-
Mortality and Risk Factors for Emphysematous Pyelonephritis in Korea: A Multicenter Retrospective Cohort Study
-
Seung-Kwon Choi, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2025;20(1):34-41. Published online April 30, 2025
-
DOI: https://doi.org/10.14777/uti.2550006003
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose
Emphysematous pyelonephritis (EPN) is a life-threatening disease requiring immediate treatment. This multicenter retrospective cohort study aimed to analyze the mortality rate and risk factors associated with EPN.
Materials and Methods: Between January 2011 and February 2021, 217 patients diagnosed with EPN via computed tomography who visited 14 teaching hospitals were retrospectively analyzed. Clinical data, including age, sex, comorbidities, Huang and Tseng classification, hydronephrosis, acute kidney injury, blood and urine tests, surgical interventions, percutaneous drainage, and conservative treatments, were compared between the survival and death groups. Risk factors for mortality due to EPN were analyzed using univariate and multivariate methods.
Results
The mean age of survivors and deceased patients was 67.8 and 69.0 years, respectively (p=0.136). The sex distribution (male/female) was 48/146 and 8/15, respectively (p=0.298). Of the 217 patients, 23 died, resulting in a mortality rate of 10.6%. In univariate analysis, the Huang and Tseng classification (p=0.004), platelet count (p=0.005), and acute kidney injury (p=0.007) were significantly associated with mortality from EPN. In multivariate analysis, only the Huang and Tseng classification (p=0.029) was identified as a risk factor. Mortality rates according to the Huang and Tseng classification were as follows: class I (5.88%), class II (7.50%), class IIIa (14.28%), class IIIb (25.00%), and class IV (23.07%).
Conclusions
EPN is associated with a high mortality rate. Among various clinical factors, the Huang and Tseng classification was the most significant indicator for predicting mortality.
-
Citations
Citations to this article as recorded by  - Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
-
3,371
View
-
60
Download
-
1
Crossref
-
Impact of Antibiotics on the Efficacy of Immune Checkpoint Inhibitors in Metastatic Urothelial Carcinoma
-
Do Gyeong Lim, Ho Yeon Lee, Ho Seok Chung, Eu Chang Hwang, Seung Il Jung, Dong Deuk Kwon
-
Urogenit Tract Infect 2023;18(3):75-81. Published online December 31, 2023
-
DOI: https://doi.org/10.14777/uti.2023.18.3.75
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
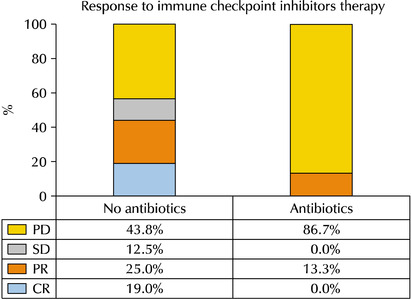
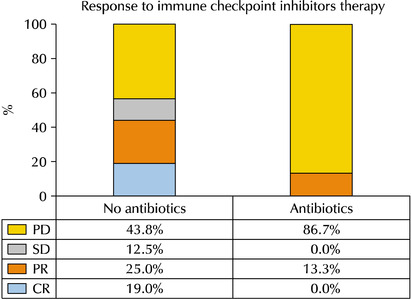
- Purpose: Emerging evidence has suggested that prior or concurrent antibiotic (ATB) use may be associated with a poor response to immune checkpoint inhibitors (ICIs) in patients with some solid tumors. This study examined the effects of ATB use on the oncological outcomes of patients receiving ICIs for mUC.
Materials and Methods: Patients receiving ICIs for mUC between 2018 and 2020 were assessed retrospectively. Those with over three cycles of atezolizumab or pembrolizumab were included. ATB use, defined as ≥ three days within 60 days before or three months after ICI administration, was compared between groups for oncological outcomes.
Results: Thirty-one patients were examined. The ATB-use and no-ATB-use groups consisted of 15 (48.4%) and 16 patients (51.6%), respectively. The ATB-use group showed a lower disease control rate (56.3% vs. 13.3%, p=0.023) than the no-ATB-use group. The objective response rate in the ATB-use group was lower than the no-ATB-use group, but the difference was statistically insignificant (43.7% vs. 13.3%, p=0.113). The ATB-use group had shorter progression-free survival (median three vs. six months, log-rank p=0.045) and shorter overall survival (median three vs. 14 months, log-rank p=0.023) than the no-ATB-use group. The most commonly used antibiotics were fluoroquinolones (46.7%), cephalosporins (40.0%), non-cephalosporin beta-lactams (6.7%), and nitrofurantoin (6.7%).
Conclusions: ATB may be associated with poorer oncological outcomes in patients with mUC who received ICI therapy. Hence, further research will be needed to understand the relationship between the modulation of ATB-related dysbiosis and gut microbiota composition with the oncological outcomes in patients with mUC.
-
Korean Multicenter Study of Infectious Complications after Transurethral Prostate Surgery in Patients with Preoperative Sterile Urine
-
Seong Hyeon Yu, Seung Il Jung, Eu Chang Hwang, Tae-Hyoung Kim, Jae Duck Choi, Koo Han Yoo, Jeong Woo Lee, Dong Hoon Koh, Sangrak Bae, Seung Ok Yang, Joongwon Choi, Seung Ki Min, Hoon Choi
-
Urogenit Tract Infect 2022;17(3):81-88. Published online December 31, 2022
-
DOI: https://doi.org/10.14777/uti.2022.17.3.81
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: To evaluate the efficacy of antibiotic prophylaxis and determine the risk factors of infectious complications after transurethral surgery of the prostate.
Materials and Methods: Seven hundred and seventy-two patients who underwent transurethral resection of the prostate (TURP) or holmium laser enucleation of the prostate (HOLEP) were reviewed. Of these, this study enrolled 643 patients without bacteriuria who had not received antibiotics for urinary tract infections for two weeks before surgery. The patients were divided into two groups according to the duration of the antibiotics (Group 1: less than one day, n=396 vs. Group 2: more than one day, n=247).
Results: The overall incidence of postoperative infectious complications in 643 patients was 5.0% (32/643). When postoperative infectious complications were compared according to the duration of the antibiotics (Group 1 vs. Group 2), the infectious complications rates were 5.6% (22/396) vs. 4.0% (10/247), respectively (p=0.393). When postoperative infectious complications were compared according to the duration of antibiotics (Group 1 vs. Group 2) in the TURP and HOLEP groups, the infectious complications rates were 6.3% (12/192) vs. 1.0% (1/103) (p=0.035) and 4.9% (10/203) vs. 6.0% (8/134) (p=0.677), respectively. The duration of Foley catheterization was independently associated with infectious complications (p=0.003).
Conclusions: The results showed that prolonged postoperative catheterization affects postoperative infectious complications associated with transurethral prostate surgery. Although antibiotics administered for less than one day are effective for antibiotic prophylaxis of transurethral prostate surgery, a longer antibiotic therapy is recommended for TURP.
-
Citations
Citations to this article as recorded by  - Evaluation of Postoperative Urinary Tract Infection and Sepsis Rates After Adding Cystolitholapaxy to HoLEP:
A Retrospective Analysis
Federico Rovegno, Rajiv Pillai, Zafar Maan, Soumendra Datta, Omar Nasir, Gerald Rix
International Journal of Clinical Urology.2026; 10(1): 1. CrossRef
-
3,723
View
-
24
Download
-
1
Crossref
-
Care of Voiding Dysfunction in Rehabilitation and Convalescent Hospitals
-
Seong Hyeon Yu, Eu Chang Hwang, Seung Il Jung
-
Urogenit Tract Infect 2021;16(2):32-43. Published online August 31, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.2.32
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- The number of rehabilitation and convalescent hospitals is increasing rapidly; the primary goal of these institutions is to manage patients’ chronic disorders and maintain their daily functions. Most patients in these hospitals are elderly and experience difficulties related to behavior, communication, or cooperation because of various co-existing chronic medical diseases. Therefore, urologic problems may be more prevalent in these hospitals compared to other hospitals. On the other hand, unlike the medical management of other chronic medical problems, urologic problems have been neglected. This situation could increase the secondary complications, decrease the quality of life, and exacerbate co-existing conditions among such patients. Therefore, this review investigates problems concerning voiding dysfunction-related care in rehabilitation and convalescent hospitals and seeks solutions to overcome them.
-
Characteristics and Treatment Trends for Emphysematous Pyelonephritis in Korea: A 10-Year Multicenter Retrospective Study
-
Seung-Kwon Choi, Koo Han Yoo, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2021;16(2):49-54. Published online August 31, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.2.49
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
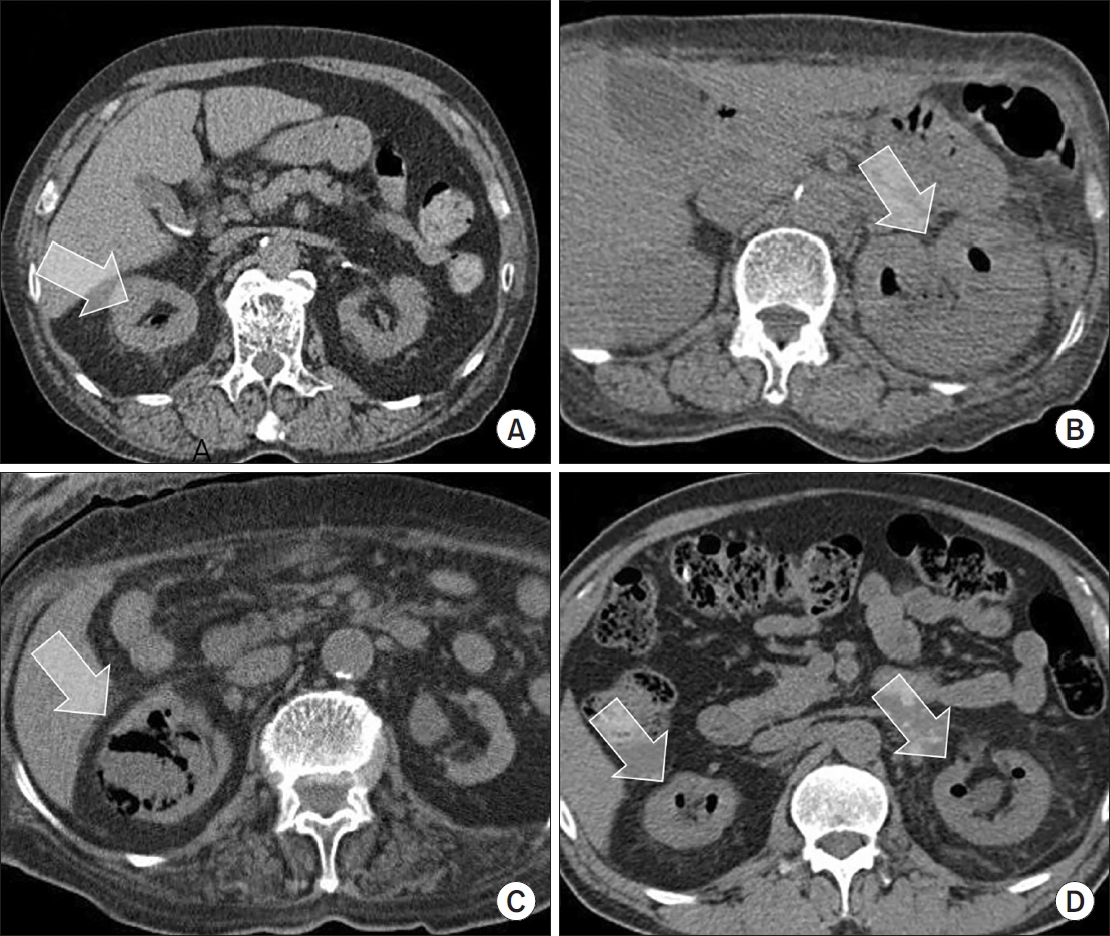
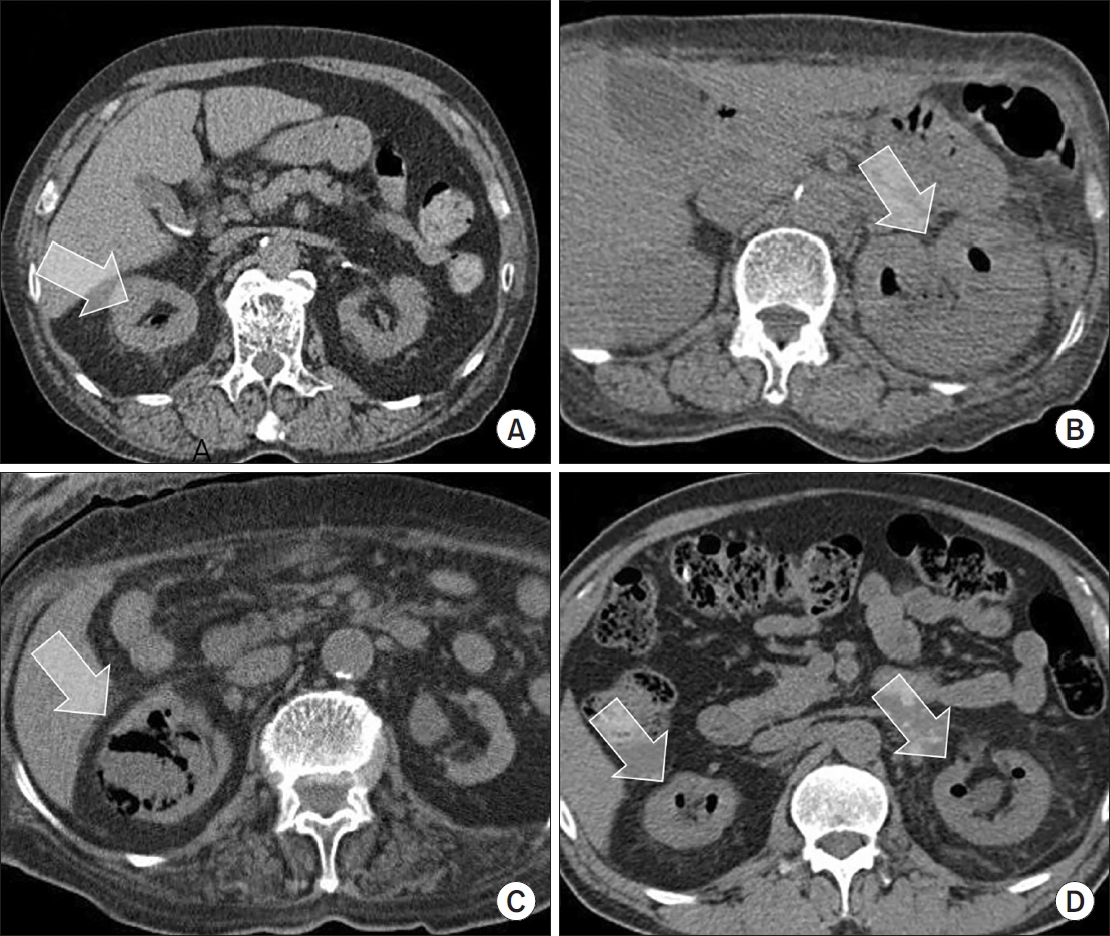
- Purpose: This study examined the characteristics, current treatment trends, and outcomes of patients with emphysematous pyelonephritis (EPN) in Korea.
Materials andMethods: Two hundred and seventeen patients diagnosed with EPN were evaluated using abdominal computed tomography in 2011-2021 at 15 institutes in Korea. The patients’ demographic and clinical characteristics, treatment modalities, and treatment outcomes were analyzed. The total study period was divided arbitrarily into groups A (2011-2014), B (2015-2017), and C (2018-2021) to analyze the trends in the EPN treatment.
Results: The mean age of the patients was 65.1 years; there were more female patients (74.2%) than male patients. The overall mortality rate was 10.6%. Ninety-five (43.8%), 98 (45.2%), and 24 (11.0%) patients were treated with medical, minimally invasive, and surgical management, respectively; the corresponding mortality rates were 13.7%, 6.1%, and 16.7%. There was no significant change in the proportion of patients treated with medical management over time (group A=46.5%, group B=47.0%, and group C=38.8%). The proportion of patients treated with minimally invasive management gradually increased over time (group A=35.2%; group B=43.9%; group C=55.0%), while those who underwent surgical management decreased gradually over time (group A=18.3%, group B=9.1%, and group C=6.3%). No differences in mortality rates were observed between the groups.
Conclusions: EPN with medical and minimally invasive management had a relatively high treatment success rate, which increased gradually, while surgical management decreased gradually over time in Korea. The mortality rate was relatively lower than that reported in studies published before the 2010s.
-
Korean Translation of the GRADE Series Published in the BMJ, ‘Use of GRADE Grid to Reach Decisions on Clinical Practice Guidelines When Consensus Is Elusive’ (A Secondary Publication)
-
Hyun Jin Jung, Eu Chang Hwang, Do Kyung Kim, Ho Won Kang, Ja Yoon Ku, Hong Wook Kim, Jae Hung Jung, Guideline Development Committee in the Korean Association of Urogenital Tract Infection and Inflammation
-
Urogenit Tract Infect 2020;15(3):83-89. Published online December 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.3.83
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader ePub ePub
- This article is the last of a series providing guidance for the use of the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system for rating the quality of evidence and grading the strength of recommendations in systematic reviews and clinical practice guidelines. Formulating recommendations with the applicable evidence can be difficult due to the large and diverse nature of guideline committees. This article describes a simple technique called the GRADE grid for clarifying the opinions from guideline panels, dealing with disagreement, and achieving consensus among guideline panels. The grid may be helpful for any guideline groups who want to use GRADE to develop their guidelines and achieve consensus or understand the patterns of uncertainty that surround the interpretation of scientific evidence.
-
Performance of the Sysmex UF-1000i System in Screening for Significant Bacteriuria in Patients with Bladder Cancer Who Received Bacillus Calmette-Guérin Treatment
-
Tae Hee Kim, Seung Il Jung, Myung Soo Kim, Hyun-Jung Choi, Ho Seok Chung, Eu Chang Hwang, Dong Deuk Kwon
-
Urogenit Tract Infect 2020;15(2):38-46. Published online August 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.2.38
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: Diagnosing urinary tract infections by urine culture is time-consuming during a Bacillus Calmette-Guérin treatment. Because the urine culture results take time to collect, patients are treated presumptively, or Bacillus Calmette-Guérin is discontinued before the results. This study evaluated the ability of the Sysmex UF-1000i system to examine the urine bacterial count and determine if it could be used to predict a positive culture.
Materials and Methods: 180 patients who underwent transurethral resection for bladder tumors and received intravesical Bacillus Calmette-Guérin treatment between January 2017 and July 2018 were evaluated prospectively. For patients who received an intravesical Bacillus Calmette-Guérin treatment, urine flow cytometry, and urine cultures were assessed weekly during the treatment period.
Results: During Bacillus Calmette-Guérin instillation, 44, 146, and 27 patients had bacteriuria, pyuria, and positive urine nitrite, respectively. Multivariate analysis indicated that the predictors associated with bacteriuria included the urine flow cytometry results of >100 bacteria/µl (odds ratio, 22.73; p<0.001) and positive urine nitrite (odds ratio, 5.67; p=0.012) at the time of sampling for positive urine culture. The area under the receiver operative characteristic curve for diagnosing bacteriuria by urine flow cytometry was 0.825. A urine flow cytometry cutoff value of >100 bacteria/µl resulted in a sensitivity and specificity of 75% and 90.91%, respectively. Using the cutoff of >1,000 bacteria/µl, the sensitivity and specificity were 50% and 94.85%, respectively.
Conclusions: Rapid urinary tract infection diagnosis using Sysmex UF-1000i can be used to determine whether to treat an infection and to avoid unnecessary Bacillus Calmette-Guérin discontinuation and urine culture tests.
-
Citations
Citations to this article as recorded by  - Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
Ali Bourgi, Omar Ghanem, Camille Brocail, Franck Bruyère
Surgical Infections.2025; 26(6): 390. CrossRef
-
2,075
View
-
2
Download
-
1
Crossref
-
Rates and Risk Factors of Bacteriuria in Patients with Bladder Cancer Who Underwent Treatment with Bacillus Calmette-Guérin
-
Seong Jong Eun, Myung Soo Kim, Seung Il Jung, Hyun-Jung Choi, Ho Seok Chung, Eu Chang Hwang, Dong Deuk Kwon
-
Urogenit Tract Infect 2020;15(2):47-53. Published online August 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.2.47
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study evaluated the rate and predictors of bacteriuria in patients who underwent transurethral resection of bladder tumor (TURBT) and Bacillus Calmette-Guérin (BCG) treatment.
Materials and Methods: We prospectively evaluated 266 patients who underwent TURBT and intravesical BCG treatment between January 2017 and September 2019. Urinalysis and urine culture were performed at the baseline, one to two weeks after TURBT and weekly during the BCG treatment period. The primary outcomes were the bacteriuria rates in BCG-treated patients, while the secondary outcomes were the risk factors of bacteriuria during BCG treatments.
Results: Of the 266 patients, the rate of bacteriuria was 4.5% before TURBT, 5.3% in the postoperative period, and 24.4% in the BCG treatment period. After BCG instillation, urinalysis showed that 204 and 38 patients tested positive for pyuria and nitrite, respectively. Multivariate analysis indicated that the risk factors associated with bacteriuria during BCG treatment included age (odds ratio [OR]: 1.06; p=0.003), sex (female) (OR, 5.41; p=0.007), diabetes mellitus (DM) (OR, 2.82; p=0.023), postoperative bacteriuria (OR, 8.08; p=0.032), bacterial counts>100/µl in urine flow cytometry (OR, 29.72; p<0.001), and positive urine nitrite test (OR, 6.20; p=0.001) at the time of positive urine culture sampling.
Conclusions: Approximately 25% of the patients suffered from bacteriuria during intravesical BCG treatment. Old age, female sex, DM, and postoperative bacteriuria were found to be the risk factors of bacteriuria during BCG treatment. Predictive factors could aid in clinical decisions during BCG treatments as well as decisions on BCG discontinuation.
-
Citations
Citations to this article as recorded by  - Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
Ali Bourgi, Omar Ghanem, Camille Brocail, Franck Bruyère
Surgical Infections.2025; 26(6): 390. CrossRef - MESANE KANSERİ ve ÜRİNER STOMASI OLAN HASTANIN EVDE BAKIMI
Neşe İşcan Ayyıldız
Paramedik ve Acil Sağlık Hizmetleri Dergisi.2024; 5(1): 31. CrossRef - Mesane Kanserinde İntravezikal Bacille Calmette- Guerin (BCG) Uygulaması ve Hemşirenin Sorumlulukları
Ayla YAVUZ KARAMANOĞLU, Ali Ersin ZÜMRÜTBAŞ
Adnan Menderes Üniversitesi Sağlık Bilimleri Fakültesi Dergisi.2023; 7(1): 256. CrossRef
-
4,001
View
-
13
Download
-
3
Crossref
-
Korean Translation of the GRADE Series Published in the BMJ, ‘GRADE: Incorporating Considerations of Resources Use into Grading Recommendations’ (A Secondary Publication)
-
Hong Wook Kim, Jae Hung Jung, Do Kyung Kim, Ho Won Kang, Ja Yoon Ku, Hyun Jin Jung, Eu Chang Hwang, Guideline Development Committee in the Korean Association of Urogenital Tract Infection and Inflammation
-
Urogenit Tract Infect 2020;15(2):57-62. Published online August 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.2.57
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader ePub ePub
- This article is the fifth translation of a GRADE series published in the BMJ for incorporating the considerations of resources use into grading recommendations. Clinical recommendations inevitably involve judgments about the allocation of resources use (costs). Although costs differ from typical healthcare outcomes, such as mortality, morbidity, and quality of life, costs are another potentially important outcome that differs across and within a jurisdiction. A balance sheet is a useful method for determining if the net benefits are worth the incremental costs. Resource use, not just monetary values, should always be presented in an evidence profile. Formal economic modeling may or may not help judge the certainty of the evidence for resource use.
-
Korean Translation of the GRADE Series Published in the BMJ, ‘GRADE: Grading Quality of Evidence and Strength of Recommendations for Diagnostic Tests and Strategies’ (A Secondary Publication)
-
Jae Hung Jung, Do Kyung Kim, Ho Won Kang, Ja Yoon Ku, Hyun Jin Jung, Hong Wook Kim, Eu Chang Hwang, Guideline Development Committee in the Korean Association of Urogenital Tract Infection and Inflammation
-
Urogenit Tract Infect 2020;15(1):16-25. Published online April 30, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.1.16
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader ePub ePub
- This article is the fourth translation of a GRADE series published in the BMJ, which graded the quality of evidence and strength of recommendations for diagnostic tests or strategies, as a comprehensive and transparent approach for developing recommendations. Randomized trials for diagnostic approaches represent the ideal study design for intervention studies. On the other hand, cross-sectional or cohort studies with a direct comparison of the test results with an appropriate reference standard can provide high-quality evidence. The guideline panel must be reminded that the test accuracy is a surrogate for patient-important outcomes, so such studies often provide a low quality of evidence for recommendations regarding diagnostic tests, even when the studies do not have serious limitations. Diagnostic accuracy studies showing that a diagnostic test or strategy improves important patient outcomes will require the availability of effective treatment, reduction of test-related adverse effects or anxiety, or improvement of the patients’ well-being from prognostic information. Therefore, it is important to assess the directness of the test results regarding the consequences of diagnostic recommendations that are important to patients.
-
Korean Translation of the GRADE Series Published in the BMJ, ‘GRADE: Going from Evidence to Recommendations’ (A Secondary Publication)
-
Eu Chang Hwang, Do Kyung Kim, Ho Won Kang, Ja Yoon Ku, Hyun Jin Jung, Hong Wook Kim, Jae Hung Jung, Guideline Development Committee in the Korean Association of Urogenital Tract Infection and Inflammation
-
Urogenit Tract Infect 2019;14(3):99-103. Published online December 31, 2019
-
DOI: https://doi.org/10.14777/uti.2019.14.3.99
-
-
 Abstract Abstract
 PDF PDF
- This article is the third translation of a GRADE series published in the BMJ for developing and presenting recommendations for managing patients. The strength of a recommendation reflects the extent to which we can be confident that desirable effects of an intervention outweigh any undesirable effects. GRADE classifies the strength of recommendations as strong or weak. The strength of recommendation is determined by the balance between desirable and undesirable consequences of alternative management strategies, quality of the evidence, variability in values and preferences, and the appropriate usage of resources.
-
Korean Translation of the GRADE Series Published in the BMJ, ‘GRADE: What Is “Quality of Evidence” and Why Is It Important to Clinicians?’ (A Secondary Publication)
-
Ho Won Kang, Jae Hung Jung, Do Kyung Kim, Ja Yoon Ku, Hyun Jin Jung, Hong Wook Kim, Eu Chang Hwang, Guideline Development Committee in the Korean Association of Urogenital Tract Infection and Inflammation
-
Urogenit Tract Infect 2019;14(2):64-70. Published online August 30, 2019
-
DOI: https://doi.org/10.14777/uti.2019.14.2.64
-
-
 Abstract Abstract
 PDF PDF
- This article is second translation of a GRADE series published in the BMJ to create a highly structured, transparent, and informative system for rating quality of evidence for developing recommendations. The process to develop a guideline, we should formulate a clear question with specification of all outcomes of importance to patients. Grading of Recommendations, Assessment, Development and Evaluation (GRADE) offers four levels of evidence quality: high, moderate, low, and very low for these patient-important outcomes. Randomized trials begin as high quality evidence and observational studies as low quality evidence. Although randomized trials begin as high quality evidence, quality may be downgraded as a result of study limitations (risk of bias), inconsistency (variability in results), indirectness, imprecision (wide confidence intervals), or publication bias. While the quality of evidence derived from observational studies starts at ‘low’ but may be upgraded based on a very large magnitude of effect, a dose-response gradient, and if all plausible biases would reduce an apparent treatment effect.
-
Korean Translation of the GRADE Series Published in the BMJ, ‘GRADE: An Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations’ (A Secondary Publication)
-
Do Kyung Kim, Eu Chang Hwang, Ho Won Kang, Ja Yoon Ku, Hyun Jin Jung, Hong Wook Kim, Jae Hung Jung, Guideline Development Committee in the Korean Association of Urogenital Tract Infection and Inflammation
-
Urogenit Tract Infect 2019;14(1):28-32. Published online April 30, 2019
-
DOI: https://doi.org/10.14777/uti.2019.14.1.28
-
-
 Abstract Abstract
 PDF PDF
- Clinical practice guidelines are statements that include recommendations intended to optimize patient care based on a systematic review of the evidence assessing the benefits and harm of alternative care options. Guideline developers should use an explicit, judicious, and transparent methodology to make trustworthy guidelines. Although there are a variety of frameworks that can help translate enormous medical knowledge into recommendations, the most widely adopted tool for grading the quality of evidence and making recommendations is GRADE (Grading of Recommendations, Assessment, Development and Evaluations). This article is the first translation of a series published in the BMJ with regard to the GRADE Approach for Evidence Based Clinical Practice Guideline Development to provide informative knowledge for moving from evidence to recommendations to Korean guideline developers.
-
Infectious Complications after Prostate Biopsy: A Prospective Multicenter Prostate Biopsy Study
-
Eu Chang Hwang, Ho Song Yu, Seung Il Jung, Dong Deuk Kwon, Sun Ju Lee, Tae-Hyoung Kim, In Ho Chang, Hana Yoon, Bongsuk Shim, Kwang Hyun Kim, Donghyun Lee, Jung-Sik Huh, Dong Hoon Lim, Won Jin Jo, Seung Ki Min, Gilho Lee, Ki Ho Kim, Tae Hwan Kim, Seo Yeon Lee, Seung Ok Yang, Jae Min Chung, Sang Don Lee, Chang Hee Han, Sang Rak Bae, Hyun Sop Choe, Seung-Ju Lee, Hong Chung, Yong Gil Na, Seung Woo Yang, Sung Woon Park, Young Ho Kim, Tae Hyo Kim, Won Yeol Cho, June Hyun Han, Yong-Hyun Cho, U-Syn Ha, Heung Jae Park, The Korean Association of Urogenital Tract Infection and Inflammation (KAUTII)
-
Urogenit Tract Infect 2016;11(1):17-24. Published online April 30, 2016
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: Recent studies have highlighted an increasing trend of infectious complications due to fluoroquinolone-resistant organisms among men undergoing transrectal prostate biopsy. This study evaluated the current incidence of infective complications after trans-rectal prostate biopsy for identification of risk factors in Korean men who received fluoroquinolone prophylaxis.
Materials and Methods: A prospective, multicenter study was conducted in Korea from January to December 2015. Prostate biopsies performed with fluoroquinolone prophylaxis during 3 months in each center were included. A pre-biopsy questionnaire was used for identification of patient characteristics. Clinical variables including underlying disease, antibiotic prophylaxis, enema, povidoneiodine cleansing of the rectum, and infectious complications were evaluated. The primary outcome was the post-biopsy infection rate after fluoroquinolone prophylaxis. Univariable and multivariable analyses were used for identification of risk factors for infectious complications.
Results: The study included 827 patients, of whom 93 patients (11.2%) reported receiving antibiotics in the previous 6 months and 2.5% had a history of prostatitis. The infectious complication rate was 2.2%. Post-biopsy sepsis was reported in 2 patients (0.2%). In multivariable analysis predictors of post-biopsy sepsis included person performing biopsy (adjusted odds ratio [OR], 4.05; 95% confidence interval [CI], 1.31-12.5; p=0.015) and operation history within 6 months (adjusted OR, 5.65; 95% CI, 1.74-18.2; p=0.004).
Conclusions: The post-prostate biopsy infectious complication rate in this study was 2.2%. Person performing biopsy (non-urologists) and recent operation history were independent risk factors for infectious complications after trans-rectal prostate biopsy.
-
Risk Factors of Infectious Complications after Transurethral Prostate Surgery in Patients with Preoperative Sterile Urine
-
Eu Chang Hwang, Seong Hyeon Yu, Jong Beom Kim, Seung Il Jung, Taek Won Kang, Dong Deuk Kwon, Kwangsung Park
-
Korean J Urogenit Tract Infect Inflamm 2013;8(1):27-31. Published online April 30, 2013
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: To determine the risk factors of infectious complications after transurethral surgery of the prostate in patients with sterile urine.
Materials and Methods: A total of 183 patients who underwent transurethral resection of the prostate or holmium laser enucleation of the prostate were reviewed. All patients had urinalyses and urine cultures preoperatively, on the day of catheter removal, and at two weeks postoperatively. Patients were divided into two groups according to whether preoperative urinalysis showed sterile urine (group I, n=99) or not (group II, n=84). Clinical parameters were compared between the two groups. Univariate and multivariate logistic regression were used for estimation of infectious complications after surgery in group I.
Results: Compared with group II, group I showed younger age, fewer post voided residuals, low prostate specific antigen levels, short-term duration of oral antibiotic therapy, and low incidence of infectious complications (p<0.05). In univariate analysis in group I, age, diabetes mellitus (DM), prostate volume, resection weight, and duration of oral antibiotic therapy showed an association with infectious complications (p<0.05). Factors showing independent association with infectious complications in group I were DM (odds ratio [OR], 7.31; 95% confidence interval [CI], 1.83-29.0; p=0.005), resection weight (OR, 1.03; 95% CI, 1.01-1.06; p=0.039), and duration of oral antibiotics (OR, 0.64; 95% CI, 0.43-0.94; p=0.025).
Conclusions: Kinds of antibiotics showed no effect on infectious complication, therefore, second generation cephalosporin is recommended for reduction of antibiotic resistance. Clinicians should be aware of the high risk for infectious complication in patients with DM and who underwent large volume resection of the prostate.
-
Clinical Study According to Presence of Prior Manipulation in Patients with Acute Bacterial Prostatitis
-
Kwang Ho Kim, Eu Chang Hwang, Sun Ouck Kim, Seung Il Jung, Taek Won Kang, Dong Deuk Kwon, Kwang Sung Park
-
Korean J Urogenit Tract Infect Inflamm 2012;7(2):172-177. Published online October 31, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: Acute bacterial prostatitis (ABP) is uncommon and proper guidelines concerning antibiotic administration for ABP with urologic procedure are unclear. We retrospectively analyzed clinical symptoms and etiologic organism in ABP according to presence of prior urologic manipulation.
Materials and Methods: The clinical records of 65 patients who had been treated for ABP between January 2007 and December 2011 were reviewed. We analyzed parameters including history taking, physical examination, prior manipulations, antibiotics administration, mean length of treatment, complications, urinalysis, and urine and blood culture. Results were analyzed according to two subgroups; Group 1, those without prior urologic manipulation, and Group 2, those with prior manipulation.
Results: The population of Group 1 was 22 (33.8%) and Group 2 was 43 (66.2%). The mean age of the patients in both groups were 56.5±15.6 years and 64.0±12.5 years, respectively. Of the clinical symptoms in both groups, fever was most common (81.8% and 83.7%). The mean pyuria grades were 2.82±0.37 and 3.47±0.25 each in both groups. In group 2, prostatic biopsy (36, 83.7%) was the most frequent manipulation of the patients. Dysuria and storage symptoms were significantly more frequent in Group 1. The number of diabetes mellitus patients and the admission rates were higher in Group 2. E. coli was the most frequently isolated pathogen from urine and blood (23.1% and 24.6%, respectively). Resistance to ciprofloxacin was very high in group 1 (60.0%) and group 2 (83.3%). However, there was no significant difference between the two groups.
Conclusions: Resistance rates to ampicillin and ciprofloxacin in ABP were very high in all patients. The resistance rates were higher in patients with prior manipulation, but there was no significant difference. When we consider high resistance to ciprofloxacin in ABP, more careful attention should be paid to empirical treatment of ABP patients with prior manipulation. (Korean J UTII 2012;7:172-177)
-
Prophylactic Effectiveness of Second Generation Cephalosporin According to Prostatic Operation Methods
-
Seong Woong Na, Eu Chang Hwang, Seung Il Jung, Dong Deuk Kwon, Kwangsung Park, Soo Bang Ryu
-
Korean J Urogenit Tract Infect Inflamm 2011;6(2):171-177. Published online October 31, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: There is no definitive standard concerning the use of prophylactic antibiotics for prostatic operations, except for transurethral resection of prostate (TUR-P). This study prospectively investigated the prophylactic effectiveness of a second generation cephalosporin according to prostatic operation method. Materials and Methods: From October 2010 to January 2011, prostatic operations were conducted for 67 patients: group I (radical prostatectomy, n=18), group II (TUR-P, n=38), group III (laser TUR-P, n=11) for 11: group III). Prophylactic antibiotics were intravenously administered beginning 1 hour preoperatively and orally with several days postoperatively. Prophylactic effectiveness was evaluated by comparison of urine analysis and presence of bacteriuria. Results: In group I, no patient had preoperative Foley catheter installation, and mean antibiotic prescription period pre- and post-operatively was 5.83 days and 6.94 days. Five group I patients (27.8%) displayed bacteriuria. In group II, 9 patients had preoperative Foley catheter installation and mean antibiotic prescription period was 3.76 days and 5.68 days, respectively. Five patients (13.2%) had postoperative bacteriuria; two in preoperative catheterized patients and three in preoperative non-catheterized patients. In group III, mean antibiotic prescription period was 1.73 days and 5.09 days, respectively. There was no postoperative bacteriuria. Conclusions: Prophylactic use of a second generation cephalosporin for prostatic operation, except laser TUR-P, was limited in preventing postoperative pyuria with bacteriuria. There was a tendency of higher occurrence of postoperative bacteriuria in patients with preoperative Foley catheter installation."
-
Clinical Features of Bacteremia Caused by Ciprofloxacin-Resistant Bacteria after Transrectal Ultrasound-Guided Prostate Biopsy
-
Bo Sung Shin, Eu Chang Hwang, Seung Il Jung, Dong Deuk Kwon, Kwangsung Park, Soo Bang Ryu, Jin Woong Kim
-
Korean J Urogenit Tract Infect Inflamm 2011;6(1):61-66. Published online April 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: Fluoroquinolone is considered the prophylactic antibiotic of choice for Transrectal ultrasound (TRUS)-guided biopsy. However, failure of quinolone prophylaxis due to emerging quinolone-resistant enterobacteriae has been increasing. We reviewed bacteremia cases after TRUS-guided biopsy to identify antibiotic-resistant bacterial strains with the objective to prevent urosepsis. Materials and Methods: A total of 2,348 patients underwent TRUS-guided biopsy at our institution between January 2004 and December 2009. All patients received intravenous ciprofloxacin for prophylaxis. We retrospectively evaluated patients who developed infectious symptoms, such as fevers and chills. Results: Eleven (0.4%) of 2,348 patients developed infectious symptoms. Escherichia coli was the pathogen responsible for post-biopsy infections occurring in a; 11 (100%) patients with positive blood cultures, which confirmed ciprofloxacin-resistant E. coli, with one isolate producing extended-spectrum beta lactamase. Ten out of 11 E. coli isolates (91%) were resistant to ampicillin and 9 of 11 E. coli isolates (82%) were resistant to gentamicin. Ten out of 11 E. coli isolates (91%) were susceptible to third generation cephalosporins. All such patients were admitted to the hospital and treated with a third generation cephalosporin. One patient who habored an E. coli isolate producing extended-spectrum beta-lactamase received imipenem. Conclusions: Ciprofloxacin is effective in reducing infectious complications. However, recently, bacteremiccases are increasing due to ciprofloxacin resistant E. coli. For patients with infectious symptoms after transrectal prostate biopsy, early antibiotics change, including third generation cephalosporins, are recommended to prevent urosepsis."
-
Fournier’s Gangrene: Six Years of Experience with 33 Patients and Validity of the Fournier’s Gangrene Severity Index Score in Korean Patients
-
Eu Chang Hwang, Seong Woong Na, Young Jung Kim, Jun Seok Kim, Sun-Ouck Kim, Seung Il Jung, Dong Deuk Kwon, Kwangsung Park, Soo Bang Ryu, Lu Ji Wan
-
Korean J Urogenit Tract Infect Inflamm 2010;5(2):199-206. Published online October 31, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: To identify predictive factors of survival in patients with Fournier’s gangrene (FG), and to determine the validity of the Fournier’s Gangrene Severity Index Score (FGSIS) in Korean patients. Materials and Method: Thirty-three patients with FG were enrolled. Data were collected regarding medical history, symptoms, physical examination findings, admission laboratory tests, and the extent of body surface area involved (%). The FGSIS, which was developed to assign a numerical score that describes the disease acuity, was used in our study. The data were assessed based on whether or not the patient had survived. Results: Of the 33 patients, 16 survived (48.5%, Group I) and 17 died (51.5%, Group II). Isolated FGSIS and admission laboratory parameters that were statistically different in the two groups included heart rate (p=0.009), white blood cell count (WBC; p=0.035), and serum calcium (p=0.001). The mean body surface area in Group II was statistically different from that of Group I (6.4% vs. 2.4%, p=0.001). The mean FGSIS for groups I and II was 6.6±3.7 and 8.2±4.1, respectively (p=0.26). Based on univariate regression analysis, disease severity had no correlation with the FGSIS. However, isolated parameters, including heart rate, WBC count, serum total calcium level, and the extent of body surface area involved was associated with disease severity. Conclusions: Although the FGSIS was not shown to be a predictive factor for disease severity, metabolic parameters and the extent of body surface area involved appeared to be important factors for predicting FG severity."
-
Candida Infection Accompanying Glans Necrosis in Diabetic Patient
-
Bo sung Shin, Hyunchong Ki, Eu chang Hwang, Chang Min Im, Sook Jung Yun, Seung IL Jung, Dong Deuk Kwon
-
Korean J Urogenit Tract Infect Inflamm 2010;5(1):93-96. Published online April 30, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- Candida albicans is considered to be responsible for up to 35% of all cases of infectious balanitis. We report a man with glans necrosis with candidal infection. A 56 year old man visited our institute to consult for penile pain and black colored glans of penis. He had noted two months earlier due to gradually increased wounds, resulting in voiding difficulty. On the physical examination, there was hard necrotic lesion on the glans of penis with secondary meatal stenosis. Tissue culture and biopsy suggested candidial infection. We review the literature on the different forms of presentation of this condition and the differential diagnosis of ischemic penile lesions.
-
Retroperitoneal Fibrosis with Spontaneous Subcapsular Renal Hemorrhage Treated with Medical Thearpy
-
Eu Chang Hwang, Ho Suck Chung, Chang Min Im, Seung Il Jung, Dong Deuk Kwon, Kwangsung Park, Soo Bang Ryu, Jun Eul Hwang1
-
Korean J Urogenit Tract Infect Inflamm 2009;4(1):86-88. Published online April 30, 2009
-
-
-
 Abstract Abstract
 PDF PDF
- Spontaneous subcapsular renal hemorrhage is relative uncommon. The literature suggests that the majority causes for this phenomenon associated with disease of the kidney, blood vessel disease, blood dyscrasia. We report a unique case of retroperitoneal fibrosis combined with subcapsular renal hemorrhage. The patient was successfully treated with medical therapy.
|