Search
- Page Path
- HOME > Search
Review Articles
- Adult Syphilis: A Narrative Review of Clinical Insights and Public Health Implications in Urology
- Seung-Ju Lee, Jin Bong Choi
- Urogenit Tract Infect 2025;20(3):123-131. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550039017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
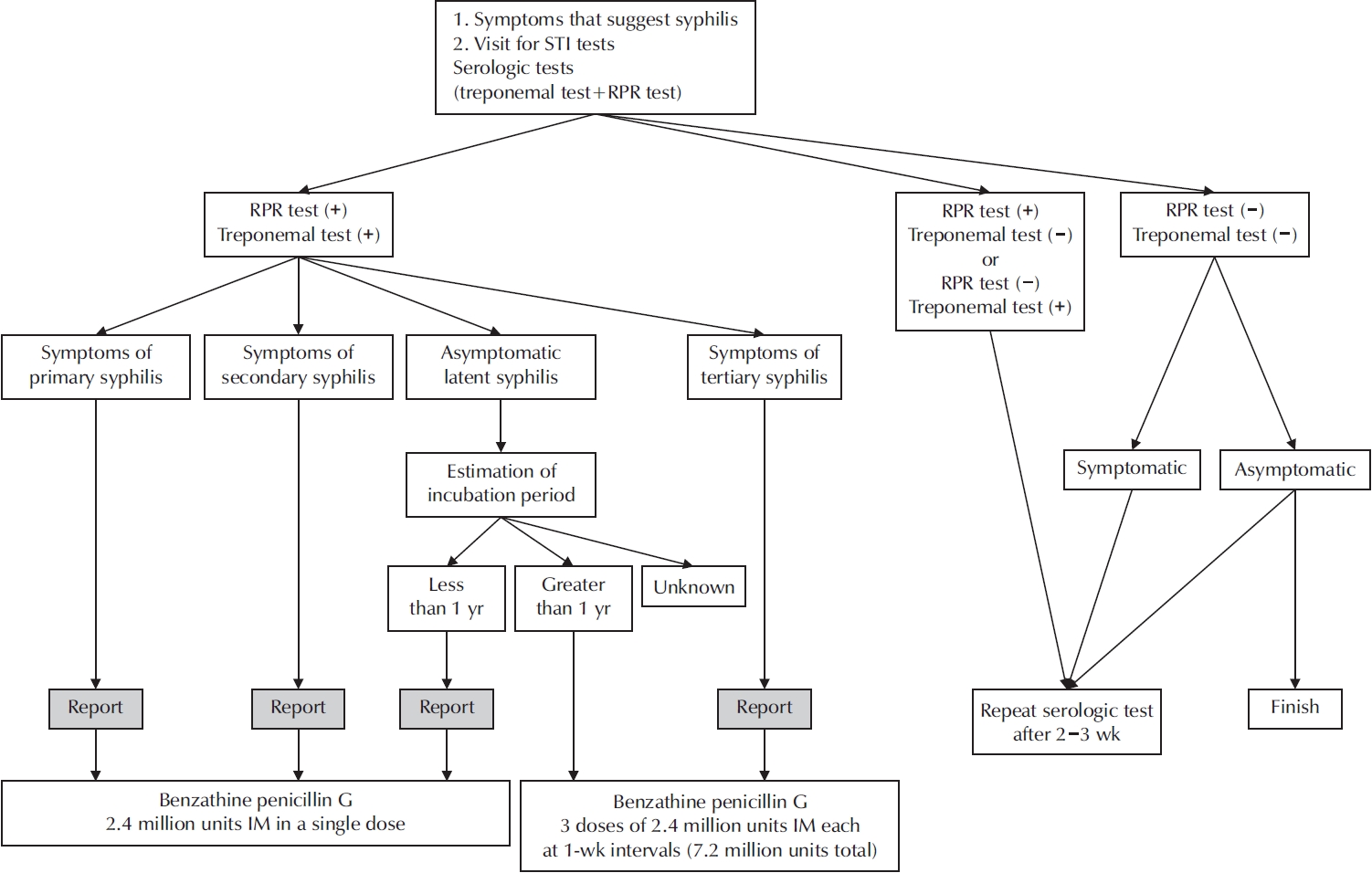
ePub - Syphilis continues to pose a major global public health concern, with more than 7 million cases reported worldwide in 2022, and its incidence continues to rise in numerous regions. In Korea, the shift from sentinel to universal notification in 2024 has revealed a markedly greater disease burden, particularly among men who have sex with men and among younger adults, underscoring changing epidemiological patterns and the urgent need for revised control strategies. In urological practice, syphilis presents with a wide range of often misleading symptoms, including painless genital ulcers, urethritis, and sexual dysfunction, that frequently resemble other genitourinary disorders and complicate diagnostic evaluation. Accurate identification relies on integrating a thorough clinical assessment with serologic testing while remaining alert to diagnostic challenges such as early latent infection, serofast states, and human immunodeficiency virus coinfection. Penicillin G remains the mainstay of therapy, with treatment regimens tailored to the stage of disease and to the presence or absence of central nervous system involvement. Effective partner notification, targeted screening, and consistent follow-up are essential to prevent reinfection and limit further transmission. At a public health level, a multifaceted strategy—strengthened surveillance systems, focused testing in high-risk populations, and embedding syphilis screening within broader sexually transmitted infection care frameworks—is critical to curbing its resurgence. In summary, prompt recognition, adherence to evidence-based management, and coordinated public health measures, together with ongoing advances in diagnostics and prevention, remain fundamental to reducing the continued spread of syphilis and mitigating its impact on both individual and population health.
- 581 View
- 9 Download

- A Narrative Review of Syphilis Notification Systems in Korea: Change to Mandatory Surveillance System
- Seung-Ju Lee, Jin Bong Choi
- Urogenit Tract Infect 2025;20(1):28-33. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550004002
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
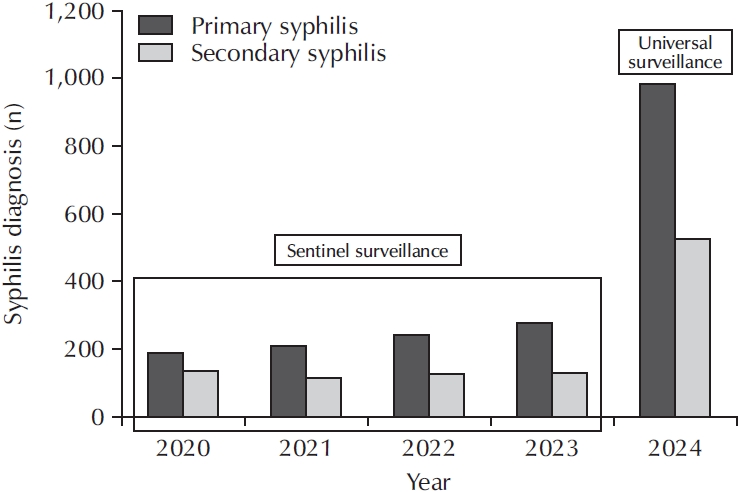
ePub - New cases of syphilis are clearly showing an increasing trend worldwide. However, in a sentinel surveillance system, the collection of information on disease outbreaks is limited, making it difficult to understand the overall outbreak situation and perform detailed analyses of patients' demographic characteristics and disease stages. In accordance with the revision of the Infectious Disease Prevention Act, syphilis was converted from a grade 4 infectious disease subject to sentinel surveillance to a grade 3 infectious disease subject to mandatory surveillance from January 1, 2024, with all medical institutions required to report syphilis diagnosis within 24 hours.
-
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Adult Syphilis: A Narrative Review of Clinical Insights and Public Health Implications in Urology
Seung-Ju Lee, Jin Bong Choi
Urogenital Tract Infection.2025; 20(3): 123. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,279 View
- 38 Download
- 2 Crossref

Original Article
- Trend Analysis of Sexually Transmitted Infection Treatments in Korea
- Soeon Park, Byung Kyu Han, Sangrak Bae, Seung-Ju Lee, Jin Bong Choi
- Urogenit Tract Infect 2024;19(2):25-30. Published online August 31, 2024
- DOI: https://doi.org/10.14777/uti.2024.19.2.25
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: The revision of the 2023 Guidelines for the Treatment of Sexually Transmitted Infections (STIs) has been released. Hence, it is necessary to analyze the current status of STI treatments in Korea.
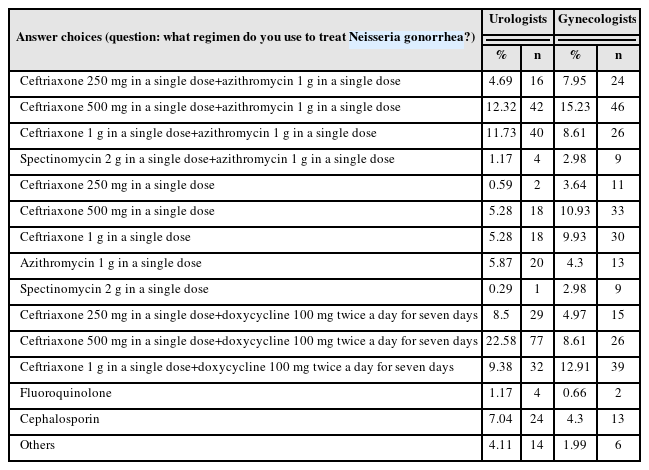
Materials and Methods: A questionnaire was distributed to urologists and gynecologists from December 2022 to January 2023 through an online survey program. Three hundred and forty-one urologists and 302 gynecologists responded to the questionnaire.
Results: For Neisseria gonorrhea treatment, ceftriaxone 500 mg and 100 mg of doxycycline twice daily for seven days were most preferred by urologists (22.58%). The treatment most preferred by gynecologists (15.23%) was 500 mg of ceftriaxone and 1 g of azithromycin in a single dose. Both urologists and gynecologists generally treat Chlamydia trachomatis according to the treatment guidelines. For treating Mycoplasma genitalium, 29.03% of urologists preferred administering azithro-mycin at 500 mg once daily, followed by 250 mg for four days. In contrast, 33.11% of gynecologists preferred doxycycline 100 mg twice daily for seven days.
Conclusions: Most urologists and gynecologists followed the treatments recommended in the 2nd edition of the STI treatment guidelines, revised in 2016. As many treatment regimens have changed because of the recent increase in antibiotic-resistant STIs, there is a need to encourage them to follow the new treatment guidelines. -
Citations
Citations to this article as recorded by- Comparative Study of the Clinical Characteristics of Patients With Sexually Transmitted Infections Diagnosed by Nucleic Acid Amplification Tests
Jung Soo Son, Namhee Kim, Hong Sang Oh, Sang Won Park, Dong Hoon Shin
Journal of Korean Medical Science.2025;[Epub] CrossRef
- Comparative Study of the Clinical Characteristics of Patients With Sexually Transmitted Infections Diagnosed by Nucleic Acid Amplification Tests
- 6,766 View
- 36 Download
- 1 Crossref

Reviews
- Healthcare-Associated Urinary Tract Infection: Multi Drug Resistance and Risk Factors
- Jin Bong Choi, Seung-Ju Lee
- Urogenit Tract Infect 2018;13(2):21-25. Published online August 31, 2018
-
 Abstract
Abstract
 PDF
PDF - A new category of infections called healthcare-associated (HCA) infections was created due to increased procedures performed in outpatient clinics of hospitals. The risk of HCA infections is on the rise as the use of long-term care facilities (LTCFs) is increasing. HCA-urinary tract infection (UTI) is one of the most frequently occurring bacterial infections. In clinical and microbiological analyses, HCA-UTI is similar to hospital-acquired-UTI. The prevalence of multidrug-resistant (MDR) organisms in HCA-UTI has increased and is varied according to the type of LTCFs and regions. Finally, prior investigations reported the association between several risk factors and MDR acquisition, which vary considerably according to study design. Therefore, additional research is needed to develop a more accurate methodology.
- 391 View
- 2 Download

- The Clinical Guidelines for Acute Uncomplicated Cystitis and Acute Uncomplicated Pyelonephritis
- Ki Ho Kim, Jae Heon Kim, Seung-Ju Lee, Hong Chung, Jae Min Chung, Jae Hung Jung, Hyun Sop Choe, Hun Choi, Sun-Ju Lee, The Committee of The Korean Association of Urogenital Track Infection and Inflammation
- Urogenit Tract Infect 2017;12(2):55-64. Published online August 31, 2017
-
 Abstract
Abstract
 PDF
PDF - To date, there has not been an establishment of guidelines for urinary tract infections, due to limited domestic data in Korea, unlike other North American and European countries. The clinical characteristics, etiology, and antimicrobial susceptibility of urinary tract infections vary from country to country. Moreover, despite the same disease, antibiotic necessary to treat it may vary from country to country. Therefore, it is necessary to establish a guideline that is relevant to a specific country. However, in Korea, domestic data have been limited, and thus, guidelines considering the epidemiological characteristics pertaining specifically to Korea do not exist. Herein, describe a guideline that was developed by the committee of The Korean Association of Urogenital Tract Infection and Inflammation, which covers only the uncomplicated urinary tract infections, as covering all parts in the first production is difficult.
- 1,090 View
- 6 Download

Original Article
- The Antibiotic Susceptibility of Escherichia coli from Community-Acquired Uncomplicated Urinary Tract Infection: A Focused on Fosfomycin
- Hyun-Sop Choe, Seung-Ju Lee, In Ho Chang, Tae-Hyoung Kim, Hong Chung, Jae Min Chung, Sang Don Lee, Jae Hung Jung, Ki Ho Kim, Seung Ki Min, Yong Gil Na, Hana Yoon, Ho Song Yu, Mi-Kyung Lee, Sun-Ju Lee
- Urogenit Tract Infect 2017;12(2):77-81. Published online August 31, 2017
-
 Abstract
Abstract
 PDF
PDF - Purpose: To assess the antibiotic susceptibility of Escherichia coli from community-acquired uncomplicated urinary tract infection (UTI).
Materials and Methods: Between August and December of 2015, confirmed cases of E. coli as a pathogen of community-acquired uncomplicated UTI were collected and assessed for antibiotic susceptibility in 10 designated hospitals. Additional fosfomycin susceptibility test was performed by a central laboratory using the disk diffusion method.
Results: A total of 347 E. coli isolates were collected from urine samples of community-acquired uncomplicated UTIs patients. The susceptibility rates of antibiotics were as follows: amikacin 100.0% (347), imipenem 100.0% (347), ciprofloxacin 57.1% (198), cefotaxime 74.9% (260), ampicillin 30.0% (104), trimethoprim/sulfamethoxazole 66.9% (232), and fosfomycin 98.0% (340). All fosfomycin-resistant E. coli isolates were extended-spectrum β-lactamase (ESBL)-producing. In 85 cases of ESBL-producing E. coli, the fosfomycin susceptibility rate was 91.8% (78/85).
Conclusions: Fosfomycin may be a useful option for the treatment of community-acquired uncomplicated UTIs. Further studies evaluating the role of fosfomycin in the treatment of UTIs and its clinical efficacy are necessary.
- 392 View
- 0 Download

Reviews
- 2017 Guidelines of The Korean Association of Urogenital Tract Infection and Inflammation: Acute Uncomplicated Cystitis
- Ki Ho Kim, Seung-Ju Lee, Yong-Hyun Cho, Hyun-Sop Choe, Yong Gil Na, Jae Heon Kim, Hong Chung, Jae Min Chung, Jae Hung Jung, Hoon Choi, Sun-Ju Lee
- Urogenit Tract Infect 2017;12(1):3-6. Published online April 30, 2017
-
 Abstract
Abstract
 PDF
PDF - Acute uncomplicated cystitis is the most common urinary tract infection that mainly occurs in adult females, particularly sexually active young women and postmenopausal women. It is commonly observed in primary health care settings, including urology as well as obstetrics and gynecology; more than half of healthy adult women visit clinics and hospitals at least once in their lifetime due to acute uncomplicated cystitis. The most common bacterium causing this condition is Escherichia coli, followed by Staphylococcus saprophyticus, Klebsiella pneumoniae, Proteus mirabilis, and etc. Trimethoprim-sulfamethoxazole or fluoroquinolones have been used as an empirical antibiotic treatment. However, as fluoroquinolone-resistant organisms or extended spectrum beta-lactamase-producing organisms are becoming more prevalent worldwide, information on regional antibiotic resistance and guidelines on antibiotic use are becoming increasingly more desparate.
- 826 View
- 4 Download

- 2017 Guidelines of The Korean Association of Urogenital Tract Infection and Inflammation: Recurrent Urinary Tract Infection
- Seung-Ju Lee, Hyun-Sop Choe, Yong Gil Na, Ki Ho Kim, Jae Heon Kim, Hong Chung, Jae Min Chung, Jae Hung Jung, Hoon Choi, Sun-Ju Lee, Yong-Hyun Cho
- Urogenit Tract Infect 2017;12(1):7-14. Published online April 30, 2017
-
 Abstract
Abstract
 PDF
PDF - Recurrent infection after an acute urinary tract infection (UTI) episode is common in adult women. It is onerous to both the patient and the physician to treat frequent recurrent UTI. Every time when UTI recurs, patients experience lower urinary tract symptoms, fatigue, and limitation in everyday life, while the physician has difficulty in counseling patients with a disease entity whose pathophysiology is less known. Currently, prophylactic treatment for recurrent UTI is limited, is ineffective in most cases, and sometimes accompanies unexpected side effects. In this guideline, we aimed to establish feasible and effective recommendations for the treatment of recurrent UTI in healthy adult women.
- 543 View
- 4 Download

- National Trends of Antimicrobial Resistance in Uncomplicated Cystitis
- Hyun-Sop Choe, Seung-Ju Lee
- Urogenit Tract Infect 2016;11(1):7-11. Published online April 30, 2016
-
 Abstract
Abstract
 PDF
PDF - Acute uncomplicated cystitis is a common bacterial infection of the urinary bladder in women. Antibiotic resistance against Escherichia coli is increasing nationwide in Korea; therefore, we reviewed the local available data regarding acute cystitis. The recently determined susceptibilities of E. coli to gentamicin, fluoroquinolone, 3rd generation cephalosporin, and amikacin are 75%, 85-95%, 95%, and 97%, respectively. The resistance rates of E. coli to trimethoprim/sulfamethoxazole, fluoroquinolone, and even 3rd generation cephalosporin are higher in Korea compared with other countries, however, the studies that determined those resistance rates included data collected at tertiary referral hospitals, which may have been overestimated. Continuous monitoring of antibiotic resistance and opportune establishment and revision of treatment guidelines are required for the optimal management of acute cystitis.
- 477 View
- 1 Download

Original Article
- Infectious Complications after Prostate Biopsy: A Prospective Multicenter Prostate Biopsy Study
- Eu Chang Hwang, Ho Song Yu, Seung Il Jung, Dong Deuk Kwon, Sun Ju Lee, Tae-Hyoung Kim, In Ho Chang, Hana Yoon, Bongsuk Shim, Kwang Hyun Kim, Donghyun Lee, Jung-Sik Huh, Dong Hoon Lim, Won Jin Jo, Seung Ki Min, Gilho Lee, Ki Ho Kim, Tae Hwan Kim, Seo Yeon Lee, Seung Ok Yang, Jae Min Chung, Sang Don Lee, Chang Hee Han, Sang Rak Bae, Hyun Sop Choe, Seung-Ju Lee, Hong Chung, Yong Gil Na, Seung Woo Yang, Sung Woon Park, Young Ho Kim, Tae Hyo Kim, Won Yeol Cho, June Hyun Han, Yong-Hyun Cho, U-Syn Ha, Heung Jae Park, The Korean Association of Urogenital Tract Infection and Inflammation (KAUTII)
- Urogenit Tract Infect 2016;11(1):17-24. Published online April 30, 2016
-
 Abstract
Abstract
 PDF
PDF - Purpose: Recent studies have highlighted an increasing trend of infectious complications due to fluoroquinolone-resistant organisms among men undergoing transrectal prostate biopsy. This study evaluated the current incidence of infective complications after trans-rectal prostate biopsy for identification of risk factors in Korean men who received fluoroquinolone prophylaxis.
Materials and Methods: A prospective, multicenter study was conducted in Korea from January to December 2015. Prostate biopsies performed with fluoroquinolone prophylaxis during 3 months in each center were included. A pre-biopsy questionnaire was used for identification of patient characteristics. Clinical variables including underlying disease, antibiotic prophylaxis, enema, povidoneiodine cleansing of the rectum, and infectious complications were evaluated. The primary outcome was the post-biopsy infection rate after fluoroquinolone prophylaxis. Univariable and multivariable analyses were used for identification of risk factors for infectious complications.
Results: The study included 827 patients, of whom 93 patients (11.2%) reported receiving antibiotics in the previous 6 months and 2.5% had a history of prostatitis. The infectious complication rate was 2.2%. Post-biopsy sepsis was reported in 2 patients (0.2%). In multivariable analysis predictors of post-biopsy sepsis included person performing biopsy (adjusted odds ratio [OR], 4.05; 95% confidence interval [CI], 1.31-12.5; p=0.015) and operation history within 6 months (adjusted OR, 5.65; 95% CI, 1.74-18.2; p=0.004).
Conclusions: The post-prostate biopsy infectious complication rate in this study was 2.2%. Person performing biopsy (non-urologists) and recent operation history were independent risk factors for infectious complications after trans-rectal prostate biopsy.
- 819 View
- 3 Download

Review Article
- HIV Infection in Urological Practice
- Seung-Ju Lee
- Korean J Urogenit Tract Infect Inflamm 2011;6(2):140-154. Published online October 31, 2011
-
 Abstract
Abstract
 PDF
PDF - This review evaluates the scientific evidence suggesting that urological factors increase the efficiency of human immunodeficiency virus (HIV) transmission and discusses the important urological manifestations of HIV infection. Level 1 evidence suggests that sexually transmitted infections (STIs) are substantially associated with an increased risk of HIV infection. Several randomized controlled trials show that improved STI control can play a vital role in comprehensive programs to prevent sexual transmission of HIV. However, there is limited evidence that control of STIs reduces HIV incidence at a population level. HIV has become a chronic manageable condition thanks to highly active antiretroviral therapy. Urologists face a challenge in trying to manage the genitourinary manifestations of HIV infection.
- 378 View
- 2 Download

Clinical Guideline Review
- The New Korean Guideline for Sexually Transmitted Infections
- Dong-Hoon Lim, Seung-Ju Lee, Bongsuk Shim, Chul-Sung Kim, Min Eui Kim, Yong-Hyun Cho
- Korean J Urogenit Tract Infect Inflamm 2011;6(1):96-113. Published online April 30, 2011
-
 Abstract
Abstract
 PDF
PDF - Sexually transmitted infections (STIs) are increasing worldwide. To have a well-designed localized guideline on STIs is crucial in controlling the condition. We reviewed the newly developed Korean STI guideline, 2011 that will provide comprehensive information regarding STI management.
- 452 View
- 0 Download

Review Articles
- Treatment and Prevention of Catheter-Associated Urinary Tract Infections
- Seung Hyuk Yim, U-Syn Ha, Dong Wan Sohn, Seung-Ju Lee, Chang Hee Han, Choong Bum Lee, Yong-Hyun Cho
- Korean J Urogenit Tract Infect Inflamm 2009;4(2):159-169. Published online October 31, 2009
-
 Abstract
Abstract
 PDF
PDF - Urinary tract infections (UTIs) represent the second most often observed infectious diseases in community, following the respiratory tract infections. Approximately 40% of nosocomial infections originate in the urinary tract; about 80% of urinary tract infections is related to urinary catheterization. The duration of catheterization is the most important risk factor for development of UTIs and additional risk factors include female sex, diabetes mellitus, renal function impairment, lack of antimicrobial therapy, and not maintaining a closed drainage system. There are many methods for preventing catheter-associated urinary tract infections (CAUTI); (i) an indwelling catheter should be introduced under antiseptic conditions; (ii) urethral trauma should be minimized by the use of adequate lubricant and the smallest possible catheter; (iii) the catheter system should remain closed; and (iv) the duration of catheterization should be minimal. Antimicrobial urinary catheters can prevent or delay the onset of CAUTI, but the effect on morbidity is not known. Antibiotic treatment is recommended only in symptomatic infection (bacteremia, pyelonephritis, epididymitis, prostatitis), but systemic antimicrobial treatment of asymptomatic CAUTI is only recommended in the following circumstances; (i) patients undergoing urological surgery or implantation of prosthesis; (ii) treatment may be part of a plan to control nosocomial infection due to a particularly virulent organism prevailing in a treatment unit; (iii) patients who have a high risk of serious infectious complications; and (iv) infections caused by strains causing a high incidence of bacteremia.
- 424 View
- 3 Download

- Current Status of Antimicrobial Resistance among Bacterial Pathogens Causing Urinary Tract Infection in Korea
- Seung-Ju Lee
- Korean J Urogenit Tract Infect Inflamm 2009;4(1):37-46. Published online April 30, 2009
-
 Abstract
Abstract
 PDF
PDF - Antimicrobial resistance among bacterial pathogens causing urinary tract infection (UTI) is a leading concern, with a high level of Gram-negative organisms resistant to trimethoprim/sulfamethoxazole and fluoroquinolones in Korea. The Korean Association of Urogenital Tract Infection and Inflammation has conducted multicenter surveillance studies for antimicrobial resistance since 2002. The present article reviews the current status of antimicrobial resistance among uropathogens in Korea based on the last 2008 study. Main etiologic pathogens of community-acquired UTI were E. coli (60.0%), E. faecalis (10.2%) and K. pneumoniae (4.1%). Nosocomial pathogens causing UTI were E. coli (38.7%), K. pneumoniae (15.1%) and P. aeruginosa (6.5%). Community-acquired UTIs were divided by uncomplicated UTI and complicated UTI. These are categorized by uncomplicated cystitis, uncomplicated pyelonephritis, complicated UTI with pyelonephritis and complicated UTI without pyelonephritis. Ciprofloxacin resistance rates in community-acquired E. coli were 24.8%, 18.4%, 25.0% and 40.9% for each category, respectively. In contrast, nosocomial E. coli showed higher resistance rate (76.4%) against ciprofloxacin. Among E. coli isolates form uncomplicated cystitis, the resistance rates to TMP/SMX, cefuroxime, cefpodoxime and amikacin were 32.4%, 9.9%, 6.4% and 0.3%, respectively. The concordance rate of the empirical antimicrobial agents were 66.7% in nosocomial UTI and 86.3% in community-acquired UTI. Among E. coli and K. pneumoniae isolates, 9.9% and 22.8% were extended spectrum β-lactamase (ESBL) producers, respectively. These results demonstrated that several uropathogens isolated in Korea have high resistance to various classes of antimicrobial agents. Fluoroquinolone-resistant E. coli and ESBL-producing K. pneumoniae constitute serious problem for UTI in Korea.
- 698 View
- 2 Download

Original Article
- Expression of Multidrug Resistance of Ciprofloxacin-Resistant Escherichia coli from Outpatients with Uncomplicated Cystitis
- Choong Bum Lee, Dae Haeng Cho, Moon Soo Chung, Seung-Ju Lee
- Korean J Urogenit Tract Infect Inflamm 2009;4(1):80-85. Published online April 30, 2009
-
 Abstract
Abstract
 PDF
PDF - "Purpose: Currently, the prevalence of fluoroquinolone-resistant isolates of uropathogens has been reported to be increasing over time in some centers in Korea. We determined the in vitro susceptibilities of collected ciprofloxacin-resistant urine isolates of Escherichia coli (E. coli) from outpatients to other oral antimicrobial agents used for the treatment of acute cystitis. Materials and Methods: From January 2007 to December 2008, a total of 150 ciprofloxacin-resistant E. coli isolates from urine specimens from outpatients with acute cystitis were collected from 5 university hospitals in Korea. Clinical and Laboratory Standards Institute-specified broth microdilution testing was performed with amoxicillin/clavulanate, ampicillin, cefuroxime, cefpodoxime, and trimethoprim/sulfamethoxazole (TMP/SMX). Results: Ciprofloxacin-resistant E. coli isolates were frequently resistant to ampicillin (84.6% of isolates) and TMP/SMX (63.4%); concurrent resistance to amoxicillin/clavulanate (10.0%) or cefpodoxime (6.6%) was less common. Only 6.6% of isolates was resistant to ciprofloxacin alone; concurrently resistant to one (28.7%), two (42.7%), three (10.7%), four (9.3%), or five (2.0%) other oral antimicrobial agents, most commonly ampicillin and TMP/SMX. Conclusions: Ciprofloxacin-resistant E. coli isolates from urine were frequently multidrug resistant in Korea. Close attention is required to monitor fluoroquinolone resistance patterns and the association of multidrug resistance with fluoroquinolone resistance in uropathogens."
- 362 View
- 0 Download

Review Articles
- Innovative Diagnostics for Sexually Transmitted Infections
- Seung-Ju Lee
- Korean J Urogenit Tract Infect Inflamm 2008;3(1):43-54. Published online April 30, 2008
-
 Abstract
Abstract
 PDF
PDF - Diagnostics for sexually transmitted infections (STIs) with easy non-invasive sample collection are important to increase testing and hence to reduce the spread of this infection. From this point of view, molecular technologies and rapid point-of-care tests are innovations which have gradually shifted the paradigm in the diagnosis of STIs from biological to molecular amplification and from laboratory to near-patient testing. These powerful diagnostic tools have improved and will continue to have a significant impact on our ability to design strategies and programs for the control and prevention of STIs.
- 397 View
- 4 Download

- The Relationship between Sexually Transmitted Diseases and HIV Transmission
- Sung Dae Kim, Dong Wan Sohn, Seung-Ju Lee, Sae Woong Kim, Yong-Hyun Cho
- Korean J Urogenit Tract Infect Inflamm 2007;2(2):157-166. Published online October 31, 2007
-
 Abstract
Abstract
 PDF
PDF - More than 42 million people worldwide are now infected with HIV, in spite of sustained prevention activities. Although the spread of HIV has been primarily sexual, epidemiological studies have indicated that the efficiency of the spread of HIV is poor, perhaps as infrequently as 1 in every 1,000 episodes of sexual intercourse. However, sexually transmitted diseases (STDs) that cause ulcers or inflammation greatly increase the efficiency of HIV transmission by increasing both the infectiousness of, and the susceptibility to HIV infection. STDs might be particularly important in the early stages of a localized HIV epidemic, when people with risky sexual behaviour are most likely to become infected. In China, eastern Europe and Russia, there has been a remarkable increase in the incidence of STDs in recent years, and this is reflected in the rapid increase in the spread of HIV in these areas. Targeted STDs detection and treatment should have a central role in HIV prevention in these emerging epidemics.
- 584 View
- 2 Download

- Practical Clinical Approach to Diagnosis and Update on Treatment of Syphilis
- Seung-Ju Lee
- Korean J Urogenit Tract Infect Inflamm 2006;1(1):31-38. Published online October 31, 2006
-
 Abstract
Abstract
 PDF
PDF - Syphilis is a systemic disease caused by Treponema pallidum. Syphilis is characterized by episodes of active disease(primary, secondary, tertiary stages) interrupted by periods of latency. The diagnosis of syphilis may involve dark?field microscopy of skin lesions but most often requires screening with a nontreponemal test and confirmation with a treponemal?specific test. Parenterally administered penicillin G is considered first?line therapy for all stages of syphilis. Alternative regimens for nonpregnant patients with no evidence of central nervous system involvement include doxycycline, tetracycline, ceftriaxone, and azithromycin. In pregnant women and congenital syphilis, penicillin remains the only effective treatment option; if these patients are allergic to penicillin, desensitization is required before treatment is initiated.. Once the diagnosis of syphilis is confirmed, quantitative nontreponemal test titers should be obtained. These titers should decline fourfold within six months after treatment of primary or secondary syphilis and within 12 to 24 months after treatment of latent or late syphilis. (Korean J UTII 2006;1:31-8)
- 352 View
- 0 Download


 KAUTII
KAUTII

 First
First Prev
Prev


