Abstract
Urinary tract infections (UTIs) are among the most prevalent bacterial infections worldwide, with uropathogenic Escherichia coli (UPEC) serving as the primary causative agent. Although antibiotic therapy remains the standard of care for UTI treatment, the increasing prevalence of antimicrobial resistance has substantially reduced the effectiveness of commonly prescribed antibiotics. Resistance to trimethoprim-sulfamethoxazole (TMP-SMX), β-lactams, and fluoroquinolones is particularly concerning, as these agents constitute the principal therapeutic options for UTIs. This review examines the molecular mechanisms underlying UPEC resistance to these three classes of antibiotics, including target site modifications, efflux pump overexpression, porin regulation, and enzymatic degradation. Furthermore, it explores how these resistance determinants contribute to the development of multidrug-resistant (MDR) UPEC strains, which demonstrate cross-resistance to multiple antibiotics and present significant challenges for clinical management. Novel therapeutic strategies, such as efflux pump inhibitors, bacteriophage therapy, and genomic-guided precision medicine, are under investigation as potential solutions to address the growing global burden of MDR UPEC, alongside alternative non-antibiotic treatments. This review aims to provide a comprehensive overview of the genetic and regulatory pathways driving antibiotic resistance in UPEC, offering insights that may guide the development of effective treatment strategies and help mitigate the ongoing spread of antimicrobial resistance.
-
Keywords: Uropathogenic Escherichia coli, Antibiotic resistance, Multidrug resistance, Urinary tract infections, Efflux pumps
HIGHLIGHTS
Uropathogenic Escherichia coli (UPEC) is the leading cause of urinary tract infections (UTIs) worldwide, and resistance to key antibiotics such as trimethoprim-sulfamethoxazole, β-lactams, and fluoroquinolones is rapidly increasing. This resistance is driven by mechanisms including target site mutations, efflux pump overexpression, porin regulation, and enzymatic degradation. These factors contribute to the emergence of multidrug-resistant (MDR) UPEC, posing major challenges to treatment. Novel therapeutic strategies, including efflux pump inhibitors, bacteriophage therapy, and precision medicine, are being explored. A deeper understanding of resistance pathways is essential for developing effective interventions and controlling the spread of MDR UPEC.
INTRODUCTION
Urinary tract infections (UTIs) are among the most prevalent bacterial infections in humans, with approximately 150 million cases annually and a high public and financial impact [
1]. Uropathogenic
Escherichia coli (UPEC) causes both uncomplicated and complicated UTIs, and its virulence and adaptability allow for survival in the urinary tract despite host immune defenses [
2,
3]. Currently, antibiotic therapy remains a first-line therapy for UTIs, but increased resistance to most antibiotics has limited therapeutic options [
4]. The most affected antibiotics include trimethoprim-sulfamethoxazole (TMP-SMX), β-lactams, and fluoroquinolones [
5]. Recent epidemiologic data reveal UPEC resistance to TMP-SMX between 14.6% and 60%, and resistance to fluoroquinolones >30% in most regions [
4,
6]. In addition, extended-spectrum β-lactamase (ESBL)-producing and carbapenem-resistant UPEC strains have compounded the issue, with such strains being resistant to nearly all β-lactam antibiotics, including carbapenems, which are considered a last-resort option [
7,
8].
UPEC exhibits multiple antibiotic resistance mechanisms, including target site modifications, enzymatic inactivation, porin modifications, and regulation of efflux pump activity [
9,
10]. These mechanisms, often encoded on mobile genetic elements (MEGs) contribute to the rapid spread of multidrug-resistant (MDR) strains, further complicating treatment strategies [
11-
13]. This review aims to provide a comprehensive overview of UPEC resistance mechanisms against TMP-SMX, β-lactams, and fluoroquinolones by emphasizing genetic mutations, and shared resistance determinants. Additionally, it explores how these mechanisms contribute to MDR UPEC emergence and persistence, emphasizing the urgent need for novel antimicrobial strategies. Understanding the molecular basis of UPEC resistance is crucial for developing targeted interventions that can mitigate resistance spread and improve UTI management in clinical settings.
PATHOGENICITY AND INFECTION MECHANISMS OF UPEC
UTIs caused by UPEC occur through a complex interplay between bacterial virulence factors and host immune processes [
3,
14]. UPEC utilizes various strategies for colonization of the urinary tract, evasion of immune processes, and establishment of persistent infection, which results in UTI recurrence and chronicity [
14,
15]. These pathogenic strategies not only complicate effective treatment but also highlight a necessity for new therapeutic interventions targeting bacterial persistence and immune evasion mechanisms [
3,
16,
17].
UPEC possesses various virulence factors that facilitate adhesion to host cells, nutrient acquisition, and immune system evasion, which contribute to bacterial survival and pathogenesis [
3,
18]. These include adhesins, toxins, and iron acquisition systems that act synergistically to allow bacterial survival in the urinary tract [
14,
19,
20].
A critical step in UPEC pathogenesis is the adherence to the urothelium, which is mediated by adhesion factors that enable bacterial colonization and invasion. Type 1 fimbriae (FimH), in particular, provides a crucial role in the initial attachment to bladder epithelial cells, allowing for bacterial invasion and establishment of intracellular bacterial communities (IBCs). FimH binds to mannosylated glycoproteins on bladder epithelial cells, promoting invasion and biofilm formation, contributing to recurrent UTIs. Biofilm formation creates a physical barrier that impedes antibiotic penetration, leading to insufficient drug concentrations in the deeper layers and allowing subpopulations of bacteria to remain unaffected. In contrast, adhesion in kidneys is facilitated through P fimbriae (PapG adhesin). P fimbriae recognize Gal(α1-4)Gal receptors on kidney epithelial cells, facilitating upper UTIs and pyelonephritis [
21,
22].
In addition to adhesion, UPEC produces toxins that disrupt host cell integrity and modulate immune responses.
Hemolysin (HlyA), a pore-forming transmembrane toxin, induces lysis of host cell, and evasion of the immune system [
23-
25]. Cytotoxic necrotizing factor 1 interferes with host cell signaling pathways, enhancing bacterial invasion and intracellular survival [
26,
27]. These virulence factors contribute to host tissue damage and bacterial survival within the urinary tract.
Furthermore, to overcome iron limitations in the urinary tract, UPEC utilizes high-affinity iron acquisition systems to compete against the host for iron. Siderophores such as enterobactin and aerobactin scavenge iron from host proteins to provides iron to support bacterial growth and virulence [
28]. The expression of these iron acquisition systems is tightly regulated in response to iron availability, allowing for UPEC to efficiently adapt to the host environment [
29].
The infection mechanism of UPEC is a coordinated cascade of events that enable bacterial colonization, immune evasion, and long-term persistence [
16]. Following initial adhesion via type 1 fimbriae, UPEC invades urothelial cells and forms IBCs, which develop biofilm-like aggregates that protect the bacterium from immune clearance and antibiotic treatment, leading to persistent and recurrent infections [
30-
32]. To further evade host immune responses, the modification of lipopolysaccharides reduces the efficacy of antimicrobial peptides and complement-mediated killing of bacteria, while the expression of a polysaccharide capsule inhibits phagocytosis by immune cells [
33,
34]. Additionally, UPEC secretes immune-modulating factors that interfere with neutrophil recruitment and cytokine signaling, further impairing host defenses [
17,
35].
As the infection progresses, some UPEC cells transition into a quiescent intracellular state, forming quiescent intracellular reservoirs within bladder epithelial cells. These dormant bacterial populations evade immune responses and antibiotic treatment, but reactivate under favorable conditions to cause recurrent infections [
36]. This cycle of dormancy and reactivation poses a significant therapeutic challenge, necessitating targeted strategies against persistent UPEC populations [
37,
38].
ANTIBIOTIC RESISTANCE MECHANISMS IN UPEC
1. TMP-SMX Resistance
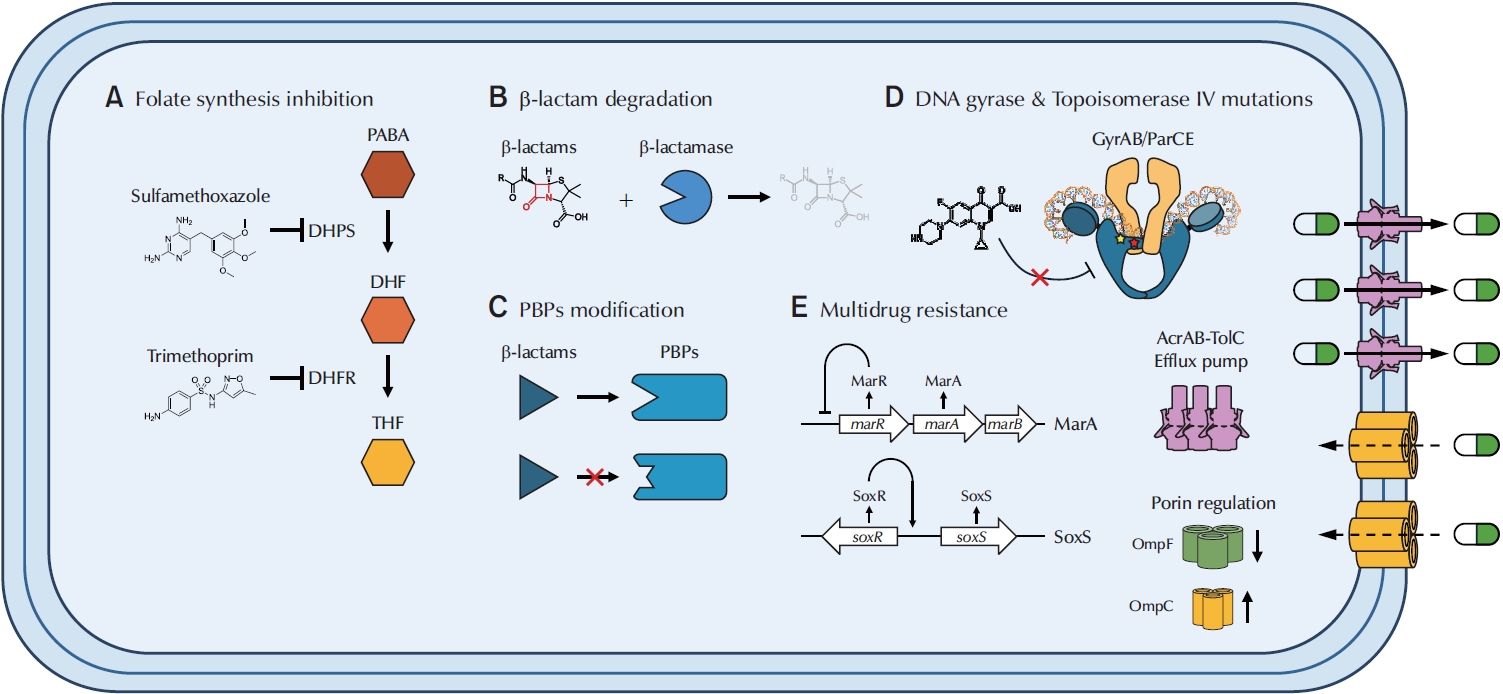
UPEC employs diverse molecular mechanisms to resist commonly prescribed antibiotics. The major strategies include enzymatic inactivation, target site modification, reduced membrane permeability, and efflux pump overexpression. These mechanisms compromise the efficacy of key antibiotic classes used to treat urinary tract infection, such as TMP-SMX, β-lactams, and fluoroquinolones (
Table 1).
TMP-SMX is a combination antibiotic that targets the bacterial folate synthesis pathway, which is essential for nucleotide biosynthesis and DNA replication (
Fig. 1) [
39]. Trimethoprim selectively inhibits dihydrofolate reductase (DHFR), preventing the reduction of dihydrofolate (DHF) to tetrahydrofolate (THF), a critical cofactor in DNA synthesis [
40]. Sulfamethoxazole inhibits dihydropteroate synthase (DHPS), an enzyme required for the biosynthesis of DHF. By synergistically disrupting folate metabolism, TMP-SMX exerts a strong bactericidal effect against
E. coli [
41]. Despite its long-standing clinical use, resistance to TMP-SMX has become increasingly prevalent among UPEC strains, reducing its efficacy in UTI treatment. Epidemiological studies report substantial regional variations in TMP-SMX resistance rates, with resistance levels ranging from 14.6% to 60%, posing a major challenge to empirical treatment strategies [
4]. In the United States, surveillance data from 2017 indicated that 32.1% of UPEC isolates were resistant to TMP-SMX, with resistance rates reaching up to 43.5% in certain regions [
6]. Furthermore, patients with recurrent UTIs or recent exposure to TMP-SMX exhibited a significantly higher risk of resistance [
42]. This increasing prevalence of TMP-SMX resistance has necessitated a reassessment of its role as a first-line treatment and stresses the urgent need for alternative therapeutic strategies.
The primary mechanism of TMP-SMX resistance involves the acquisition of plasmid-encoded resistance genes, encoding alternative forms of DHFR and DHPS with lowered affinities for TMP and SMX, respectively [
43]. The
dfrA and
sul gene families play a central role in this resistance, as
dfrA genes (e.g.,
dfrA1, dfrA5, dfrA12) encode trimethoprim-resistant DHFR variants that allow bacterial folate synthesis to continue despite TMP exposure, while
sul genes (
sul1, sul2, sul3) encode sulfamethoxazole-resistant DHPS enzymes, preventing SMX from inhibiting folate biosynthesis [
44,
45]. These genes are often carried on integrons and transposons, facilitating horizontal gene transfer and promoting their widespread dissemination among UPEC isolates [
46].
In addition to plasmid-mediated resistance, chromosomal mutations in endogenous
dhfr and
dhps genes have also been identified in TMP-SMX-resistant UPEC isolates. These mutations alter the three-dimensional structures of DHFR and DHPS, reducing drug-binding affinity while preserving enzymatic activity [
43,
47]. The combination of these resistance mechanisms allows UPEC to survive despite antibiotic exposure, increasing the adaptability of this pathogen in response to selective pressure.
Beta-lactam antibiotics inhibit penicillin-binding proteins (PBPs), which are important for bacterial cell wall synthesis. PBPs catalyze the cross-linking of peptidoglycan layers, a process necessary for maintaining cell wall integrity [
48]. By irreversibly binding to PBPs, β-lactams disrupt peptidoglycan synthesis, leading to cell lysis and bacterial death [
49]. However, UPEC has evolved multiple mechanisms to evade β-lactam activity, significantly reducing the efficiency of these antibiotics in UTI treatment.
A primary mechanism of β-lactam resistance in UPEC is the production of β-lactamases, enzymes that hydrolyze β-lactam antibiotics, rendering them ineffective. Among these, ESBLs, such as CTX-M type β-lactamase enzymes (named for their high level of activity against cefotaxime [CTX] and first observed in Münich [M]), TEM (named after a Greek patient, Temoneira, whose clinical samples yielded this gene), and SHV-type enzymes (originally reported in
Klebsiella pneumoniae clinical isolate and exhibit an overall preference for hydrolyzing sulfhydryl-containing cephalosporins [hence the SHV name]), confer resistance to a broad range of β-lactams, including third-generation cephalosporins and monobactams [
50-
53].
MEGs play a crucial role in the rapid dissemination of β-lactam resistance in UPEC. Plasmids carrying
blaCTX-M,
blaTEM, and
blaSHV facilitate horizontal gene transfer, promoting the cotransfer of multiple resistance determinants via integrons and transposons [
54]. This accumulation of resistance genes within a single UPEC strain reduces treatment efficacy and increases the risk of therapeutic failure. Additionally, AmpC β-lactamases, often plasmid-encoded, hydrolyze cephamycins and penicillins while evading inhibition by traditional β-lactamase inhibitors such as clavulanic acid [
55].
In addition to β-lactam degradation, mutations in PBPs also contribute to β-lactam resistance by reducing antibiotic binding affinity. Certain UPEC strains have mutations in both PBP2 and PBP3, leading to structural modifications that impair β-lactam binding, allowing for peptidoglycan synthesis even in the presence of antibiotics [
16,
56]. Another key mechanism involves the regulation of peptidoglycan remodeling, which enhances bacterial survival under β-lactam stress. Mutations in
nlpD, a regulator of peptidoglycan hydrolases, have been linked to modifications in cell wall integrity, reducing the impact of β-lactam antibiotics without compromising cell viability [
10,
57]. This ability to alter cell wall synthesis pathways allows UPEC to tolerate β-lactam exposure while maintaining structural stability. The combination of β-lactamase production, PBP modifications, and cell wall remodeling emphasizes the complexity of β-lactam resistance in UPEC. These mechanisms allow UPEC to persist despite β-lactam treatment, contributing to recurrent infections and therapeutic challenges.
Fluoroquinolones are broad-spectrum antibiotics that target DNA gyrase (
gyrA) and topoisomerase IV (
parC), essential enzymes for maintaining DNA supercoiling during bacterial replication. By inhibiting these enzymes, fluoroquinolones disrupt DNA replication, ultimately leading to bacterial cell death [
58]. However, UPEC has developed multiple resistance mechanisms that significantly reduce fluoroquinolone efficacy, contributing to treatment failure.
A primary mechanism of fluoroquinolone resistance is target site modification, which occurs via point mutations in the quinolone resistance-determining regions (QRDRs) of
gyrA and
parC. These mutations alter the structure of DNA gyrase and topoisomerase IV, reducing their binding affinity for fluoroquinolones. Among the most commonly observed mutations, S83L and D87N in
gyrA and S80I and E84K in
parC significantly impair fluoroquinolone binding, allowing bacterial replication to proceed despite antibiotic exposure [
59,
60]. Fluoroquinolone treatment can induce RecA-mediated activation of the LexA-controlled SOS response, increasing mutation rates in QRDRs and accelerating resistance development [
61].
In addition to target site modifications, plasmid-mediated quinolone resistance (PMQR) genes further promote UPEC survival under fluoroquinolone exposure. Genes such as
qnrA, qnrB, and
qnrS encode proteins that bind to DNA gyrase and topoisomerase IV, shielding them from fluoroquinolone inhibition [
62,
63]. Unlike chromosomal QRDR mutations, which alter enzyme structure, PMQR genes do not modify target enzymes but instead prevent fluoroquinolones from binding effectively [
64]. These genes are frequently located on conjugative plasmids, enabling horizontal gene transfer and facilitating the rapid dissemination of fluoroquinolone resistance among UPEC strains.
The presence of aminoglycoside acetyltransferase
AAC(6′)-Ib-cr, a PMQR gene embedded within a gene cassette or an integron, further provides an additional resistance mechanism by modifying fluoroquinolones through acetylation. Originally identified for its role in aminoglycoside resistance, AAC(6′)-Ib-cr can also reduce the activity of ciprofloxacin and norfloxacin, further diminishing fluoroquinolone efficacy [
65,
66]. This dual-resistance function enhances UPEC adaptability under antibiotic pressure, contributing to multidrug resistance. The combination of QRDR mutations, plasmid-mediated protection, and enzymatic drug modification underlines the complexity of fluoroquinolone resistance in UPEC, allowing the bacterium to persist despite fluoroquinolone treatment, leading to recurrent infections and limited therapeutic options.
The emergence of MDR UPEC poses a significant challenge in UTI treatment, as these strains exhibit resistance to multiple antibiotic classes, including the aforementioned β-lactams, fluoroquinolones, and TMP-SMX. A recent experimental evolution studies on ampicillin-resistant UPEC has demonstrated that resistance to a single β-lactam antibiotic can rapidly extend to multiple drug classes, including ciprofloxacin, tetracycline, and chloramphenicol [
10]. This phenomenon is primarily driven by mutations in global regulators such as
marR (V66F),
acrR, and
envZ (T402M), which collectively lead to AcrAB-TolC efflux pump overexpression, differential regulation of porin proteins (OmpF loss and OmpC increase), and reduced membrane permeability, thus facilitating cross-resistance to unrelated antibiotics. Efflux pump overexpression and porin modifications play central roles in conferring MDR in UPEC strains [
10,
67,
68]. Among these, the AcrAB-TolC efflux system is a key contributor to MDR phenotypes. This tripartite resistance-nodulation-division pump actively expels fluoroquinolones, β-lactams, and TMP-SMX, lowering intracellular antibiotic concentrations and reducing drug efficacy. Mutations in
marR, acrR, and
soxS disrupt efflux pump repression, leading to constitutive overexpression of AcrAB-TolC [
10]. Additionally, overexpression of MdtK, a member of the major facilitator superfamily, has been linked to enhanced fluoroquinolone resistance in MDR UPEC isolates [
69].
Alongside efflux-mediated drug extrusion, porin downregulation and structural modifications significantly contribute to MDR. The loss or mutation of outer membrane porins, particularly OmpF and OmpC, restricts antibiotic influx, thereby lowering intracellular drug concentrations [
70]. These changes are often regulated by the EnvZ-OmpR 2-component system, which modulates porin expression in response to environmental stressors [
10]. The combination of increased efflux activity and reduced membrane permeability creates an impermeable bacterial barrier, reinforcing MDR phenotypes and limiting the efficacy of multiple antibiotic classes [
10].
CLINICAL IMPLICATIONS
MDR UPEC poses a significant challenge in the treatment of UTIs, leading to an increase in treatment failures and recurring infections. Standard first-line antibiotics, including fluoroquinolones and TMP-SMX, are losing effectiveness due to escalating resistance rates, necessitating frequent modifications to clinical guidelines [
4]. This widespread resistance to first-line antibiotics limits therapeutic options, often necessitating the use of last-resort antibiotics such as carbapenems [
71]. However, the rise of carbapenem-resistant UPEC strains further complicates treatment strategies and increases the burden on healthcare systems [
72]. Similarly, novel β-lactamase inhibitors (e.g., avibactam and vaborbactam) are being developed to combat ESBL- and AmpC-producing UPEC strains [
73,
74]. In regions where TMP-SMX resistance exceeds 20%, alternative agents such as nitrofurantoin and fosfomycin are recommended [
75,
76].
Efflux pump overexpression plays a major role in MDR UPEC, significantly reducing the efficacy of multiple antibiotic classes. Given this challenge, clinical strategies must focus on novel approaches such as efflux pump inhibitors (EPIs) and alternative treatment methods. The use of EPIs, such as PAβN and D13-9001, is a potential strategy for enhancing therapeutic efficacy [
77,
78]. While EPIs have shown promise in restoring antibiotic susceptibility, their clinical application remains limited due to concerns regarding toxicity and pharmacokinetics. Further research is needed to develop safer and more effective inhibitors for use as adjunct therapies in MDR UPEC treatment.
Despite ongoing research efforts, UTI treatment remains challenging due to the formation of biofilms and quiescent intracellular reservoirs within bladder epithelial cells. These bacterial populations evade immune defenses and are protected from antibiotic exposure, making complete eradication difficult [
79]. Moreover, biofilm-associated UPEC strains demonstrate heightened tolerance to multiple antibiotics, further contributing to chronic and recurrent infections [
36]. Therefore, alternative treatment strategies and early diagnosis are crucial alongside antibiotic therapy. Bacteriophage therapy and immunomodulatory treatments are currently being explored as potential non-antibiotic approaches for combating MDR UPEC [
80]. A study published in 2024 demonstrated the effectiveness of using lytic phages belonging to the
Tequatrovirus genus to kill MDR
E. coli in vivo [
81]. Utilizing mouse models, the study reported that mice infected with
E. coli ST131 were able to survive when treated with isolated phage cocktails. However, the current state of bacteriophage therapy and immunomodulatory treatments is still undergoing extensive testing, and it remains too early to draw definitive conclusions or determine the efficacy of other alternative therapeutic strategies for combating MDR UPEC.
The continued evolution of MDR UPEC highlights the urgent need for genomic surveillance and antimicrobial stewardship programs to track resistance trends and guide evidence-based treatment decisions [
82]. Rapid molecular diagnostics, such as whole-genome sequencing and polymerase chain reaction-based resistance profiling, hold promise for more precise and personalized antibiotic selection, ultimately improving patient outcomes [
83]. A comprehensive approach that incorporates novel therapeutics, advanced diagnostics, and robust infection control measures will be essential in mitigating the global public health impact of MDR UPEC.
CONCLUSIONS
UTIs remain one of the most common bacterial infections worldwide, yet their treatment is becoming increasingly difficult due to the rapid emergence of MDR UPEC [
1,
6,
12]. As highlighted previously, resistance to first-line antibiotics such as β-lactams, fluoroquinolones, and TMP-SMX has severely limited therapeutic options, leading to higher recurrence rates and increased healthcare burdens. This review has covered the key mechanisms underlying UPEC resistance to β-lactams, fluoroquinolones, and TMP-SMX, including mutations in target enzymes, overexpression of efflux pumps, and horizontal gene transfer of resistance determinants [
9-
11]. Resistance to a single antibiotic, such as ampicillin, can readily extend to multiple drug classes through mutations affecting global regulators (
marR, acrR, envZ), resulting in efflux pump overexpression, porin downregulation, and reduced membrane permeability [
10,
67,
68], all of which collectively contribute to a shared mechanism of MDR to structurally unrelated antibiotics. Given these findings, addressing MDR UPEC infections requires a multifaceted approach, including the potential use of EPIs as adjunctive therapies to restore antibiotic efficacy [
77,
78], along with rapid molecular diagnostics and resistance surveillance. A proactive, evidence-based approach to antibiotic use and resistance monitoring will be critical in controlling the spread of MDR UPEC and improving clinical outcomes for UTI patients. Combination therapies and immunomodulatory treatments should be further explored to improve UTI management.
NOTES
-
Funding/Support
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) [NRF-2022R1A2B5B02002256, NRF-2022R1A4A1025913, and NRF-2020M3A9H5104235 to E.-J.L.].
-
Conflict of Interest
The authors have nothing to disclose.
-
Author Contribution
Conceptualization: EJL; Data curation: NC, DUK; Writing - original draft: EJL, NC; Writing - review & editing: EJL, DUK.
Fig. 1.Mechanisms of antibiotics resistance (TMP-SMX, β-lactams, and fluoroquinolones) and multidrug resistance in UPEC. (A) TMP-SMX inhibits folate synthesis by blocking both DHPS and DHFR, preventing the conversion of PABA into DHF and ultimately inhibiting the reduction of DHF into THF, the active form of folate. (B) Beta-lactamases recognize and bind to the β-lactam ring of antibiotics, hydrolyzing the ring and converting it into a linear, inactive structure. (C) Point mutations in native pbp genes reduce β-lactam binding affinity, rendering antibiotics ineffective. Horizontal gene transfer of novel pbp genes can also decrease β-lactam efficacy. (D) Mutations in gyrA and gyrB alter fluoroquinolone-binding pockets in DNA gyrase, reducing drug affinity. Similarly, mutations in parC and parE modify binding sites in topoisomerase IV. (E) MarA and SoxS upregulate the AcrAB-TolC efflux system, actively pumping antibiotics out of the cell. They also downregulate expression of OmpF, a large outer membrane porin, thereby reducing antibiotic influx, while OmpC, which forms a smaller pore, is upregulated. Under normal conditions, MarR represses the marA operon; however, mutations can abolish this repression. SoxS is activated by SoxR, which may become constitutively active even in the absence of oxidative stress. TMP-SMX, trimethoprim-sulfamethoxazole; UPEC, uropathogenic Escherichia coli; DHPS, dihydropteroate synthase; DHFR, dihydrofolate reductase; PABA, para-aminobenzoic acid; DHF, dihydrofolate; THF, tetrahydrofolate; PBP, penicillin-binding protein.

Table 1.Major antibiotic resistance mechanisms in uropathogenic Escherichia coli
|
Antibiotic class |
Target |
Resistance mechanisms |
References |
|
Trimethoprim-sulfamethoxazole |
Dihydrofolate reductase & dihydropteroate synthase |
Plasmid-encoded dfrA and sul genes; mutations in endogenous dhfr and dhps genes |
[44,45] |
|
β-Lactams |
Penicillin-binding proteins (PBPs) |
β-lactamase production; mutations in PBPs; peptidoglycan remodeling |
[48,49] |
|
Fluoroquinolones |
DNA gyrase & topoisomerase IV |
QRDR mutations in gyrA and parC; plasmid-mediated qnr genes (qnrA, qnrB, qnrS) |
[59,60,62,63] |
REFERENCES
- 1. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 2015;13:269-84.ArticlePubMedPMCPDF
- 2. Torres-Puig S, García V, Stærk K, Andersen TE, Møller-Jensen J, Olsen JE, et al. “Omics” technologies-what have they told us about uropathogenic Escherichia coli fitness and virulence during urinary tract infection? Front Cell Infect Microbiol 2022;12:824039.ArticlePubMedPMC
- 3. Bien J, Sokolova O, Bozko P. Role of uropathogenic Escherichia coli virulence factors in development of urinary tract infection and kidney damage. Int J Nephrol 2012;2012:681473.ArticlePubMedPMCPDF
- 4. Kot B. Antibiotic resistance among uropathogenic. Pol J Microbiol 2019;68:403-15.PubMedPMC
- 5. Mehnert-Kay SA. Diagnosis and management of uncomplicated urinary tract infections. Am Fam Physician 2005;72:451-6.PubMed
- 6. Critchley IA, Cotroneo N, Pucci MJ, Mendes R. The burden of antimicrobial resistance among urinary tract isolates of Escherichia coli in the United States in 2017. PLoS One 2019;14:e0220265.ArticlePubMedPMC
- 7. Grome HN, Grass JE, Duffy N, Bulens SN, Ansari U, Campbell D, et al. Carbapenem-resistant and extended-spectrum β-lactamase-producing enterobacterales in children, United States, 2016-2020. Emerg Infect Dis 2024;30:1104.ArticlePubMedPMC
- 8. Husna A, Rahman MM, Badruzzaman A, Sikder MH, Islam MR, Rahman MT, et al. Extended-spectrum β-lactamases (ESBL): challenges and opportunities. Biomedicines 2023;11:2937.ArticlePubMedPMC
- 9. Nasrollahian S, Graham JP, Halaji M. A review of the mechanisms that confer antibiotic resistance in pathotypes of E. coli. Front Cell Infect Microbiol 2024;14:1387497.ArticlePubMedPMC
- 10. Choi N, Choi E, Cho YJ, Kim MJ, Choi HW, Lee EJ. A shared mechanism of multidrug resistance in laboratory-evolved uropathogenic Escherichia coli. Virulence 2024;15:2367648.ArticlePubMedPMC
- 11. Sun D, Jeannot K, Xiao Y, Knapp CW. Editorial: horizontal gene transfer mediated bacterial antibiotic resistance. Front Microbiol 2019;10:1933.ArticlePubMedPMC
- 12. Ramírez-Castillo FY, Moreno-Flores AC, Avelar-González FJ, Márquez-Díaz F, Harel J, Guerrero-Barrera AL. An evaluation of multidrug-resistant Escherichia coli isolates in urinary tract infections from Aguascalientes, Mexico: cross-sectional study. Ann Clin Microbiol Antimicrob 2018;17:1-13.PubMedPMC
- 13. Rozwadowski M, Gawel D. Molecular factors and mechanisms driving multidrug resistance in uropathogenic Escherichia coli—an update. Genes 2022;13:1397.ArticlePubMedPMC
- 14. Terlizzi ME, Gribaudo G, Maffei ME. UroPathogenic Escherichia coli (UPEC) infections: virulence factors, bladder responses, antibiotic, and non-antibiotic antimicrobial strategies. Front Microbiol 2017;8:1566.ArticlePubMedPMC
- 15. Zhou Y, Zhou Z, Zheng L, Gong Z, Li Y, Jin Y, et al. Urinary tract infections caused by uropathogenic Escherichia coli: mechanisms of infection and treatment options. Int J Mol Sci 2023;24:10537.ArticlePubMedPMC
- 16. Whelan S, Lucey B, Finn K. Uropathogenic Escherichia coli (UPEC)-associated urinary tract infections: the molecular basis for challenges to effective treatment. Microorganisms 2023;11:2169.ArticlePubMedPMC
- 17. Olson PD, Hunstad DA. Subversion of host innate immunity by uropathogenic Escherichia coli. Pathogens 2016;5:2.ArticlePubMedPMC
- 18. Subashchandrabose S, Mobley HL. Virulence and fitness determinants of uropathogenic Escherichia coli. In: Mulvey MA, Klumpp DJ, Stapleton AE, editors. Urinary tract infections: molecular pathogenesis and clinical management. Washington, DC; ASM Press; 2017. p. 235-61.
- 19. Frick-Cheng AE, Sintsova A, Smith SN, Pirani A, Snitkin ES, Mobley HL. Ferric citrate uptake is a virulence factor in uropathogenic Escherichia coli. mBio 2022;13:e0103522.ArticlePubMedPMCPDF
- 20. Nielubowicz GR, Mobley HL. Host-pathogen interactions in urinary tract infection. Nat Rev Urol 2010;7:430-41.ArticlePubMedPDF
- 21. Roberts JA, Marklund BI, Ilver D, Haslam D, Kaack MB, Baskin G, et al. The Gal (alpha 1-4) Gal-specific tip adhesin of Escherichia coli P-fimbriae is needed for pyelonephritis to occur in the normal urinary tract. Proc Natl Acad Sci U S A 1994;91:11889-93.ArticlePubMedPMC
- 22. Melican K, Sandoval RM, Kader A, Josefsson L, Tanner GA, Molitoris BA, et al. Uropathogenic Escherichia coli P and Type 1 fimbriae act in synergy in a living host to facilitate renal colonization leading to nephron obstruction. PLoS Pathog 2011;7:e1001298.ArticlePubMedPMC
- 23. Dhakal BK, Mulvey MA. The UPEC pore-forming toxin α-hemolysin triggers proteolysis of host proteins to disrupt cell adhesion, inflammatory, and survival pathways. Cell Host Microbe 2012;11:58-69.ArticlePubMedPMC
- 24. Nagamatsu K, Hannan TJ, Guest RL, Kostakioti M, Hadjifrangiskou M, Binkley J, et al. Dysregulation of Escherichia coli α-hemolysin expression alters the course of acute and persistent urinary tract infection. Proc Natl Acad Sci U S A 2015;112:E871-80.ArticlePubMedPMC
- 25. Naskar M, Parekh VP, Abraham MA, Alibasic Z, Kim MJ, Suk G, et al. α-Hemolysin promotes uropathogenic E. coli persistence in bladder epithelial cells via abrogating bacteria-harboring lysosome acidification. PLoS Pathog 2023;19:e1011388.ArticlePubMedPMC
- 26. Fabbri A, Travaglione S, Fiorentini C. Escherichia coli cytotoxic necrotizing factor 1 (CNF1): toxin biology, in vivo applications and therapeutic potential. Toxins 2010;2:283-96.ArticlePubMedPMC
- 27. Sun X, Yang J, Deng X, Wei Y, Wang C, Guo Y, et al. Interactions of bacterial toxin CNF1 and Host JAK1/2 driven by liquid-liquid phase separation enhance macrophage polarization. mBio 2022;13:e0114722.ArticlePubMedPMCPDF
- 28. Garcia EC, Brumbaugh AR, Mobley HL. Redundancy and specificity of Escherichia coli iron acquisition systems during urinary tract infection. Infect Immun 2011;79:1225-35.ArticlePubMedPMCPDF
- 29. Robinson AE, Heffernan JR, Henderson JP. The iron hand of uropathogenic Escherichia coli: the role of transition metal control in virulence. Future Microbiol 2018;13:745-56.ArticlePubMedPMC
- 30. Stærk K, Khandige S, Kolmos HJ, Møller-Jensen J, Andersen TE. Uropathogenic Escherichia coli express type 1 fimbriae only in surface adherent populations under physiological growth conditions. J Infect Dis 2016;213:386-94.ArticlePubMed
- 31. Mulvey MA, Schilling JD, Martinez JJ, Hultgren SJ. Bad bugs and beleaguered bladders: interplay between uropathogenic Escherichia coli and innate host defenses. Proc Natl Acad Sci U S A 2000;97:8829-35.ArticlePubMedPMC
- 32. Lewis AJ, Richards AC, Mulvey MA. Invasion of host cells and tissues by uropathogenic bacteria. In: Mulvey MA, Klumpp DJ, Stapleton AE, editors. Urinary tract infections: molecular pathogenesis and clinical management. Washington, DC; ASM Press; 2017. p. 359-81.
- 33. Needham BD, Trent MS. Fortifying the barrier: the impact of lipid A remodelling on bacterial pathogenesis. Nat Rev Microbiol 2013;11:467-81.ArticlePubMedPMCPDF
- 34. Sarkar S, Ulett GC, Totsika M, Phan MD, Schembri MA. Role of capsule and O antigen in the virulence of uropathogenic Escherichia coli. PLoS One 2014;9:e94786.ArticlePubMedPMC
- 35. Billips BK, Schaeffer AJ, Klumpp DJ. Molecular basis of uropathogenic Escherichia coli evasion of the innate immune response in the bladder. Infect Immun 2008;76:3891-900.ArticlePubMedPMCPDF
- 36. Mulvey MA, Schilling JD, Hultgren SJ. Establishment of a persistent Escherichia coli reservoir during the acute phase of a bladder infection. Infect Immun 2001;69:4572-9.ArticlePubMedPMCPDF
- 37. Blango MG, Ott EM, Erman A, Veranic P, Mulvey MA. Forced resurgence and targeting of intracellular uropathogenic Escherichia coli reservoirs. PLoS One 2014;9:e93327.ArticlePubMedPMC
- 38. Mysorekar IU, Hultgren SJ. Mechanisms of uropathogenic Escherichia coli persistence and eradication from the urinary tract. Proc Natl Acad Sci U S A 2006;103:14170-5.ArticlePubMedPMC
- 39. Minato Y, Dawadi S, Kordus SL, Sivanandam A, Aldrich CC, Baughn AD. Mutual potentiation drives synergy between trimethoprim and sulfamethoxazole. Nat Commun 2018;9:1003.ArticlePubMedPMCPDF
- 40. Gleckman R, Blagg N, Joubert DW. Trimethoprim: mechanisms of action, antimicrobial activity, bacterial resistance, pharmacokinetics, adverse reactions, and therapeutic indications. Pharmacotherapy 1981;1:14-20.ArticlePubMedPDF
- 41. Masters PA, O'Bryan TA, Zurlo J, Miller DQ, Joshi N. Trimethoprim-sulfamethoxazole revisited. Arch Intern Med 2003;163:402-10.ArticlePubMed
- 42. Wesolek JL, Wu JY, Smalley CM, Wang L, Campbell MJ. Risk factors for trimethoprim and sulfamethoxazole-resistant Escherichia coli in ED patients with urinary tract infections. Am J Emerg Med 2022;56:178-82.ArticlePubMed
- 43. Nolan LK, Li G, Logue CM. Origin and dissemination of antimicrobial resistance among uropathogenic Escherichia coli. In: Mulvey MA, Klumpp DJ, Stapleton AE, editors. Urinary tract infections: molecular pathogenesis and clinical management. Washington, DC; ASM Press; 2017. p. 179-205.
- 44. Sköld O. Resistance to trimethoprim and sulfonamides. Vet Res 2001;32:261-73.ArticlePubMed
- 45. Kirby WM, Corpron DO, Tanner DC. Urinary tract infections caused by antibiotic-resistant coliform bacilli. J Am Med Assoc 1956;162:1-4.ArticlePubMed
- 46. Poey ME, de los Santos E, Aznarez D, García-Laviña CX, Laviña M. Genetics of resistance to trimethoprim in cotrimoxazole resistant uropathogenic Escherichia coli: integrons, transposons, and single gene cassettes. Front Microbiol 2024;15:1395953.ArticlePubMedPMC
- 47. Estrada A, Wright DL, Anderson AC. Antibacterial antifolates: from development through resistance to the next generation. Cold Spring Harb Perspect Med 2016;6:a028324.ArticlePubMedPMC
- 48. Sauvage E, Kerff F, Terrak M, Ayala JA, Charlier P. The penicillin-binding proteins: structure and role in peptidoglycan biosynthesis. FEMS Microbiol Rev 2008;32:234-58.ArticlePubMed
- 49. Edoo Z, Arthur M, Hugonnet JE. Reversible inactivation of a peptidoglycan transpeptidase by a β-lactam antibiotic mediated by β-lactam-ring recyclization in the enzyme active site. Sci Rep 2017;7:9136.ArticlePubMedPMCPDF
- 50. Bajpai T, Pandey M, Varma M, Bhatambare G. Prevalence of TEM, SHV, and CTX-M Beta-Lactamase genes in the urinary isolates of a tertiary care hospital. Avicenna J Med 2017;7:12-6.ArticlePubMedPMC
- 51. Copur Cicek A, Saral A, Ozad Duzgun A, Yasar E, Cizmeci Z, Ozlem Balci P, et al. Nationwide study of Escherichia coli producing extended-spectrum β-lactamases TEM, SHV and CTX-M in Turkey. J Antibiot (Tokyo) 2013;66:647-50.ArticlePubMedPDF
- 52. Gniadkowski M. Evolution of extended-spectrum beta-lactamases by mutation. Clin Microbiol Infect 2008;14 Suppl 1:11-32.PubMed
- 53. Hussain HI, Aqib AI, Seleem MN, Shabbir MA, Hao H, Iqbal Z, et al. Genetic basis of molecular mechanisms in beta-lactam resistant gram-negative bacteria. Microb Pathog 2021;158:105040.PubMedPMC
- 54. Alipour M, Jafari A. Evaluation of the prevalence of blaSHV, blaTEM, and blaCTX Genes in Escherichia coli isolated from urinary tract infections. Avicenna J Clin Microbiol Infect 2019;6:83-7.ArticlePDF
- 55. Sadeghi M, Ebrahim-Saraie HS, Mojtahedi A. Prevalence of ESBL and AmpC genes in E. coli isolates from urinary tract infections in the north of Iran. New Microbes New Infect 2021;45:100947.ArticlePubMedPMC
- 56. Issakhanian L, Behzadi P. Antimicrobial agents and urinary tract infections. Curr Pharm Des 2019;25:1409-23.ArticlePubMed
- 57. Tsang MJ, Yakhnina AA, Bernhardt TG. NlpD links cell wall remodeling and outer membrane invagination during cytokinesis in Escherichia coli. PLoS Genet 2017;13:e1006888.ArticlePubMedPMC
- 58. Hooper DC, Jacoby GA. Topoisomerase inhibitors: fluoroquinolone mechanisms of action and resistance. Cold Spring Harb Perspect Med 2016;6:a025320.ArticlePubMedPMC
- 59. Bagel S, Hüllen V, Wiedemann B, Heisig P. Impact of gyrA and parC mutations on quinolone resistance, doubling time, and supercoiling degree of Escherichia coli. Antimicrob Agents Chemother 1999;43:868-75.ArticlePubMedPMCPDF
- 60. Sorlozano A, Gutierrez J, Jimenez A, de Dios Luna J, Martínez JL. Contribution of a new mutation in parE to quinolone resistance in extended-spectrum-β-lactamase-producing Escherichia coli isolates. J Clin Microbiol 2007;45:2740-2.ArticlePubMedPMCPDF
- 61. Recacha E, Machuca J, Díaz de Alba P, Ramos-Güelfo M, Docobo-Pérez F, Rodriguez-Beltrán J, et al. Quinolone resistance reversion by targeting the SOS response. mBio 2017;8:e00971-17.ArticlePubMedPMCPDF
- 62. Jacoby GA, Strahilevitz J, Hooper DC. Plasmid-mediated quinolone resistance. In: Tolmasky ME, Alonso JC, editors. Plasmids: biology and impact in biotechnology and discovery. Washington, DC; ASM Press; 2015. p. 475-503.ArticlePubMed
- 63. Rezazadeh M, Baghchesaraei H, Peymani A. Plasmid-mediated quinolone-resistance (qnr) genes in clinical isolates of Escherichia coli collected from several hospitals of Qazvin and Zanjan Provinces, Iran. Osong Public Health Res Perspect 2016;7:307-12.ArticlePubMedPMC
- 64. Tran JH, Jacoby GA. Mechanism of plasmid-mediated quinolone resistance. Proc Natl Acad Sci U S A 2002;99:5638-42.ArticlePubMedPMC
- 65. Whelan S, Bottacini F, Buttimer C, Finn K, Lucey B. Whole genome sequencing of uropathogenic E. coli from Ireland reveals diverse resistance mechanisms and strong correlation with phenotypic (EUCAST) susceptibility testing. Infect Genet Evol 2024;121:105600.ArticlePubMed
- 66. Morgan-Linnell SK, Becnel Boyd L, Steffen D, Zechiedrich L. Mechanisms accounting for fluoroquinolone resistance in Escherichia coli clinical isolates. Antimicrob Agents Chemother 2009;53:235-41.ArticlePubMedPMCPDF
- 67. Rijavec M, Erjavec MS, Avguštin JA, Reissbrodt R, Fruth A, Križan-Hergouth V, et al. High prevalence of multidrug resistance and random distribution of mobile genetic elements among uropathogenic Escherichia coli (UPEC) of the four major phylogenetic groups. Curr Microbiol 2006;53:158-62.ArticlePubMedPDF
- 68. Ganjo AR, Balaky STJ, Mawlood AH, Smail SB, Shabila NP. Characterization of genes related to the efflux pump and porin in multidrug-resistant Escherichia coli strains isolated from patients with COVID-19 after secondary infection. BMC Microbiol 2024;24:122.ArticlePubMedPMCPDF
- 69. Pietsch F, Bergman JM, Brandis G, Marcusson LL, Zorzet A, Huseby DL, et al. Ciprofloxacin selects for RNA polymerase mutations with pleiotropic antibiotic resistance effects. J Antimicrob Chemother 2016;72:75-84.ArticlePubMed
- 70. Choi U, Lee CR. Distinct roles of outer membrane porins in antibiotic resistance and membrane integrity in Escherichia coli. Front Microbiol 2019;10:953.ArticlePubMedPMC
- 71. Park KS, Kim DR, Baek JY, Shin A, Kim KR, Park H, et al. Susceptibility to Fosfomycin and Nitrofurantoin of ESBL-Positive Escherichia coli and Klebsiella pneumoniae isolated from urine of pediatric patients. J Korean Med Sci 2023;38:e361.ArticlePubMedPMCPDF
- 72. Walker MM, Roberts JA, Rogers BA, Harris PN, Sime FB. Current and emerging treatment options for multidrug resistant Escherichia coli urosepsis: a review. Antibiotics 2022;11:1821.ArticlePubMedPMC
- 73. Lin LY, Debabov D, Chang W, Stone G, Riccobene T. Antimicrobial activity of ceftazidime-avibactam and comparators against pathogens harboring OXA-48 and AmpC alone or in combination with other β-lactamases collected from Phase 3 clinical trials and an international surveillance program. Antimicrob Agents Chemother 2022;66:e01985-21.ArticlePubMedPMCPDF
- 74. Pogue JM, Bonomo RA, Kaye KS. Ceftazidime/avibactam, meropenem/vaborbactam, or both? Clinical and formulary considerations. Clin Infect Dis 2019;68:519-24.ArticlePubMed
- 75. Gupta K, Hooton TM, Roberts PL, Stamm WE. Short-course nitrofurantoin for the treatment of acute uncomplicated cystitis in women. Arch Inter Med 2007;167:2207-12.ArticlePubMed
- 76. Maraki S, Samonis G, Rafailidis PI, Vouloumanou EK, Mavromanolakis E, Falagas ME. Susceptibility of urinary tract bacteria to fosfomycin. Antimicrob Agents Chemother 2009;53:4508-10.ArticlePubMedPMCPDF
- 77. Byrd BA, Zenick B, Rocha-Granados MC, Englander HE, Hare PJ, LaGree TJ, et al. The AcrAB-TolC efflux pump impacts persistence and resistance development in stationary-phase Escherichia coli following delafloxacin treatment. Antimicrob Agents Chemother 2021;65:e0028121.ArticlePubMedPMCPDF
- 78. Kavanaugh LG, Dey D, Shafer WM, Conn GL. Structural and functional diversity of Resistance-Nodulation-Division (RND) efflux pump transporters with implications for antimicrobial resistance. Microbiol Mol Biol Rev 2024;88:e00089-23.ArticlePubMedPDF
- 79. Jacobsen S, Stickler DJ, Mobley HL, Shirtliff M. Complicated catheter-associated urinary tract infections due to Escherichia coli and Proteus mirabilis. Clinl Microbiol Rev 2008;21:26-59.ArticlePubMedPMCPDF
- 80. Zalewska-Piątek B, Piątek R. Phage therapy as a novel strategy in the treatment of urinary tract infections caused by E. coli. Antibiotics 2020;9:304.ArticlePubMedPMC
- 81. Shamsuzzaman M, Kim S, Kim J. Bacteriophage as a novel therapeutic approach for killing multidrug-resistant Escherichia coli ST131 clone. Front Microbiol 2024;15:1455710.ArticlePubMedPMC
- 82. El Chaar M, Khoury Y, Douglas GM, El Kazzi S, Jisr T, Soussi S, et al. Longitudinal genomic surveillance of multidrug-resistant Escherichia coli carriage in critical care patients. Microbiol Spectr 2024;12:e03128-3.PubMedPMC
- 83. Bonvegna M, Tomassone L, Christensen H, Olsen JE. Whole genome sequencing (WGS) analysis of virulence and AMR genes in extended-spectrum β-lactamase (ESBL)-producing Escherichia coli from animal and environmental samples in four Italian swine farms. Antibiotics 2022;11:1774.ArticlePubMedPMC
 , Dong Uk Kim
, Dong Uk Kim , Eun-Jin Lee
, Eun-Jin Lee



 KAUTII
KAUTII
 Cite
Cite

