-
Mortality and Risk Factors for Emphysematous Pyelonephritis in Korea: A Multicenter Retrospective Cohort Study
-
Seung-Kwon Choi, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2025;20(1):34-41. Published online April 30, 2025
-
DOI: https://doi.org/10.14777/uti.2550006003
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose
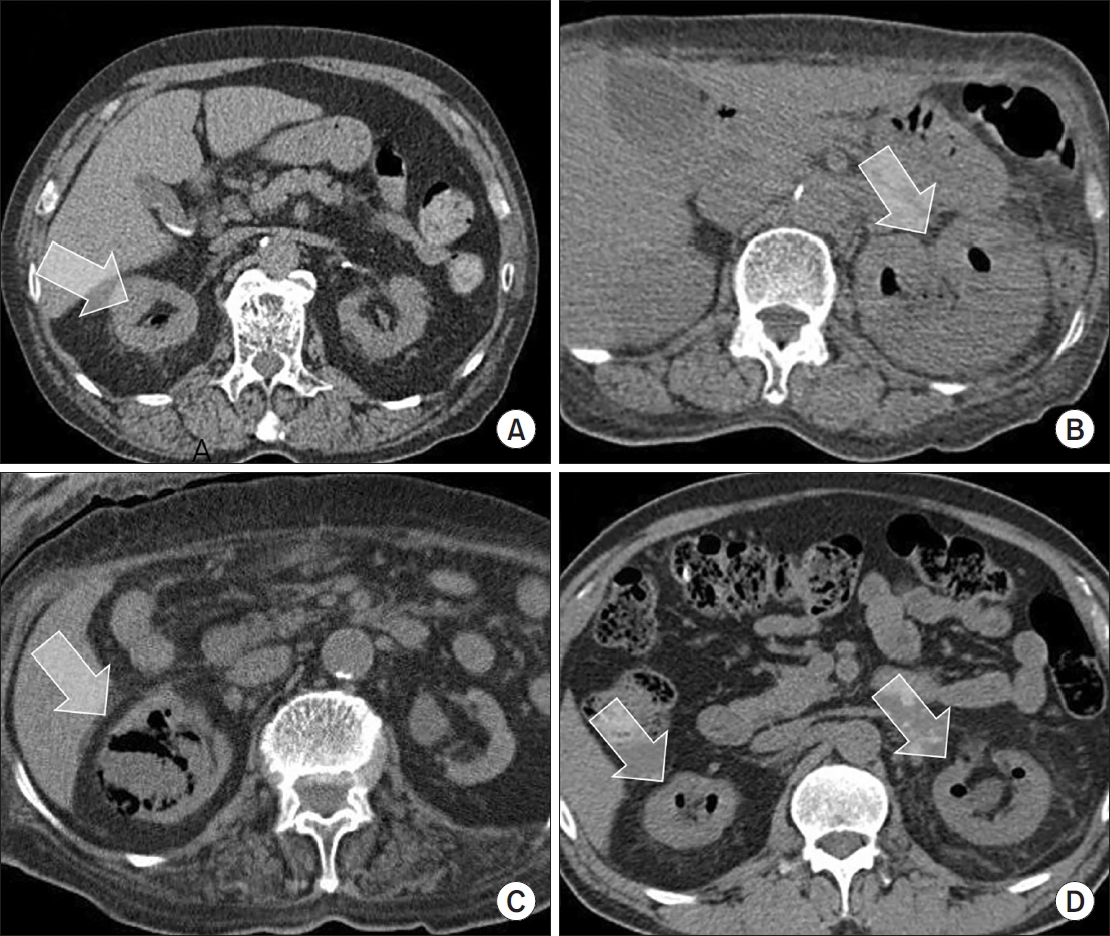
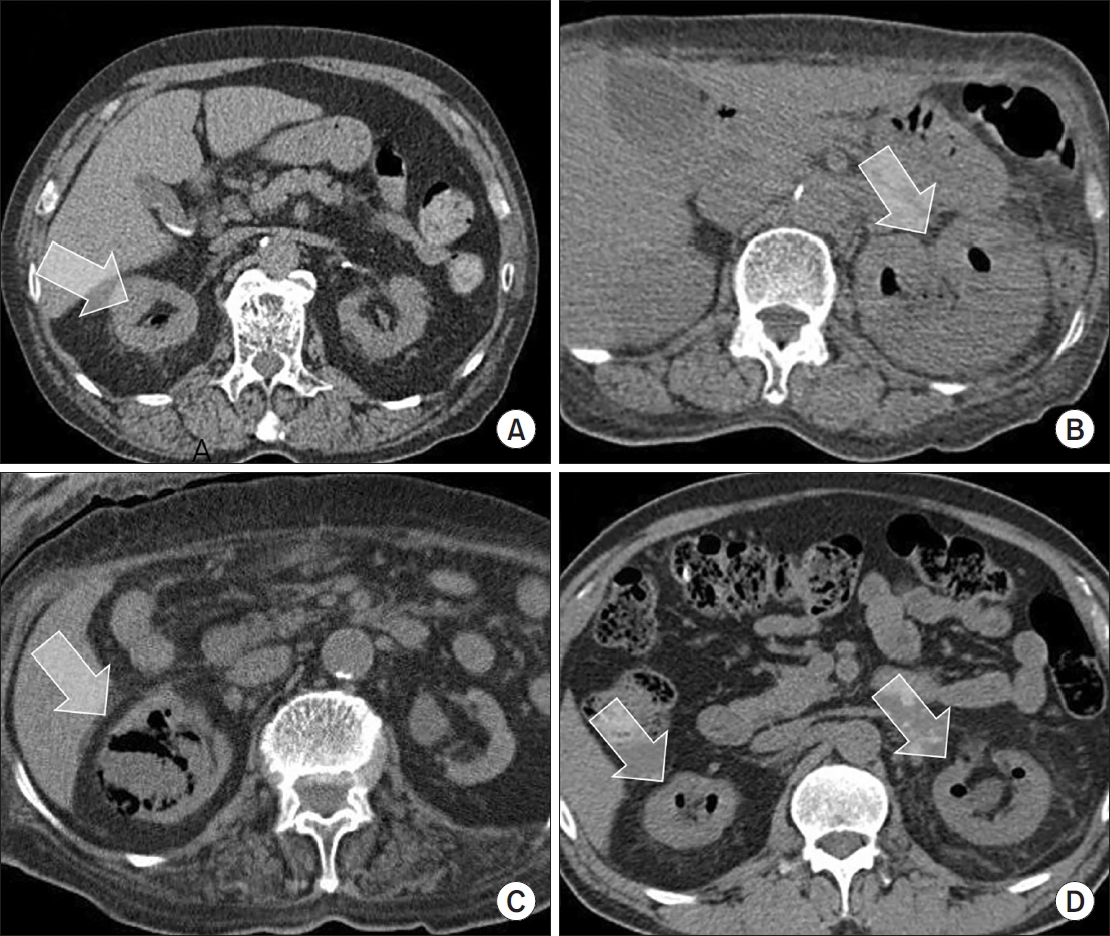
Emphysematous pyelonephritis (EPN) is a life-threatening disease requiring immediate treatment. This multicenter retrospective cohort study aimed to analyze the mortality rate and risk factors associated with EPN.
Materials and Methods: Between January 2011 and February 2021, 217 patients diagnosed with EPN via computed tomography who visited 14 teaching hospitals were retrospectively analyzed. Clinical data, including age, sex, comorbidities, Huang and Tseng classification, hydronephrosis, acute kidney injury, blood and urine tests, surgical interventions, percutaneous drainage, and conservative treatments, were compared between the survival and death groups. Risk factors for mortality due to EPN were analyzed using univariate and multivariate methods.
Results
The mean age of survivors and deceased patients was 67.8 and 69.0 years, respectively (p=0.136). The sex distribution (male/female) was 48/146 and 8/15, respectively (p=0.298). Of the 217 patients, 23 died, resulting in a mortality rate of 10.6%. In univariate analysis, the Huang and Tseng classification (p=0.004), platelet count (p=0.005), and acute kidney injury (p=0.007) were significantly associated with mortality from EPN. In multivariate analysis, only the Huang and Tseng classification (p=0.029) was identified as a risk factor. Mortality rates according to the Huang and Tseng classification were as follows: class I (5.88%), class II (7.50%), class IIIa (14.28%), class IIIb (25.00%), and class IV (23.07%).
Conclusions
EPN is associated with a high mortality rate. Among various clinical factors, the Huang and Tseng classification was the most significant indicator for predicting mortality.
-
Citations
Citations to this article as recorded by  - Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
-
3,370
View
-
60
Download
-
1
Crossref
-
The Urinary Microbiome: A Pediatric Urological Perspective
-
Sang Don Lee, Jae Min Chung
-
Urogenit Tract Infect 2022;17(3):61-70. Published online December 31, 2022
-
DOI: https://doi.org/10.14777/uti.2022.17.3.61
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- The human microbiome is currently being studied with increasing interest. The microbiome refers to the microorganisms living in the body and their genetic information. The human body is known to contain 1.3 to 10 times more microorganisms than human cells. The Human Microbiome Project was started in 2007 to characterize the human microbiome and analyze its role in human health and diseases. Based on the recent microbiome literature, alterations in the microbiome are associated with several non-urological diseases in pediatrics, such as infantile colic, necrotizing enterocolitis, asthma, atopy, obesity, type-1 diabetes, autism, atopic dermatitis, psoriasis, and bronchial asthma. While some urinary microbiome studies (including prostate cancer, bladder cancer, interstitial cystitis, urge urinary incontinence, overactive bladder, stone disease, and urinary tract infections) have been conducted in adults, there are very few pediatric urinary microbiome studies. This study reviews the role of the urinary microbiome in urinary tract diseases from a pediatric urological perspective.
-
Characteristics and Treatment Trends for Emphysematous Pyelonephritis in Korea: A 10-Year Multicenter Retrospective Study
-
Seung-Kwon Choi, Koo Han Yoo, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2021;16(2):49-54. Published online August 31, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.2.49
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study examined the characteristics, current treatment trends, and outcomes of patients with emphysematous pyelonephritis (EPN) in Korea.
Materials andMethods: Two hundred and seventeen patients diagnosed with EPN were evaluated using abdominal computed tomography in 2011-2021 at 15 institutes in Korea. The patients’ demographic and clinical characteristics, treatment modalities, and treatment outcomes were analyzed. The total study period was divided arbitrarily into groups A (2011-2014), B (2015-2017), and C (2018-2021) to analyze the trends in the EPN treatment.
Results: The mean age of the patients was 65.1 years; there were more female patients (74.2%) than male patients. The overall mortality rate was 10.6%. Ninety-five (43.8%), 98 (45.2%), and 24 (11.0%) patients were treated with medical, minimally invasive, and surgical management, respectively; the corresponding mortality rates were 13.7%, 6.1%, and 16.7%. There was no significant change in the proportion of patients treated with medical management over time (group A=46.5%, group B=47.0%, and group C=38.8%). The proportion of patients treated with minimally invasive management gradually increased over time (group A=35.2%; group B=43.9%; group C=55.0%), while those who underwent surgical management decreased gradually over time (group A=18.3%, group B=9.1%, and group C=6.3%). No differences in mortality rates were observed between the groups.
Conclusions: EPN with medical and minimally invasive management had a relatively high treatment success rate, which increased gradually, while surgical management decreased gradually over time in Korea. The mortality rate was relatively lower than that reported in studies published before the 2010s.
-
Risk Factors of Febrile Urinary Tract Infection after Ureteral Reimplantation in Infant
-
Seungsoo Lee, Jae Min Chung, Sang Don Lee
-
Urogenit Tract Infect 2020;15(2):33-37. Published online August 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.2.33
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: Children with febrile urinary tract infection (fUTI) and vesicoureteral reflux (VUR) show significant morbidity. Few studies have examined the incidence of fUTI after ureteral reimplantation for congenital urinary tract anomalies, particularly in infants. Therefore, this study examined the incidence and risk factors of fUTI after ureteral reimplantation in infants.
Materials and Methods: Children under one year of age, who underwent ureteral reimplantation from July 2017 to December 2018, were reviewed retrospectively. The patients’ data were analyzed to evaluate the predictors of fUTI after ureteral reimplantation.
Results: Ureteral reimplantation was performed in 16 patients (25 ureters) at a mean of 8.9±2.8 months. The preoperative diagnosis was VUR 14 (87.5%), obstructive megaureter 1 (6.3%), duplicated ureter 1 (6.3%). Postoperative fUTI occurred in five patients (31.3%) during the follow-up period (average 9.6±5.9 months, range 3-18 months). UTI occurred at 40.8±16.6 (17-61) days after surgery. Fourteen ureters were implanted with a ureteral catheter for three days, and 11 ureters were implanted with a double J ureteral stent for six weeks. The children’s age, sex, surgical method, renal scar, reflux grade, laterality, persisting VUR, and presence of double J ureteral stent were not predictive factors for postoperative fUTI.
Conclusions: The incidence of fUTI after ureteral reimplantation in infants was 31.3%, and all fUTI occurred within two months after surgery. The risk factors associated with fUTI after ureteral reimplantation could not be predicted.
-
Citations
Citations to this article as recorded by  - Open vs. robot-assisted laparoscopic ureteral reimplantation in a contemporary pediatric cohort: a retrospective single-institution analysis
Suhaib Abdulfattah, Nicole J. Kye, Sanjay Aiyar, Emily Ai, Marina Quairoli, Meghan F. Davis, Karl Godlewski, Katherine Fischer, Christopher J. Long, Dana A. Weiss, Aseem R. Shukla, Arun K. Srinivasan, Sameer Mittal
Journal of Robotic Surgery.2026;[Epub] CrossRef - Etiological Agents of Urinary Tract Infection (UTI)
Rana Thamer Hadi Alkhafaji, M. Jayashankar
International Journal of Scientific Research in Science and Technology.2022; : 381. CrossRef
-
2,980
View
-
10
Download
-
2
Crossref
-
Analysis of Uropathogens of Febrile Urinary Tract Infection in Infant and Relationship with Vesicoureteral Reflux
-
Kyung Hwan Kim, Seung Hee Seo, Sang Don Lee, Jae Min Chung
-
Urogenit Tract Infect 2018;13(3):58-65. Published online December 31, 2018
-
DOI: https://doi.org/10.14777/uti.2018.13.3.58
-
-
 Abstract Abstract
 PDF PDF
- Purpose: This study aimed to investigate the relationship between uropathogens of infants with febrile urinary tract infection (UTI) and vesicoureteral reflux (VUR).
Materials and Methods: We analyzed 308 infants hospitalized for febrile UTI between January 2010 and December 2015, and assessed the voiding cystourethrography (VCUG). The medical records, including clinical symptoms, laboratory findings, urinalysis, urine culture tests, ultrasound (US), dimercaptosuccinic acid scan, and VCUG, were retrospectively obtained. The incidences of VUR and high-grade VURs (III, IV, and V) were analyzed in 4 groups categorized by uropathogens and renal US findings.
Results: The mean age of 308 infants was 3.29±2.18 months. The male-to-female ratio was 3.46:1. In urine culture tests, 267 infants (86.69%) showed single bacterial uropathogen; Escherichia coli in 241 infants (78.25%) and non-E. coli uropathogens in 26 infants (8.44%). Multiple distinctive microorganisms were identified as causative uropathogens in 41 infants (13.31%). Abnormal findings of US and VCUG were identified in 216 and 64 patients, respectively. In 308 infants, the incidences of VUR and high-grade VUR were not different among the 4 groups. In 239 male infants, the incidences of high-grade VUR were higher in patients with non-E. coli single or multiple uropathogen and with abnormal US findings (p=0.042).
Conclusions: In male infants with non-E. coli uropathogen or multiple uropathogens and with abnormal US findings at febrile UTI, there was an increased chance of finding high-grade VURs on subsequent VCUG tests.
-
Citations
Citations to this article as recorded by  - Low yield from imaging after non-E. coliurine tract infections in children treated in primary care and emergency department
Yincent Tse, Charlie Pickles, Stephen Owens, Michal Malina, Richard Peace, Milan Gopal
Archives of Disease in Childhood.2023; 108(6): 474. CrossRef - E. coli versus Non-E. coli Urinary Tract Infections in Children
Abdullah Al Nafeesah, Khaled Al Fakeeh, Syed Chishti, Tahir Hameed
International Journal of Pediatrics and Adolescent Medicine.2022; 9(1): 46. CrossRef
-
861
View
-
0
Download
-
2
Crossref
-
The Clinical Guidelines for Acute Uncomplicated Cystitis and Acute Uncomplicated Pyelonephritis
-
Ki Ho Kim, Jae Heon Kim, Seung-Ju Lee, Hong Chung, Jae Min Chung, Jae Hung Jung, Hyun Sop Choe, Hun Choi, Sun-Ju Lee, The Committee of The Korean Association of Urogenital Track Infection and Inflammation
-
Urogenit Tract Infect 2017;12(2):55-64. Published online August 31, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- To date, there has not been an establishment of guidelines for urinary tract infections, due to limited domestic data in Korea, unlike other North American and European countries. The clinical characteristics, etiology, and antimicrobial susceptibility of urinary tract infections vary from country to country. Moreover, despite the same disease, antibiotic necessary to treat it may vary from country to country. Therefore, it is necessary to establish a guideline that is relevant to a specific country. However, in Korea, domestic data have been limited, and thus, guidelines considering the epidemiological characteristics pertaining specifically to Korea do not exist. Herein, describe a guideline that was developed by the committee of The Korean Association of Urogenital Tract Infection and Inflammation, which covers only the uncomplicated urinary tract infections, as covering all parts in the first production is difficult.
-
The Antibiotic Susceptibility of Escherichia coli from Community-Acquired Uncomplicated Urinary Tract Infection: A Focused on Fosfomycin
-
Hyun-Sop Choe, Seung-Ju Lee, In Ho Chang, Tae-Hyoung Kim, Hong Chung, Jae Min Chung, Sang Don Lee, Jae Hung Jung, Ki Ho Kim, Seung Ki Min, Yong Gil Na, Hana Yoon, Ho Song Yu, Mi-Kyung Lee, Sun-Ju Lee
-
Urogenit Tract Infect 2017;12(2):77-81. Published online August 31, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: To assess the antibiotic susceptibility of Escherichia coli from community-acquired uncomplicated urinary tract infection (UTI).
Materials and Methods: Between August and December of 2015, confirmed cases of E. coli as a pathogen of community-acquired uncomplicated UTI were collected and assessed for antibiotic susceptibility in 10 designated hospitals. Additional fosfomycin susceptibility test was performed by a central laboratory using the disk diffusion method.
Results: A total of 347 E. coli isolates were collected from urine samples of community-acquired uncomplicated UTIs patients. The susceptibility rates of antibiotics were as follows: amikacin 100.0% (347), imipenem 100.0% (347), ciprofloxacin 57.1% (198), cefotaxime 74.9% (260), ampicillin 30.0% (104), trimethoprim/sulfamethoxazole 66.9% (232), and fosfomycin 98.0% (340). All fosfomycin-resistant E. coli isolates were extended-spectrum β-lactamase (ESBL)-producing. In 85 cases of ESBL-producing E. coli, the fosfomycin susceptibility rate was 91.8% (78/85).
Conclusions: Fosfomycin may be a useful option for the treatment of community-acquired uncomplicated UTIs. Further studies evaluating the role of fosfomycin in the treatment of UTIs and its clinical efficacy are necessary.
-
Antimicrobial Resistance and Urinary Tract Infections: Biggest Threats
-
Young Sam Cho, Jae Min Chung
-
Urogenit Tract Infect 2017;12(1):1-2. Published online April 30, 2017
-
-
-
 PDF PDF
-
2017 Guidelines of The Korean Association of Urogenital Tract Infection and Inflammation: Acute Uncomplicated Cystitis
-
Ki Ho Kim, Seung-Ju Lee, Yong-Hyun Cho, Hyun-Sop Choe, Yong Gil Na, Jae Heon Kim, Hong Chung, Jae Min Chung, Jae Hung Jung, Hoon Choi, Sun-Ju Lee
-
Urogenit Tract Infect 2017;12(1):3-6. Published online April 30, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Acute uncomplicated cystitis is the most common urinary tract infection that mainly occurs in adult females, particularly sexually active young women and postmenopausal women. It is commonly observed in primary health care settings, including urology as well as obstetrics and gynecology; more than half of healthy adult women visit clinics and hospitals at least once in their lifetime due to acute uncomplicated cystitis. The most common bacterium causing this condition is Escherichia coli, followed by Staphylococcus saprophyticus, Klebsiella pneumoniae, Proteus mirabilis, and etc. Trimethoprim-sulfamethoxazole or fluoroquinolones have been used as an empirical antibiotic treatment. However, as fluoroquinolone-resistant organisms or extended spectrum beta-lactamase-producing organisms are becoming more prevalent worldwide, information on regional antibiotic resistance and guidelines on antibiotic use are becoming increasingly more desparate.
-
2017 Guidelines of The Korean Association of Urogenital Tract Infection and Inflammation: Recurrent Urinary Tract Infection
-
Seung-Ju Lee, Hyun-Sop Choe, Yong Gil Na, Ki Ho Kim, Jae Heon Kim, Hong Chung, Jae Min Chung, Jae Hung Jung, Hoon Choi, Sun-Ju Lee, Yong-Hyun Cho
-
Urogenit Tract Infect 2017;12(1):7-14. Published online April 30, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Recurrent infection after an acute urinary tract infection (UTI) episode is common in adult women. It is onerous to both the patient and the physician to treat frequent recurrent UTI. Every time when UTI recurs, patients experience lower urinary tract symptoms, fatigue, and limitation in everyday life, while the physician has difficulty in counseling patients with a disease entity whose pathophysiology is less known. Currently, prophylactic treatment for recurrent UTI is limited, is ineffective in most cases, and sometimes accompanies unexpected side effects. In this guideline, we aimed to establish feasible and effective recommendations for the treatment of recurrent UTI in healthy adult women.
-
Infectious Complications after Prostate Biopsy: A Prospective Multicenter Prostate Biopsy Study
-
Eu Chang Hwang, Ho Song Yu, Seung Il Jung, Dong Deuk Kwon, Sun Ju Lee, Tae-Hyoung Kim, In Ho Chang, Hana Yoon, Bongsuk Shim, Kwang Hyun Kim, Donghyun Lee, Jung-Sik Huh, Dong Hoon Lim, Won Jin Jo, Seung Ki Min, Gilho Lee, Ki Ho Kim, Tae Hwan Kim, Seo Yeon Lee, Seung Ok Yang, Jae Min Chung, Sang Don Lee, Chang Hee Han, Sang Rak Bae, Hyun Sop Choe, Seung-Ju Lee, Hong Chung, Yong Gil Na, Seung Woo Yang, Sung Woon Park, Young Ho Kim, Tae Hyo Kim, Won Yeol Cho, June Hyun Han, Yong-Hyun Cho, U-Syn Ha, Heung Jae Park, The Korean Association of Urogenital Tract Infection and Inflammation (KAUTII)
-
Urogenit Tract Infect 2016;11(1):17-24. Published online April 30, 2016
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: Recent studies have highlighted an increasing trend of infectious complications due to fluoroquinolone-resistant organisms among men undergoing transrectal prostate biopsy. This study evaluated the current incidence of infective complications after trans-rectal prostate biopsy for identification of risk factors in Korean men who received fluoroquinolone prophylaxis.
Materials and Methods: A prospective, multicenter study was conducted in Korea from January to December 2015. Prostate biopsies performed with fluoroquinolone prophylaxis during 3 months in each center were included. A pre-biopsy questionnaire was used for identification of patient characteristics. Clinical variables including underlying disease, antibiotic prophylaxis, enema, povidoneiodine cleansing of the rectum, and infectious complications were evaluated. The primary outcome was the post-biopsy infection rate after fluoroquinolone prophylaxis. Univariable and multivariable analyses were used for identification of risk factors for infectious complications.
Results: The study included 827 patients, of whom 93 patients (11.2%) reported receiving antibiotics in the previous 6 months and 2.5% had a history of prostatitis. The infectious complication rate was 2.2%. Post-biopsy sepsis was reported in 2 patients (0.2%). In multivariable analysis predictors of post-biopsy sepsis included person performing biopsy (adjusted odds ratio [OR], 4.05; 95% confidence interval [CI], 1.31-12.5; p=0.015) and operation history within 6 months (adjusted OR, 5.65; 95% CI, 1.74-18.2; p=0.004).
Conclusions: The post-prostate biopsy infectious complication rate in this study was 2.2%. Person performing biopsy (non-urologists) and recent operation history were independent risk factors for infectious complications after trans-rectal prostate biopsy.
-
Predictive Parameters of Testicular Salvage of Pediatric Testicular Torsion: A 6-Year Experience of a Single Center
-
Seungsoo Lee, Bu Kyung Park, Moon Kee Chung, Jae Min Chung, Sang Don Lee
-
Urogenit Tract Infect 2016;11(1):25-29. Published online April 30, 2016
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: We evaluated parameters associated with testicular salvage in boys with testicular torsion.
Materials and Methods: During 2009-2014, 19 boys younger than 18 years old underwent emergency surgery for testicular torsion in our hospital. Age, chief complaint, laterality of the torsion, physical appearance, ultrasonographic results, duration between the onset of symptoms and hospital visit, duration between the onset of symptoms and start of surgery, intraoperative appearance, surgical method (orchiopexy or orchiectomy), and any postoperative complications were analyzed retrospectively. Cases were categorized according to salvageable testes (n=14) or unsalvageable testes (n=5) groups based on testes viability.
Results: The mean age was not significantly different between the two groups. All patients were diagnosed using color Doppler ultrasonography of the scrotum. Six (42.9%) boys in the salvageable testes group and all five in the unsalvageable testes group were transferred from other clinics or hospitals (p=0.026). The mean duration between the onset of symptoms and hospital visit was 925 minutes in the salvageable testes group and 3,488 minutes in the unsalvageable testes group (p=0.042), and the mean duration between the onset of symptoms and start of surgery was 1,131 minutes in the salvageable testes group and 3,777 minutes in the unsalvageable testes group (p=0.042).
Conclusions: There was a high possibility that orchiectomy was required if surgery was delayed. However, even when a boy is admitted to the hospital more than 24 hours after the onset of symptoms, the testis can still be viable provided the surgery is performed as quickly as possible.
-
Characteristics of Patients Who Visited the Emergency Room after Prostate Biopsy: Single Center Retrospective Study
-
Seung Chan Jeong, Seungsoo Lee, Jae Min Chung, Sang Don Lee
-
Urogenit Tract Infect 2015;10(2):120-125. Published online October 31, 2015
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: To educate patients and prevent biopsy-related complications, it is helpful to understand the causes for visiting the emergency room (ER). Therefore, we want to analyze the causes and factors of complications that cause patients to visit the ER after prostate biopsy.
Materials and Methods: We conducted a study of in-patients who visited the ER of Pusan National University Yangsan Hospital after prostate biopsy from December 2008 to July 2015. Age, postoperative interval before visiting the ER, Charlson comorbidity index (CCI) score, symptoms in ER, prostate size, pathologic result, and number of biopsy cores were analyzed retrospectively.
Results: Among all 1,694 cases of patients who had undergone prostate biopsies during a 7-year period, only 37 patients (2.2%) visited the ER. Diabetes mellitus (DM) is the most common underlying disease among patients with accompanying infection-related symptoms compared to patients with accompanying non-infection- related symptoms (p<0.001). In univariate analysis, DM (p=0.004) and CCI score (p=0.030) were statistically significant risk factors for infection, but only DM was significant in multivariate analysis (p=0.004). Prostate size (p=0.044) was a significant risk factor for acute urinary retention (AUR) in univariate analysis, but not statistically significant in multivariate analysis. CCI score was a statistically significant risk factor for bleeding (p=0.005 [univariate], 0.035 [multivariate]).
Conclusions: AUR after transrectal ultrasound-biopsy is the most common reason for visiting the ER. CCI score showed correlation with bleeding and DM showed correlation with infection. Consideration of risk factors of complications after prostate biopsy will be helpful to the patients in the treatment and prevention of complication.
-
Xanthogranulomatous Inflammation of Urachus
-
Jeong Hyun Oh, Jae Min Chung, Seong Choi
-
Korean J Urogenit Tract Infect Inflamm 2013;8(1):55-58. Published online April 30, 2013
-
-
-
 Abstract Abstract
 PDF PDF
- Urachal xanthogranuloma is an extremely rare disease. An 18-year-old male presented with lower abdominal pain, hematuria, and dysuria. An urachal mass with bladder invasion, which was suspected to be an urachal carcinoma or abscess, was observed on computed tomography. Exploratory laparotomy, excision of the urachus, and partial cystectomy was performed by way of a lower midline incision. Histopathologic examination identified the mass as an urachal xanthogranuloma.
-
Ureterosigmoidal Fistula Complicated by Crohn's Disease
-
Jeong Hyun Oh, Jae Min Chung, Seong Choi
-
Korean J Urogenit Tract Infect Inflamm 2012;7(1):73-76. Published online April 30, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- We report a case of ureterosigmoidal fistula in a 38 year-old-man with Crohn's disease, who was presented with pneumaturia and feces in urine. Computed tomography showed a fistula between the right ureter and the sigmoid colon, which was successfully managed with right transureteroureterostomy.
-
Clinical Outcome of Acute Bacterial Prostatitis; A Multicenter Study
-
Seong Ju Lee, Jin Mo Koo, Bong Suk Shim, Yong Hyun Cho, Chang Hee Han, Seung Ki Min, Sung Joo Lee, Hwan Cheol Son, Jun Mo Kim, Jong Bo Choi, Tae Hyoung Kim, Sang Kuk Yang, Kil Ho Lee, Yong Kil Na, Sung Ho Lee, Hee Jong Jung, Seung Il Jung, Chul Sung Kim, Jae Min Chung, Young Jin Seo, Won Yeol Cho, Kweon Sik Min, Sang Don Lee
-
Korean J Urogenit Tract Infect Inflamm 2011;6(2):165-170. Published online October 31, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: Proper guidelines concerning antibiotic administration for acute bacterial prostatitis (ABP) are unclear. We retrospectively analyzed treatment status and clinical outcomes to establish a proper treatment guideline. Materials and Methods: The clinical records of 669 patients from 21 hospitals diagnosed with ABP were reviewed. Prior manipulation, antibiotics administration, mean length of treatment, complication and procedure were analyzed. Results: The mean age of 538 patients (80.4%) without manipulation (group 1) and 131 patients (19.6%) with manipulation (group 2) was 58.3 years (range 19-88 years). Transrectal prostate biopsy was the most common cause of acute bacterial prostatitis (n=66; 50.4%). Of the clinical symptoms in the non-manipulation and manipulation groups, fever was most common (88.2% and 86.3%, respectively). Acute urinary retention (14.3% and 28.1%, respectively) was significantly increased in the manipulation group (p<0.05). Escherichia coli was the most frequently isolated bacterium from urine (72.0% and 66.7% of cases, respectively). Mean length of treatment was 6.5days and 7.9days, respectively; the difference was significant (p<0.05). Combination antibiotic therapy with third generation cephalosporin+aminoglycoside was used in 49.3% and 55.5% of cases, respectively. For single antibiotic therapy, second generation quinolones were used the most (35.5% and 34.3%, respectively). Sequale occurred in 29 group 1 patients (5.4%) and 20 group 2 patients (15.3%); the difference was significant (p<0.05). Conclusions: Prior manipulation was associated with 20% of ABP patients. Regardless of manipulation, clinical outcome was similar after treating with appropriate antibiotics."
-
Guideline for the Prevention of Health Care-associated Infection in Urological Practice in Japan
-
Jae Min Chung
-
Korean J Urogenit Tract Infect Inflamm 2011;6(2):230-239. Published online October 31, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- The present guideline for the prevention of health care-associated infection in urological practice is partially a result of numerous discussions of the working group in the Japanese Society of Urinary Tract Infection Cooperative Study Group. The results of these discussions were systematically organized by the Japanese Urological Association. They surveyed the literature including standard precautions, environmental considerations in both the inpatient and outpatient settings, the management of urinary catheters, endoscopy techniques, and the disinfection and sterilization of instruments used in endoscopies and related procedures. The concept of this guideline is to show the minimum precautions that urologists and other medical professionals should observe when they work in the urological field. Standard precautions based on hand hygiene and the use of personal protective equipment should be observed in both the inpatient and outpatient settings. In the inpatient setting, the management of the toilet is important. Collecting urine should be restricted only when it is necessary to determine a patient’s urinary output. The management for urinary catheter and infection are created based on the “European and Asian guidelines on management and prevention of catheter-associated urinary tract infections”. In addition, we propose that nephrostomy should be carried out after maximum barrier precautions have been taken. Urinary catheters are replaced in the event of an occlusion or if there are signs that an occlusion might occur, but the same catheter cannot be left in place for more than 2 months. Regarding the handling of urine containing Mycobacterium tuberculosis, airborne infection countermeasures are unnecessary, except for the laboratory personnel. For the procedures using urological endoscopes, aseptic techniques are recommended. Endoscopes and related devices should be used by sterilization or high-level disinfection, but formaldehyde gas cannot be used.
-
Emphysematous Cystitis Associated with Prostate and Urethra Involvement
-
Jae Min Chung, Jeong Hyun Oh, Su Hwan Kang, Seong Choi
-
Korean J Urogenit Tract Infect Inflamm 2011;6(1):80-83. Published online April 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- Emphysematous cystitis is primary infection of the bladder with gas production by bacteria. The infection is uncommon but commands clinical importance due to its morbidity and mortality potential. We report a 54 year-old man with emphysematous cystitis associated with prostatic and urethral involvement. He was managed with antibiotics and suprapubic catheterization.
-
Emphysematous Prostatitis Accompanied by Septicemia
-
Jae Min Chung, Jung Choi, Jun Taik Lee
-
Korean J Urogenit Tract Infect Inflamm 2010;5(2):207-210. Published online October 31, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- Emphysematous prostatitis is an uncommon condition which is characterized by air pockets and abscess within the prostate. We report 68-year-old man with emphysematous prostatitis accompanying septicemia. He was successfully treated with antibiotics and transurethral resection of prostatic abscess.
-
Clinical Guideline of Chancroid
-
Jae Min Chung, Ki Ho Kim
-
Korean J Urogenit Tract Infect Inflamm 2010;5(1):13-17. Published online April 30, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- Chancroid is an acute localized, autoinoculable venereal disease caused by Haemophilus ducreyi, characterized clinically by painful ulceration at the site of incubation, and frequently accompanied by regional lymphadenopathy, and short incubation period. Chancroid is a cofactor for of human immunodeficiency virus (HIV) transmission, as are genital herpes and syphilis; high rates of HIV infection among patients who have chancroid occur in some countries. A definitive diagnosis of chancroid requires the identification of H. ducreyi on special culture media. The combination of a painful genital ulcer and tender suppurative inguinal adenopathy suggests the diagnosis of chancroid. Recommended regimens for chancroid in HIV-infected patients are either azithromycin, 1g as a single oral dose, or ceftriaxone, 250mg as a single intramuscular dose. After prompt treatment, close follow-up is essential.
-
Lupus Cystitis Associated with Pediatric-onset Systemic Lupus Erythematosus
-
Jae Min Chung, Geun Tae Kim, Seong Choi, Jae Sun Park
-
Korean J Urogenit Tract Infect Inflamm 2010;5(1):87-92. Published online April 30, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- Systemic lupus erythematosus (SLE) is a disease of unknown cause which involves various organs and primary involvement of urinary bladder is very rare. We experienced a case of a girl aged 12 years who was diagnosed as SLE associated with paralytic ileus and urologic manifestations (interstitial cystitis, hydroureters and hydronephrosis). To our knowledge, the combination of paralytic ileus and interstitial cystitis is quite uncommon in pediatric-onset SLE.
-
Effect of Associated Diseases to Renal and Perirenal Abscesses
-
Dong Gil Shin, Hong Koo Ha, Jae Min Chung, Sang Don Lee
-
Korean J Urogenit Tract Infect Inflamm 2009;4(2):202-209. Published online October 31, 2009
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: We analyzed the clinical experiences of patients with renal and perirenal abscesses during the last 10 years according to associated diseases. Materials and Methods: We reviewed the medical records of 63 patients with renal, perirenal, and mixed abscesses treated at two hospital from January 1999 to August 2009. The patients were divided into 3 groups: group A consisted of 11 patients without associated diseases, group B consisted of 31 patients with nonurological associated diseases and group C consisted of 21 patients with urological associated diseases. Results: A male to female sexual ratio of 63 patients was 1:2, and the mean age was 51.4±15.2 years, respectively. The most common associated diseases were diabetes mellitus (39.7%) and liver disease (19.0%). The most common urological associated diseases were nephrolithiasis (11.1%) and ureteral obstruction (7.9%). Fever or flank pain were the common symptom. The most common isolated uropathogen in urine, blood and pus culture was E. coli. The hospitalized, clinical and laboratory improvement duration of group A was significantly shorter than group B and C, respectively. The hospitalized, clinical and laboratory improvement duration was not significantly different between group B and C. Most patients are cured or improved on discharge from hospital in all abscesses. Conclusions: We suggest that the renal and perirenal abscesses with associated diseases needs longer hospitalized days and more intensive treatment than that without associated diseases."
-
Cystic Renal Cell Carcinoma Mimicking a Renal Abscess
-
Jae Min Chung, Kyu Seop Kim, Seong Ju Kim, Byung Ju Sung, Sang Don Lee, Seong Choi
-
Korean J Urogenit Tract Infect Inflamm 2008;3(2):249-252. Published online October 31, 2008
-
-
-
 Abstract Abstract
 PDF PDF
- Cystic renal cell carcinoma is one form of renal cell carcinoma. The radiographic and pathologic findings of cystic renal cell carcinoma are often more confusing and less specific than the findings of solid renal cell carcinoma. We report a case of cystic renal cell carcinoma mimicking a renal abscess.
-
Renal Abscess Treated with Double J Catheter Insertion
-
Jae Min Chung, Seong Ju Kim, Byung Ju Sung, Sang Don Lee, Seong Choi
-
Korean J Urogenit Tract Infect Inflamm 2007;2(2):217-220. Published online October 31, 2007
-
-
-
 Abstract Abstract
 PDF PDF
- Renal abscess is uncommon and has variable symptoms of insidious onset. The most common pathogens are Escherichia coli. The patients with renal abscess usually present with fever, chills, abdominal or flank pain, and occasionally weight loss and malaise. Renal abscesses can be treated in various fashions. In these patients, renal abscess with hydronephrosis that does not respond to antimicrobial therapy was improved with double J catheter insertion.
-
Affecting Factors on the Treatment of Acute Pyelonephritis
-
Jae Min Chung, Seong Choi, Sang Don Lee
-
Korean J Urogenit Tract Infect Inflamm 2007;2(1):73-77. Published online May 31, 2007
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: We analyzed the clinical aspects of acute pyelonephritis patients who received hospitalization treatment and the factors to effect a therapy session. Materials and Methods: We evaluated 108 patients with acute pyelonephritis who underwent hospitalization treatment between January 2003 and May 2006. The patients were divided into two groups by history taking, radiological and laboratory finding: group A consisted of 60 patients without co-morbid condition and group B consisted of 48 patients with co-morbid conditions. Comparisons of the two groups were made using independent t-tests with hospitalized durations, uropathogen types, clinical improvement durations, laboratory improvement durations and co-morbid conditions. Results: The analysis included 108 patients with a male to female sexual ratio of 1:7.3, a mean age of 51.3±16.8 years and a mean number of hospitalized days of 9.7±9.2 days. The co-morbid conditions were hypertension in 18 patients (16.7%), LUTS in 16 patients (14.8%), and diabetes mellitus in 15 patients (13.9%). The hospitalized durations of two groups were 7.4±3.3 and 10.5±6.2 days in group A and B. The uropathogen types were all E. coli in group A, whereas E. coli, Pseudomonas and Enterococcus were isolated in group B. Clinical and laboratory improvement duration of group A was significantly shorter than group B. The longer hospitalized duration of group B was seen in chronic renal failure and diabetes mellitus patients for 10.4±5.4 and 14.0±4.3 days and the longer laboratory improvement duration of group B was seen in chronic renal failure and diabetes mellitus patients for 5.3±5.2 and 5.9±5.5 days. Conclusions: We concluded that the acute pyelonephritis with co-morbidity conditions need longer hospitalized days than that without co-morbidity conditions. Two variable (diabetes mellitus, chronic renal failure) that predicted a poor response after therapy for acute uncomplicated pyelonephritis. The more variable uropathogen were identified in a urine culture with co-morbidity conditions."
|