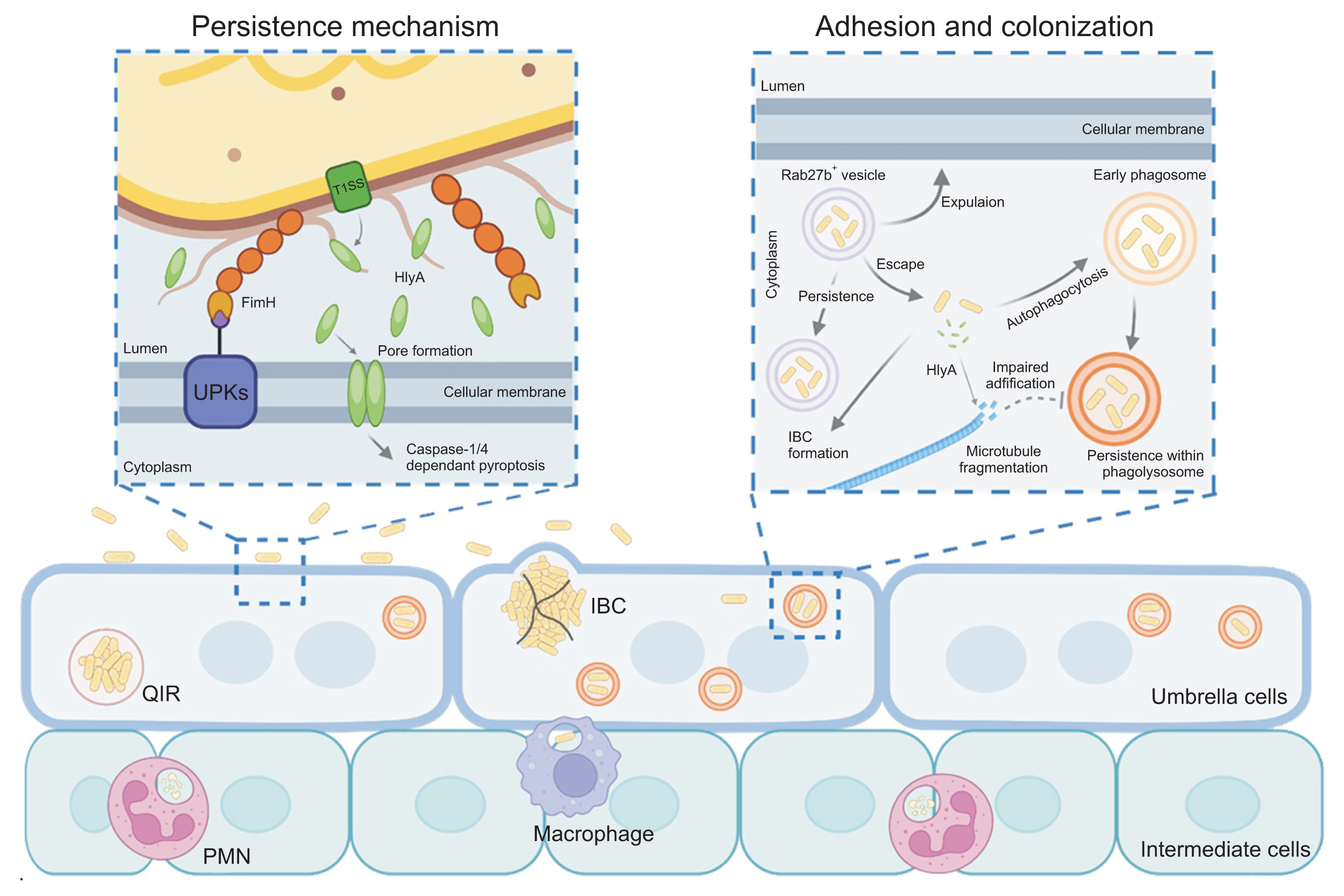
- Mechanistic Insights Into Persistent Bacterial Cystitis as a Basis for Vaccine Development: A Narrative Review
- Karen Serrano-Arevalo, Manisha Naskar, Hae Woong Choi
- Urogenit Tract Infect 2024;19(3):60-72. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448022011
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary tract infections (UTIs) are primarily caused by uropathogenic Escherichia coli (UPEC), which frequently lead to recurrent infections. These bacteria utilize several strategies to establish infection in the host; in particular, virulence factors such as fimbriae and α-hemolysin facilitate persistent infection, evade host immune responses, and minimize antibiotic exposure. To date, antibiotics have been the primary treatment for UTIs. However, an increasing emphasis has been placed on the need for UTI vaccines, with mucosal vaccine products now available in several countries. Additionally, vaccines targeting intracellular UPEC, utilizing adjuvants, are currently under development. Understanding the pathogenic mechanisms of uropathogens has enabled the development of new treatment approaches, paving the way for next-generation preventive and therapeutic methods that could effectively manage recurrent UTIs in the future.
-
Citations
Citations to this article as recorded by- Mechanisms and clinical implications of bacterial persistence in recurrent urinary tract infections
Changil Choi, Dong Soo Kim, Jin Bong Choi, Taesoo Choi, Jeong Woo Lee
Investigative and Clinical Urology.2026; 67(2): 123. CrossRef - Bacterial biofilm – as a contributor to urinary tract infections
Zuzanna Trześniewska-Ofiara, Mariola Mendrycka, Agnieszka Woźniak-Kosek
Biuletyn Głównej Biblioteki Lekarskiej.2025; 58(384): 83. CrossRef
- Mechanisms and clinical implications of bacterial persistence in recurrent urinary tract infections
- 6,755 View
- 58 Download
- 2 Crossref

Original Article
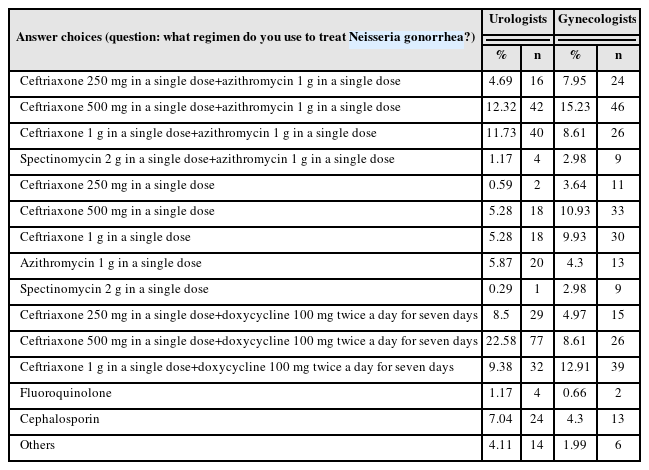
- Trend Analysis of Sexually Transmitted Infection Treatments in Korea
- Soeon Park, Byung Kyu Han, Sangrak Bae, Seung-Ju Lee, Jin Bong Choi
- Urogenit Tract Infect 2024;19(2):25-30. Published online August 31, 2024
- DOI: https://doi.org/10.14777/uti.2024.19.2.25
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: The revision of the 2023 Guidelines for the Treatment of Sexually Transmitted Infections (STIs) has been released. Hence, it is necessary to analyze the current status of STI treatments in Korea.
Materials and Methods: A questionnaire was distributed to urologists and gynecologists from December 2022 to January 2023 through an online survey program. Three hundred and forty-one urologists and 302 gynecologists responded to the questionnaire.
Results: For Neisseria gonorrhea treatment, ceftriaxone 500 mg and 100 mg of doxycycline twice daily for seven days were most preferred by urologists (22.58%). The treatment most preferred by gynecologists (15.23%) was 500 mg of ceftriaxone and 1 g of azithromycin in a single dose. Both urologists and gynecologists generally treat Chlamydia trachomatis according to the treatment guidelines. For treating Mycoplasma genitalium, 29.03% of urologists preferred administering azithro-mycin at 500 mg once daily, followed by 250 mg for four days. In contrast, 33.11% of gynecologists preferred doxycycline 100 mg twice daily for seven days.
Conclusions: Most urologists and gynecologists followed the treatments recommended in the 2nd edition of the STI treatment guidelines, revised in 2016. As many treatment regimens have changed because of the recent increase in antibiotic-resistant STIs, there is a need to encourage them to follow the new treatment guidelines. -
Citations
Citations to this article as recorded by- Comparative Study of the Clinical Characteristics of Patients With Sexually Transmitted Infections Diagnosed by Nucleic Acid Amplification Tests
Jung Soo Son, Namhee Kim, Hong Sang Oh, Sang Won Park, Dong Hoon Shin
Journal of Korean Medical Science.2025;[Epub] CrossRef
- Comparative Study of the Clinical Characteristics of Patients With Sexually Transmitted Infections Diagnosed by Nucleic Acid Amplification Tests
- 6,767 View
- 36 Download
- 1 Crossref

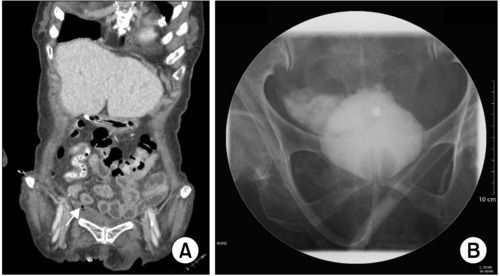
Case Report
- Spontaneous Bladder Perforation in a Patient with a Long-Term Intraurethral Catheter
- Taegi Choi, Hyunkyung Lee, Junseok Kim, Sunghoon Lee, Younkyung Cho, Eunyoung Kang, Jinsun Kang, Sumin Lee, Eunju Na
- Urogenit Tract Infect 2023;18(3):110-113. Published online December 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.3.110
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary catheters are commonly used to address various urinary problems. However, the catheter itself can be a cause of several complications, including catheter-associated urinary tract infections, damage to the bladder and kidneys, and, in extremely rare cases, bladder perforation. We present a case of spontaneous bladder perforation in a patient who had a long-term indwelling intraurethral catheter. The patient with prior hypoxic brain damage suddenly developed tachypnea, tachycardia, and oxygen desaturation. Computed tomography and retrograde cystography revealed an extraperitoneal bladder perforation with an intra-pelvic abscess. Antibiotics were prescribed and a urinary catheter was inserted for drainage. After 11 weeks, the abscess resolved, and the catheter was removed to enable self-voiding. The perforation was attributed to chronic inflammation and distension of the bladder wall caused by the intraurethral catheter. Given the potential complications associated with long-term urinary catheterization, the timely removal of indwelling catheters should be considered.
- 4,736 View
- 18 Download

Original Articles
- Impact of Microbial Infection on Sperm Parameters of Seminal Bacteria in Asymptomatic Subfertile Males
- Sae Byuk Chang, Tae Jin Kim, Tae Heon Kim, Seung-Ryeol Lee, Young Kwon Hong, Dong Soo Park, Sun-Mi Cho, Dong Hyeon Lee, Young Dong Yu
- Urogenit Tract Infect 2023;18(3):82-92. Published online December 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.3.82
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study examined the effects of asymptomatic bacteriospermia on the semen quality of subfertile males. The types of bacteria and their antibiotic susceptibility were also analyzed.
Materials and Methods: Semen was collected and analyzed from 510 subfertile males. One hundred and seventy-nine males showed bacteriospermia, while 331 males did not. The bacterial species, sperm parameters, hormone levels, underlying disease, and lifestyle patterns were compared between the two study groups.
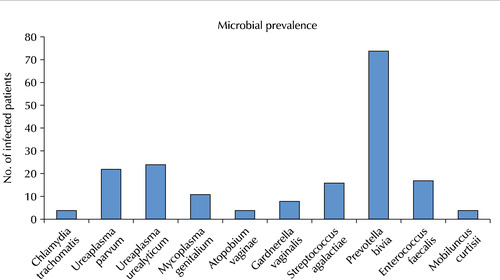
Results: The bacteriospermic males showed significantly higher rates of leukocytospermia (p=0.001) and deoxyribonucleic acid (DNA) fragmentation than the non-bacteriospermic males. Sperm motility was significantly lower in the bacteriospermic males than in non-bacteriospermic males. The most common seminal bacterial species were Prevotella bivia (P. bivia, 41.3%) and Ureaplasma urealyticum (U. urealyticum, 13.4%). U. parvum showed the highest recurrence rates (31.8%) three months after the initial antibiotic treatment. Regarding the sperm parameters of bacteriospermic males, the sperm concentration, total motility, progressive motility, leukocytospermia, and DNA fragmentation were improved significantly after the initial antibiotics treatment. Multivariate logistic regression analyses revealed P. bivia, U. urealyticum, and U. parvum to be associated with the decreased motility and increased DNA fragmentation of spermatozoa. P. bivia was also associated with a decreased sperm concentration (p=0.002) and vitality (p=0.013).
Conclusions: Bacteriospermia decreased the sperm concentration, motility, normal morphology, and vitality. P. bivia is the most commonly observed bacteria in subfertile males. Appropriate antibiotic therapy of seminal bacteria species had a strong positive impact on improving the semen parameters.
- 8,729 View
- 43 Download

- Feasibility of Anesthesia-Free Ureteroscopic Lithotripsy in Elderly Patients with Urinary Tract Infections
- Duk Yoon Kim, Hyun Jin Jung, Eun Kyoung Yang, Won Yeol Cho
- Urogenit Tract Infect 2023;18(2):60-63. Published online August 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.2.60
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: Patients with underlying diseases, particularly in the elderly, urinary tract obstruction with a ureter stone would progress to severe conditions. Some of them have poor general conditions to endure anesthesia. Therefore, this study validated the feasibility of ureteroscopic stone removal without anesthesia for elderly patients with ureter stones who were under impending septic conditions or severe urinary tract infections.
Materials and Methods: Thirty-four patients (16 males and 18 females) were included in this study. All of them had serious problems, making it difficult to endure anesthesia. Most of them were inserted pre-operative percutaneous nephrostomy catheter, and ureteroscopic lithotripsy was performed successfully after intravenous analgesic injection (pethidine 25 mg).
Results: The mean age was 71.8±10.84 years. The locations of the stones were upper ureter in 11, mid-ureter in 6, and lower ureter in 17 cases. Urine and blood cultures identified bacteria from 17/34 patients. Escherichia coli was the most common (10/17), followed in order by Klebsiella pneumoniae and Staphylococcus epidermidis in 5 and 2 cases, respectively. Most patients had an abnormal white blood cell count (19,400±4,233.3/l) and elevated C-reactive protein levels (110.3±83.6 mg/L). No patient had to stop the operation because of intolerable pain. The mean of the visual analog pain scale was 3.2±0.86. The overall success rate was 100%.
Conclusions: The trial of ureteroscopic lithotripsy after administering analgesics could improve the condition of elderly patients whose general condition is too poor to endure anesthesia without serious complications.
- 1,940 View
- 10 Download

Reviews
- Is Human Mpox a New Sexually Transmitted Infection in Korea That Should Be Monitored?
- Gilho Lee
- Urogenit Tract Infect 2023;18(2):35-44. Published online August 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.2.35
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Human monkeypox (mpox) outbreaks have been reported in more than 110 countries, with more than 86,930 confirmed cases. The World Health Organization has realized the seriousness of personal transmission and has declared a global health emergency against the infection. Traditionally, contact with infected animals in a few endemic countries has been a major transmission route of the mpox virus. On the other hand, the global mpox outbreak in 2022 has been primarily associated with sexual networks of men who have sex with men (MSM) and bisexual men exhibiting high-risk behaviors. Their common symptoms are initial fever, headache, swollen lymph nodes, and subsequent skin rashes. These presentations did not consistently occur in the 2022 outbreak. Many patients presented with skin lesions on the anogenital areas without prodromal symptoms. In addition, the atypical characteristics of the recent outbreak may result in a misdiagnosis of other skin lesions, such as chickenpox. Furthermore, infected persons are frequently co-infected with sexually transmitted infections (STIs) with similar skin lesions. The newly confirmed cases in Korea on April 2023 must have been infected through community transmission because these new patients had not traveled overseas in the past three months. Therefore, mpox is something that everybody should be concerned about in Korea. Medical practitioners must know the characteristics of the infection because patients with mpox may visit their offices with some genital lesions or other STIs. The clinical information from this paper may broaden and deepen the understanding of human mpox and curb the early transmission of the infection.
- 2,308 View
- 8 Download

- Prophylactic Antimicrobial Therapy and Antimicrobial Stewardship in Urologic Surgery
- Hee Jo Yang
- Urogenit Tract Infect 2023;18(1):8-14. Published online April 30, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.1.8
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Postoperative infectious complications are a worrying problem for surgeons. Urological surgery has a higher risk of postoperative urinary tract infection than other surgeries because of the common use of various types of catheters. Due to the recent increase in antibiotic resistance, antimicrobial stewardship recommends using appropriate antibiotics for a suitable period. It is generally advocated that prescribing antibiotics in the absence of infection is equivalent to the inappropriate use of antibiotics. Based on numerous studies reported by several academic societies, appropriate use of antibiotics before surgery has been suggested. It was confirmed that using antibiotics according to these guidelines reduces the use of antibiotics without increasing the incidence of postoperative infectious complications. Furthermore, endourological surgery reports have proved the efficacy of antibiotics given once before surgery. Differences in antibiotic resistance by region must be taken into consideration when selecting the appropriate antibiotic type.
- 8,012 View
- 100 Download

Original Article
- Evaluating Family Physicians’ Knowledge of Urinary Tract Infection in Southern Iran: Scale Development
- Hourvash Haghighinejad, Parisa Jooya, Raziye Saeedizade, Kaveh Taghipour, Fatemeh Malekpour
- Urogenit Tract Infect 2023;18(1):24-31. Published online April 30, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.1.24
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: Urinary tract infections (UTIs) often present with nonspecific symptoms in childhood and can result in serious complications. Therefore, it is imperative for the proper diagnosis, treatment, and follow-up of this affliction. We first designed a valid and reliable questionnaire. Subsequently, the study evaluated the knowledge of family physicians regarding pediatric UTI.
Materials and Methods: A questionnaire was designed to evaluate the family physicians’ knowledge of pediatric UTIs. The face and content validity and reliability of the questionnaire were first evaluated in a pilot study. Subsequently, doctors were asked to complete the questionnaire and data-collecting form delivered at their workplace.
Results: The validity and reliability of the questionnaire were deemed acceptable after omitting two questions. Cronbach's alpha of the final questionnaire was 0.71. More than 75% of the participants answered each question correctly. Approximately 50% of the physicians were post-graduates. Age was determined to be negatively correlated, and the "number of years of graduation" was positively correlated with the total score of the questionnaire.
Conclusions: The designed questionnaire had acceptable validity and reliability. Moreover, family physicians’ knowledge of pediatric UTIs was found to be favorable.
- 2,302 View
- 15 Download

Review
- Differences in Urine Microbiome of Acute Cystitis and Chronic Recurrent Cystitis in Women
- Woong Bin Kim
- Urogenit Tract Infect 2023;18(1):1-7. Published online April 30, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.1.1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The diagnosis of urinary tract infection (UTI) relies on urine culture tests to identify aerobic or anaerobic urinary tract pathogens. This method has limitations in identifying anaerobic bacteria, and there is uncertainty in identifying all bacteria. A new next-generation sequencing (NGS) method has gradually helped overcome these limitations, and the microorganisms present in the human urinary tract are gradually being revealed. This review introduces studies on the microbiome analyzed using NGS of urine from patients with acute cystitis and recurrent UTIs and discusses whether NGS may reveal the pathophysiology of the disease.
- 3,456 View
- 38 Download

Original Articles
- Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
- Gwon Kyeong Lee, Kyoung Ha Jang, Woo Seop Seong, Byeong Jin Kang, Kyung Hwan Kim, Hong Koo Ha
- Urogenit Tract Infect 2022;17(3):96-102. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.96
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study aimed to determine the treatment modality for prostatic abscesses according to size.
Materials and Methods: Twenty-five patients diagnosed with prostatic abscesses were retrospectively reviewed. All patients were treated with intravenous empirical and appropriate antibiotics according to culture results. They were grouped according to the size of the prostate abscess based on computed tomography results (group A, with prostate abscess ≤2 cm, n=10; group B, with prostate abscess size >2 cm, n=15), and their treatment modality and outcomes were compared.
Results: The prostatic abscess sizes were 1.31±0.37 and 3.49±1.06 cm for groups A and B, respectively. Prostate-specific antigen, prostatic volume, and comorbidity were not significantly different (p>0.05), whereas pelvic pain was significantly different (p=0.028). There was no difference in the microorganisms isolated from urine and blood culture, empirical antibiotics, and broad-spectrum antibiotics between the two groups (p>0.05). More patients in group B underwent transurethral abscess deroofing than those in group A (p=0.040). Patients in group B had a more extended hospitalization period and intravenous antibiotics duration than those in group A (p=0.024 and p=0.013, respectively). Group B had more cases of septic shock, intensive care unit admission, and mortality events than group A (p=0.024, p=0.001, and p=0.061, respectively). However, prostatic abscess recurrence and urological chronic complication did not significantly differ (p>0.05).
Conclusions: Appropriate use of antibiotics is crucial. This study shows that the treatment of patients with prostatic abscess >2 cm is more difficult, but transurethral abscess deroofing can lower mortality, prostatic abscess recurrence, and urological chronic complications.
- 4,856 View
- 27 Download

- Korean Multicenter Study of Infectious Complications after Transurethral Prostate Surgery in Patients with Preoperative Sterile Urine
- Seong Hyeon Yu, Seung Il Jung, Eu Chang Hwang, Tae-Hyoung Kim, Jae Duck Choi, Koo Han Yoo, Jeong Woo Lee, Dong Hoon Koh, Sangrak Bae, Seung Ok Yang, Joongwon Choi, Seung Ki Min, Hoon Choi
- Urogenit Tract Infect 2022;17(3):81-88. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.81
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: To evaluate the efficacy of antibiotic prophylaxis and determine the risk factors of infectious complications after transurethral surgery of the prostate.
Materials and Methods: Seven hundred and seventy-two patients who underwent transurethral resection of the prostate (TURP) or holmium laser enucleation of the prostate (HOLEP) were reviewed. Of these, this study enrolled 643 patients without bacteriuria who had not received antibiotics for urinary tract infections for two weeks before surgery. The patients were divided into two groups according to the duration of the antibiotics (Group 1: less than one day, n=396 vs. Group 2: more than one day, n=247).
Results: The overall incidence of postoperative infectious complications in 643 patients was 5.0% (32/643). When postoperative infectious complications were compared according to the duration of the antibiotics (Group 1 vs. Group 2), the infectious complications rates were 5.6% (22/396) vs. 4.0% (10/247), respectively (p=0.393). When postoperative infectious complications were compared according to the duration of antibiotics (Group 1 vs. Group 2) in the TURP and HOLEP groups, the infectious complications rates were 6.3% (12/192) vs. 1.0% (1/103) (p=0.035) and 4.9% (10/203) vs. 6.0% (8/134) (p=0.677), respectively. The duration of Foley catheterization was independently associated with infectious complications (p=0.003).
Conclusions: The results showed that prolonged postoperative catheterization affects postoperative infectious complications associated with transurethral prostate surgery. Although antibiotics administered for less than one day are effective for antibiotic prophylaxis of transurethral prostate surgery, a longer antibiotic therapy is recommended for TURP. -
Citations
Citations to this article as recorded by- Evaluation of Postoperative Urinary Tract Infection and Sepsis Rates After Adding Cystolitholapaxy to HoLEP:
A Retrospective Analysis
Federico Rovegno, Rajiv Pillai, Zafar Maan, Soumendra Datta, Omar Nasir, Gerald Rix
International Journal of Clinical Urology.2026; 10(1): 1. CrossRef
- Evaluation of Postoperative Urinary Tract Infection and Sepsis Rates After Adding Cystolitholapaxy to HoLEP:
A Retrospective Analysis
- 3,723 View
- 24 Download
- 1 Crossref

- Changes of Causative Organism and Antimicrobial Resistance in Urinary Tract Infections After the COVID-19
- Young Ho Choi, Jong Hyun Tae, Mi-Kyung Lee, Tae-Hyoung Kim
- Urogenit Tract Infect 2022;17(2):42-49. Published online August 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.2.42
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: During the coronavirus disease 2019 (COVID-19) pandemic, several studies reported changes in the distribution of microorganisms that cause major legal, respiratory, and gastrointestinal infectious diseases and increases in the antimicrobial resistance rates in Korea. On the other hand, there has been little domestic research on the causative organism of urinary tract infection (UTI). This study investigated the influence of the COVID-19 pandemic on the distribution of causative organisms and the antimicrobial resistance rate in UTI.
Materials and Methods: This study analyzed 17,201 urine cultures retrospectively from patients who visited Chung-Ang University Hospital from January 2018 to December 2021. Tests were then conducted to determine if there was a significant difference between the data for the eight quarters of the pre-COVID-19 period (January 2018 to December 2019) and the data for the eight quarters post-COVID-19 period (January 2020 to December 2021).
Results: Escherichia coli was the most common causative organism in all periods, but it decreased in the post-COVID-19 period. Enterococcus faecalis increased in the post-COVID-19 period. The ciprofloxacin resistance rate of E. coli and Klebsiella pneumoniae increased, but the ciprofloxacin and levofloxacin resistance rate of E. faecalis decreased.
Conclusions: There was little difference in the causative organism distribution of UTI and antimicrobial resistance rates before and after the COVID-19 pandemic. On the other hand, changes in some causative organisms are identified. Nevertheless, because this study was limited to a single medical institute, data from a broader spectrum of bacterial species collected from multiple institutions will be needed to obtain definitive results.
- 1,377 View
- 8 Download

Review
- Microbiome Analysis Using Next-Generation Sequencing in Urinary Tract Infections
- Hyunho Han, Joo Yong Lee
- Urogenit Tract Infect 2022;17(1):1-7. Published online April 30, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.1.1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - In recent decades, the understanding of the genetic information of microbes and hosts has advanced considerably with the development of next-generation sequencing (NGS). For infectious diseases, genomic analysis can provide valuable information on the host disease susceptibility, microbial pathogenicity, and drug sensitivity. For urinary tract infections (UTI), NGS can reveal the pathogenic microbe and the dysbiosis of the urinary microbiome, which is a crucial factor in the pathogenesis of UTI and other urinary tract disorders. This review outlines the role of urinary microbiome dysbiosis in UTI, urinary stone disease, and cancer. Furthermore, the recent advances in NGS technologies for future applications in infectious disease research are described in detail.
-
Citations
Citations to this article as recorded by- Next-Generation Sequencing Supports Targeted Antibiotic Treatment for Culture Negative Orthopedic Infections
Ellie J C Goldstein, Ravina Kullar, Emanuele Chisari, James Snyder, Christopher Cooper, Javad Parvizi, Jason Sniffen
Clinical Infectious Diseases.2023; 76(2): 359. CrossRef
- Next-Generation Sequencing Supports Targeted Antibiotic Treatment for Culture Negative Orthopedic Infections
- 3,451 View
- 19 Download
- 1 Crossref

Original Articles
- Ureteral Stent Induced Urinary Tract Infection and Microbial Inconsistency Between Bladder and Renal Pelvis
- Useok Choi, Eun Jae Kim, Don Hee Lyu, Bong Hee Park, Hong Chung, Chang Hee Han, Sangrak Bae
- Urogenit Tract Infect 2021;16(3):61-66. Published online December 31, 2021
- DOI: https://doi.org/10.14777/uti.2021.16.3.61
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study examined the effects of long-term ureteral stent (US) on urinary tract infection (UTI) by bacterial migration and bacterial colonization.
Materials and Methods: From March 2014 to August 2021, 64 patients who underwent US for more than six months were enrolled in this study. When the US was inserted for the first time and replaced regularly, urine was collected from the bladder and renal pelvis and cultured. Patients’ the characteristics, and differences in pathogens related to US infection were analyzed.
Results: The mean age was 66.4 years, and the mean duration of indwelling was 37.5 months. There were 38 cases (59.3%) by malignant and 26 cases (40.6%) by benign causes. UTI occurred in 33 cases (53%); 16 cases (25%) were hospitalized for febrile UTI. After the initial US insertion, bacteria were identified in the bladder 285 days later and in the renal pelvis after 619 days. The bladder culture was positive in 10 of the 33 patients, and renal pelvis alone was positive in nine of the 33 patients. The same strain was confirmed in the bladder and renal pelvis in 12 cases (18.8%), and it took a mean of 5.8 months ± 6.32 (standard deviation) for the upward migration of bacteria.
Conclusions: UTIs occur in approximately 50% of patients with long-term US indwelling. The probability of culturing the same strain by a US was approximately 18.8%, and the role of pathogen transmission of a US does not appear to be significant. In addition, renal pelvis culture would be helpful in cases of failed bladder antibiotics susceptibility. -
Citations
Citations to this article as recorded by- Chemical Analysis and Antimicrobial Potential Assessment of Wild Laurel from the National Park Skadar Lake, Montenegro
Dragica Bojović, Miomir Šoškić, Ana Žugić, Marina T. Milenković, Iva Ljumović, Vanja M. Tadić
Applied Sciences.2025; 15(12): 6741. CrossRef - Comprehensive analysis of the bacterial spectrum for enhanced clinical insight in microbial ureteral stent colonization, uncomplicated urinary tract infections and catheter-associated urinary tract infections: a principal component analysis-based literatu
Matilde Lepori, Olivier Braissant, Gernot Bonkat, Malte Rieken
World Journal of Urology.2024;[Epub] CrossRef
- Chemical Analysis and Antimicrobial Potential Assessment of Wild Laurel from the National Park Skadar Lake, Montenegro
- 8,206 View
- 28 Download
- 2 Crossref

- Changes of Antimicrobial Resistance Causing Infections Following Transrectal Prostate Biopsy: Analysis of 10-Year Data
- Da Eun Han, Sun Tae Ahn, Jong Wook Kim, Du Geon Moon, Hong Seok Park, Mi Mi Oh
- Urogenit Tract Infect 2021;16(3):55-60. Published online December 31, 2021
- DOI: https://doi.org/10.14777/uti.2021.16.3.55
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: The production of extended-spectrum β-lactamases (ESBLs) has emerged as one of the main causes of antimicrobial resistance. It is well known that infections of ESBL-producing Enterobacteriaceae causes poor clinical outcomes. This study investigated the changes in the antimicrobial resistance patterns in infections following transrectal ultrasound-guided prostate (TR) biopsy over a 10 year period and analyzed whether the clinical course varies in infections caused by the ESBL-producing Enterobacteriaceae.
Materials and Methods: We retrospectively analyzed patients who had infections after a TR biopsy at the Korea University Guro Hospital from January 2010 to October 2019. Infection from a TR biopsy was defined as readmission due to a fever of 38 degrees or higher that occurred within one week after the biopsy.
Results: Among 1,855 patients who received a TR biopsy, 39 patients (2.10%) had infectious complications. Of 33 culture-positive patients, 29 patients (87.9%) showed quinolone resistance, 10 patients (30.3%) were ESBL-positive and 9 patients had concomitant quinolone resistance and were also ESBL-positive. 75% of ESBL-positive bacterial infections occurred after 2016 indicating increasing incidence in recent days. The only significant difference in the clinical course between the ESBL-negative and the positive group was the lower systolic blood pressure of the ESBL-positive group during hospitalization (p-value=0.018).
Conclusions: Infections due to the ESBL-producing Enterobacteriaceae showed a tendency to increase among TR biopsy patients since 2016. Although the clinical course of the ESBL-positive infection did not show significant differences to ESBL-negative infection, further analysis is needed because of the small number of patients.
- 2,006 View
- 6 Download

Reviews
- Virus in the Urine of Healthy People and Patients with Infectious Diseases
- Sunho Park, Eui Tae Kim, Jung-Sik Huh
- Urogenit Tract Infect 2021;16(2):44-48. Published online August 31, 2021
- DOI: https://doi.org/10.14777/uti.2021.16.2.44
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - There has been a sustained effort to overcome the multiple infectious diseases that confront humankind. Urinary tract infections (UTIs) are most commonly caused by bacterial pathogens, primarily Escherichia coli. However, UTIs by viral pathogens have not been significantly reported. The human urinary tract, both in the healthy and diseased states, is home to many viruses despite the traditional belief that urine is sterile in healthy individuals. The most common viral pathogens found in the urinary tract are the human polyomavirus (BK virus), adenovirus, cytomegalovirus, and herpes simplex virus type-1 and type-2. Research should continue to investigate whether these viruses cause clinical infections or are mere colonizers of the urinary tract. Keywords: Urinary tract
-
Citations
Citations to this article as recorded by- Unveiling indicator, enteric, and respiratory viruses in aircraft lavatory wastewater using adsorption-extraction and Nanotrap® Microbiome A Particles workflows
Warish Ahmed, Wendy J.M. Smith, Ananda Tiwari, Aaron Bivins, Stuart L. Simpson
Science of The Total Environment.2023; 896: 165007. CrossRef
- Unveiling indicator, enteric, and respiratory viruses in aircraft lavatory wastewater using adsorption-extraction and Nanotrap® Microbiome A Particles workflows
- 10,162 View
- 53 Download
- 1 Crossref

- A New Strategy for Elimination of Human Paplloma Virus-related Disease after Human Papillomavirus Vaccines Introduction
- Yoo-Jin Park, Tae-Hee Kim, Hae-Hyeog Lee, Jun-Mo Kim
- Urogenit Tract Infect 2020;15(3):63-70. Published online December 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.3.63
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Human papillomavirus (HPV) infections are the most common sexually transmitted diseases in male and female. The most common HPV types include HPV 6/11/16/18/31/33/45/52/58. Bivalent (bHPV), quadrivalent (qHPV), and nonavalent (nHPV) vaccines, have been developed worldwide to protect against HPV infections. This paper describes the worldwide trends in HPV infections after HPV vaccination and shows the progressive changes in national HPV vaccination programs toward gender-neutral vaccination (GNV). This review article is based on original and review articles on the HPV-associated disease burden and nationwide vaccination trends. In Korea, epidemiology studies have shown a decline in the incidence of cervical cancer from 16.3% (in 1999) to 9.1% (in 2015). Interestingly, based on the 2019 annual report from Korean Center for Disease Control, the incidence of anogenital warts increased in both sexes during 2014-2018 and was 2.6 times higher in male than female in 2018. These results indicate the good efficacy of HPV vaccinations against both diseases in female. Other studies suggest that GNV would almost eliminate the risks of HPV-associated diseases in most countries, compared to female-only vaccination. HPV vaccine coverage remains lower in male in Korea despite the vaccine efficacy in both sexes and the worldwide GNV trend. Scaling up HPV vaccination in both sexes should be encouraged. Furthermore, removing the HPV-attributable burden through nHPV vaccination could be considered, showing that HPV 31, 33, 45, 52, 58, which are not covered by bHPV and qHPV, are as prevalent as HPV 6, 11, 16, 18.
-
Citations
Citations to this article as recorded by- Changes in genital Human Papillomavirus (HPV) prevalence among urban females a decade after the Malaysian HPV vaccination program
Su Pei Khoo, Nor Adriana Muhammad Ridzuan Tan, Reena Rajasuriar, Nazrila Hairizan Nasir, Patti Gravitt, Chiu Wan Ng, Yin Ling Woo, Hoh Boon-Peng
PLOS ONE.2022; 17(12): e0278477. CrossRef
- Changes in genital Human Papillomavirus (HPV) prevalence among urban females a decade after the Malaysian HPV vaccination program
- 2,257 View
- 1 Download
- 1 Crossref

Case Report
- Seminal Vesicle Infection of Zinner Syndrome Misdiagnosed for Neoplasm
- Young Joo Kim
- Urogenit Tract Infect 2020;15(2):54-56. Published online August 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.2.54
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Zinner syndrome is a rare Müllerian duct congenital anomaly representing unilateral renal agenesis, ipsilateral seminal vesicle cyst, and ejaculatory duct obstruction. A 16-year-patient presented with dysuria, nocturia, and enduring diffuse perineal pain for two months. Radiologic studies revealed a right seminal vesicle cyst with a mass lesion and right renal agenesis. Ultrasonography guided transrectal biopsy indicated a seminal vesicle neoplasm. The mass was diagnosed as chronic inflammation. This paper reports a case of seminal vesicle inflammation associated with Zinner syndrome that was initially misdiagnosed as a neoplasm.
- 1,539 View
- 7 Download

Original Articles
- Performance of the Sysmex UF-1000i System in Screening for Significant Bacteriuria in Patients with Bladder Cancer Who Received Bacillus Calmette-Guérin Treatment
- Tae Hee Kim, Seung Il Jung, Myung Soo Kim, Hyun-Jung Choi, Ho Seok Chung, Eu Chang Hwang, Dong Deuk Kwon
- Urogenit Tract Infect 2020;15(2):38-46. Published online August 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.2.38
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: Diagnosing urinary tract infections by urine culture is time-consuming during a Bacillus Calmette-Guérin treatment. Because the urine culture results take time to collect, patients are treated presumptively, or Bacillus Calmette-Guérin is discontinued before the results. This study evaluated the ability of the Sysmex UF-1000i system to examine the urine bacterial count and determine if it could be used to predict a positive culture.
Materials and Methods: 180 patients who underwent transurethral resection for bladder tumors and received intravesical Bacillus Calmette-Guérin treatment between January 2017 and July 2018 were evaluated prospectively. For patients who received an intravesical Bacillus Calmette-Guérin treatment, urine flow cytometry, and urine cultures were assessed weekly during the treatment period.
Results: During Bacillus Calmette-Guérin instillation, 44, 146, and 27 patients had bacteriuria, pyuria, and positive urine nitrite, respectively. Multivariate analysis indicated that the predictors associated with bacteriuria included the urine flow cytometry results of >100 bacteria/µl (odds ratio, 22.73; p<0.001) and positive urine nitrite (odds ratio, 5.67; p=0.012) at the time of sampling for positive urine culture. The area under the receiver operative characteristic curve for diagnosing bacteriuria by urine flow cytometry was 0.825. A urine flow cytometry cutoff value of >100 bacteria/µl resulted in a sensitivity and specificity of 75% and 90.91%, respectively. Using the cutoff of >1,000 bacteria/µl, the sensitivity and specificity were 50% and 94.85%, respectively.
Conclusions: Rapid urinary tract infection diagnosis using Sysmex UF-1000i can be used to determine whether to treat an infection and to avoid unnecessary Bacillus Calmette-Guérin discontinuation and urine culture tests. -
Citations
Citations to this article as recorded by- Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
Ali Bourgi, Omar Ghanem, Camille Brocail, Franck Bruyère
Surgical Infections.2025; 26(6): 390. CrossRef
- Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
- 2,075 View
- 2 Download
- 1 Crossref

- Risk Factors of Febrile Urinary Tract Infection after Ureteral Reimplantation in Infant
- Seungsoo Lee, Jae Min Chung, Sang Don Lee
- Urogenit Tract Infect 2020;15(2):33-37. Published online August 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.2.33
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: Children with febrile urinary tract infection (fUTI) and vesicoureteral reflux (VUR) show significant morbidity. Few studies have examined the incidence of fUTI after ureteral reimplantation for congenital urinary tract anomalies, particularly in infants. Therefore, this study examined the incidence and risk factors of fUTI after ureteral reimplantation in infants.
Materials and Methods: Children under one year of age, who underwent ureteral reimplantation from July 2017 to December 2018, were reviewed retrospectively. The patients’ data were analyzed to evaluate the predictors of fUTI after ureteral reimplantation.
Results: Ureteral reimplantation was performed in 16 patients (25 ureters) at a mean of 8.9±2.8 months. The preoperative diagnosis was VUR 14 (87.5%), obstructive megaureter 1 (6.3%), duplicated ureter 1 (6.3%). Postoperative fUTI occurred in five patients (31.3%) during the follow-up period (average 9.6±5.9 months, range 3-18 months). UTI occurred at 40.8±16.6 (17-61) days after surgery. Fourteen ureters were implanted with a ureteral catheter for three days, and 11 ureters were implanted with a double J ureteral stent for six weeks. The children’s age, sex, surgical method, renal scar, reflux grade, laterality, persisting VUR, and presence of double J ureteral stent were not predictive factors for postoperative fUTI.
Conclusions: The incidence of fUTI after ureteral reimplantation in infants was 31.3%, and all fUTI occurred within two months after surgery. The risk factors associated with fUTI after ureteral reimplantation could not be predicted. -
Citations
Citations to this article as recorded by- Open vs. robot-assisted laparoscopic ureteral reimplantation in a contemporary pediatric cohort: a retrospective single-institution analysis
Suhaib Abdulfattah, Nicole J. Kye, Sanjay Aiyar, Emily Ai, Marina Quairoli, Meghan F. Davis, Karl Godlewski, Katherine Fischer, Christopher J. Long, Dana A. Weiss, Aseem R. Shukla, Arun K. Srinivasan, Sameer Mittal
Journal of Robotic Surgery.2026;[Epub] CrossRef - Etiological Agents of Urinary Tract Infection (UTI)
Rana Thamer Hadi Alkhafaji, M. Jayashankar
International Journal of Scientific Research in Science and Technology.2022; : 381. CrossRef
- Open vs. robot-assisted laparoscopic ureteral reimplantation in a contemporary pediatric cohort: a retrospective single-institution analysis
- 2,982 View
- 10 Download
- 2 Crossref


 KAUTII
KAUTII

 First
First Prev
Prev


