-
Mortality and Risk Factors for Emphysematous Pyelonephritis in Korea: A Multicenter Retrospective Cohort Study
-
Seung-Kwon Choi, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2025;20(1):34-41. Published online April 30, 2025
-
DOI: https://doi.org/10.14777/uti.2550006003
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose
Emphysematous pyelonephritis (EPN) is a life-threatening disease requiring immediate treatment. This multicenter retrospective cohort study aimed to analyze the mortality rate and risk factors associated with EPN.
Materials and Methods: Between January 2011 and February 2021, 217 patients diagnosed with EPN via computed tomography who visited 14 teaching hospitals were retrospectively analyzed. Clinical data, including age, sex, comorbidities, Huang and Tseng classification, hydronephrosis, acute kidney injury, blood and urine tests, surgical interventions, percutaneous drainage, and conservative treatments, were compared between the survival and death groups. Risk factors for mortality due to EPN were analyzed using univariate and multivariate methods.
Results
The mean age of survivors and deceased patients was 67.8 and 69.0 years, respectively (p=0.136). The sex distribution (male/female) was 48/146 and 8/15, respectively (p=0.298). Of the 217 patients, 23 died, resulting in a mortality rate of 10.6%. In univariate analysis, the Huang and Tseng classification (p=0.004), platelet count (p=0.005), and acute kidney injury (p=0.007) were significantly associated with mortality from EPN. In multivariate analysis, only the Huang and Tseng classification (p=0.029) was identified as a risk factor. Mortality rates according to the Huang and Tseng classification were as follows: class I (5.88%), class II (7.50%), class IIIa (14.28%), class IIIb (25.00%), and class IV (23.07%).
Conclusions
EPN is associated with a high mortality rate. Among various clinical factors, the Huang and Tseng classification was the most significant indicator for predicting mortality.
-
Citations
Citations to this article as recorded by  - Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
-
3,370
View
-
60
Download
-
1
Crossref
-
Hyperbaric Oxygen Therapy for the Treatment of Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Case Report
-
Kwang Jin Kim, Yoonsuk Lee, Yong Sung Cha, Tae Wook Kang, Hyun Chul Chung, Hong Chung, Hyun Kim, Jae Hung Jung
-
Urogenit Tract Infect 2024;19(2):44-47. Published online August 31, 2024
-
DOI: https://doi.org/10.14777/uti.2024.19.2.44
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Hyperbaric oxygen therapy (HBOT) was conducted on two male patients with chronic prostatitis/chronic pelvic pain syndrome who were resistant to conventional medical therapies. Both patients underwent 20 sessions of 100% oxygen inhalation (2.0 atmosphere absolute for 90 min/day, five days/week for four weeks) in a hyperbaric chamber. The follow-up period was three months. Although the patients reported a slight improvement in the pain domain of the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) after HBOT, no changes were noted in the other domains of NIH-CPSI and International Prostate Symptom Score. No adverse events were encountered during or after HBOT.
-
Ureteral Stent Induced Urinary Tract Infection and Microbial Inconsistency Between Bladder and Renal Pelvis
-
Useok Choi, Eun Jae Kim, Don Hee Lyu, Bong Hee Park, Hong Chung, Chang Hee Han, Sangrak Bae
-
Urogenit Tract Infect 2021;16(3):61-66. Published online December 31, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.3.61
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study examined the effects of long-term ureteral stent (US) on urinary tract infection (UTI) by bacterial migration and bacterial colonization.
Materials and Methods: From March 2014 to August 2021, 64 patients who underwent US for more than six months were enrolled in this study. When the US was inserted for the first time and replaced regularly, urine was collected from the bladder and renal pelvis and cultured. Patients’ the characteristics, and differences in pathogens related to US infection were analyzed.
Results: The mean age was 66.4 years, and the mean duration of indwelling was 37.5 months. There were 38 cases (59.3%) by malignant and 26 cases (40.6%) by benign causes. UTI occurred in 33 cases (53%); 16 cases (25%) were hospitalized for febrile UTI. After the initial US insertion, bacteria were identified in the bladder 285 days later and in the renal pelvis after 619 days. The bladder culture was positive in 10 of the 33 patients, and renal pelvis alone was positive in nine of the 33 patients. The same strain was confirmed in the bladder and renal pelvis in 12 cases (18.8%), and it took a mean of 5.8 months ± 6.32 (standard deviation) for the upward migration of bacteria.
Conclusions: UTIs occur in approximately 50% of patients with long-term US indwelling. The probability of culturing the same strain by a US was approximately 18.8%, and the role of pathogen transmission of a US does not appear to be significant. In addition, renal pelvis culture would be helpful in cases of failed bladder antibiotics susceptibility.
-
Citations
Citations to this article as recorded by  - Chemical Analysis and Antimicrobial Potential Assessment of Wild Laurel from the National Park Skadar Lake, Montenegro
Dragica Bojović, Miomir Šoškić, Ana Žugić, Marina T. Milenković, Iva Ljumović, Vanja M. Tadić
Applied Sciences.2025; 15(12): 6741. CrossRef - Comprehensive analysis of the bacterial spectrum for enhanced clinical insight in microbial ureteral stent colonization, uncomplicated urinary tract infections and catheter-associated urinary tract infections: a principal component analysis-based literatu
Matilde Lepori, Olivier Braissant, Gernot Bonkat, Malte Rieken
World Journal of Urology.2024;[Epub] CrossRef
-
8,205
View
-
28
Download
-
2
Crossref
-
Characteristics and Treatment Trends for Emphysematous Pyelonephritis in Korea: A 10-Year Multicenter Retrospective Study
-
Seung-Kwon Choi, Koo Han Yoo, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2021;16(2):49-54. Published online August 31, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.2.49
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study examined the characteristics, current treatment trends, and outcomes of patients with emphysematous pyelonephritis (EPN) in Korea.
Materials andMethods: Two hundred and seventeen patients diagnosed with EPN were evaluated using abdominal computed tomography in 2011-2021 at 15 institutes in Korea. The patients’ demographic and clinical characteristics, treatment modalities, and treatment outcomes were analyzed. The total study period was divided arbitrarily into groups A (2011-2014), B (2015-2017), and C (2018-2021) to analyze the trends in the EPN treatment.
Results: The mean age of the patients was 65.1 years; there were more female patients (74.2%) than male patients. The overall mortality rate was 10.6%. Ninety-five (43.8%), 98 (45.2%), and 24 (11.0%) patients were treated with medical, minimally invasive, and surgical management, respectively; the corresponding mortality rates were 13.7%, 6.1%, and 16.7%. There was no significant change in the proportion of patients treated with medical management over time (group A=46.5%, group B=47.0%, and group C=38.8%). The proportion of patients treated with minimally invasive management gradually increased over time (group A=35.2%; group B=43.9%; group C=55.0%), while those who underwent surgical management decreased gradually over time (group A=18.3%, group B=9.1%, and group C=6.3%). No differences in mortality rates were observed between the groups.
Conclusions: EPN with medical and minimally invasive management had a relatively high treatment success rate, which increased gradually, while surgical management decreased gradually over time in Korea. The mortality rate was relatively lower than that reported in studies published before the 2010s.
-
The Clinical Guidelines for Acute Uncomplicated Cystitis and Acute Uncomplicated Pyelonephritis
-
Ki Ho Kim, Jae Heon Kim, Seung-Ju Lee, Hong Chung, Jae Min Chung, Jae Hung Jung, Hyun Sop Choe, Hun Choi, Sun-Ju Lee, The Committee of The Korean Association of Urogenital Track Infection and Inflammation
-
Urogenit Tract Infect 2017;12(2):55-64. Published online August 31, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- To date, there has not been an establishment of guidelines for urinary tract infections, due to limited domestic data in Korea, unlike other North American and European countries. The clinical characteristics, etiology, and antimicrobial susceptibility of urinary tract infections vary from country to country. Moreover, despite the same disease, antibiotic necessary to treat it may vary from country to country. Therefore, it is necessary to establish a guideline that is relevant to a specific country. However, in Korea, domestic data have been limited, and thus, guidelines considering the epidemiological characteristics pertaining specifically to Korea do not exist. Herein, describe a guideline that was developed by the committee of The Korean Association of Urogenital Tract Infection and Inflammation, which covers only the uncomplicated urinary tract infections, as covering all parts in the first production is difficult.
-
The Antibiotic Susceptibility of Escherichia coli from Community-Acquired Uncomplicated Urinary Tract Infection: A Focused on Fosfomycin
-
Hyun-Sop Choe, Seung-Ju Lee, In Ho Chang, Tae-Hyoung Kim, Hong Chung, Jae Min Chung, Sang Don Lee, Jae Hung Jung, Ki Ho Kim, Seung Ki Min, Yong Gil Na, Hana Yoon, Ho Song Yu, Mi-Kyung Lee, Sun-Ju Lee
-
Urogenit Tract Infect 2017;12(2):77-81. Published online August 31, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: To assess the antibiotic susceptibility of Escherichia coli from community-acquired uncomplicated urinary tract infection (UTI).
Materials and Methods: Between August and December of 2015, confirmed cases of E. coli as a pathogen of community-acquired uncomplicated UTI were collected and assessed for antibiotic susceptibility in 10 designated hospitals. Additional fosfomycin susceptibility test was performed by a central laboratory using the disk diffusion method.
Results: A total of 347 E. coli isolates were collected from urine samples of community-acquired uncomplicated UTIs patients. The susceptibility rates of antibiotics were as follows: amikacin 100.0% (347), imipenem 100.0% (347), ciprofloxacin 57.1% (198), cefotaxime 74.9% (260), ampicillin 30.0% (104), trimethoprim/sulfamethoxazole 66.9% (232), and fosfomycin 98.0% (340). All fosfomycin-resistant E. coli isolates were extended-spectrum β-lactamase (ESBL)-producing. In 85 cases of ESBL-producing E. coli, the fosfomycin susceptibility rate was 91.8% (78/85).
Conclusions: Fosfomycin may be a useful option for the treatment of community-acquired uncomplicated UTIs. Further studies evaluating the role of fosfomycin in the treatment of UTIs and its clinical efficacy are necessary.
-
2017 Guidelines of The Korean Association of Urogenital Tract Infection and Inflammation: Acute Uncomplicated Cystitis
-
Ki Ho Kim, Seung-Ju Lee, Yong-Hyun Cho, Hyun-Sop Choe, Yong Gil Na, Jae Heon Kim, Hong Chung, Jae Min Chung, Jae Hung Jung, Hoon Choi, Sun-Ju Lee
-
Urogenit Tract Infect 2017;12(1):3-6. Published online April 30, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Acute uncomplicated cystitis is the most common urinary tract infection that mainly occurs in adult females, particularly sexually active young women and postmenopausal women. It is commonly observed in primary health care settings, including urology as well as obstetrics and gynecology; more than half of healthy adult women visit clinics and hospitals at least once in their lifetime due to acute uncomplicated cystitis. The most common bacterium causing this condition is Escherichia coli, followed by Staphylococcus saprophyticus, Klebsiella pneumoniae, Proteus mirabilis, and etc. Trimethoprim-sulfamethoxazole or fluoroquinolones have been used as an empirical antibiotic treatment. However, as fluoroquinolone-resistant organisms or extended spectrum beta-lactamase-producing organisms are becoming more prevalent worldwide, information on regional antibiotic resistance and guidelines on antibiotic use are becoming increasingly more desparate.
-
2017 Guidelines of The Korean Association of Urogenital Tract Infection and Inflammation: Recurrent Urinary Tract Infection
-
Seung-Ju Lee, Hyun-Sop Choe, Yong Gil Na, Ki Ho Kim, Jae Heon Kim, Hong Chung, Jae Min Chung, Jae Hung Jung, Hoon Choi, Sun-Ju Lee, Yong-Hyun Cho
-
Urogenit Tract Infect 2017;12(1):7-14. Published online April 30, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Recurrent infection after an acute urinary tract infection (UTI) episode is common in adult women. It is onerous to both the patient and the physician to treat frequent recurrent UTI. Every time when UTI recurs, patients experience lower urinary tract symptoms, fatigue, and limitation in everyday life, while the physician has difficulty in counseling patients with a disease entity whose pathophysiology is less known. Currently, prophylactic treatment for recurrent UTI is limited, is ineffective in most cases, and sometimes accompanies unexpected side effects. In this guideline, we aimed to establish feasible and effective recommendations for the treatment of recurrent UTI in healthy adult women.
-
The Effects of Microwave Thermotherapy for Chronic Prostatitis/Chronic Pelvic Pain Syndrome: A Prospective, Randomized Study
-
Hong Chung, Hoon Choi, Tag Keun Yoo, Jeong Man Cho, Hong Sup Kim
-
Urogenit Tract Infect 2017;12(1):35-41. Published online April 30, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) causes pain and urinary symptoms that involve the prostate and/or other parts of the male. We analyzed the clinical outcomes of medication and microwave thermotherapy.
Materials and Methods: A total of 132 patients with CP/CPPS for at least 3 months were assigned to one of the three study groups (group A: medication; group B: thermotherapy; group C: combination therapy). The NIH-CPSI was recorded at baseline, and at weeks 2, 4, 8, and 12 post-therapy. EPS was evaluated, and semen analysis was performed to assess the changes in prostatic inflammation. Moreover, patient satisfaction questionnaire was completed.
Results: Comparisons between groups A and B, as well as between groups B and C showed no significant changes in pain, quality of life, and total scores. At week 12, group C, when compared with group A, had a significantly improved voiding score (4.19±3.02 vs. 2.71±2.30, p=0.019) and EPS (12.47±15.91 vs. 3.73±4.82, p=0.003). At week 4, the patient satisfaction score in group C was significantly different from that in other groups (p=0.043), but there was no difference at week 12 (p>0.05). There was no statistically significant difference in laboratory test results, PSA, and prostate volume between the three groups at baseline and week 12. Complications of thermotherapy resolved with conservative management.
Conclusions: Our results showed that a combination of medication and thermotherapy improved NIH-CPSI and patient satisfaction in CP/CPPS more than medication alone. We suggested that thermotherapy could be another treatment option for CP/CPPS.
-
The Association between Chronic Inflammation and Recurrent Cystitis in Women
-
Hong Chung
-
Urogenit Tract Infect 2016;11(3):86-92. Published online December 31, 2016
-
-
-
 Abstract Abstract
 PDF PDF
- Recurrent urinary tract infection is a common infectious disease seen in the clinic. It is very prevalent in women; as many as 15% of women develop urinary tract infection each year, and at least 25% have one or more recurrences. Chronic inflammation and increased urothelial apoptosis reflect a common pathophysiology in various lower urinary tract dysfunctions, causing bladder storage symptoms. It has been suggested that chronic inflammation could be associated with overactive detrusor and increased levels of urinary nerve growth factor and creatinine. The level of urinary nerve growth factor may decrease after an effective antimuscarinic therapy. Recurrent urinary tract infection could be prevented by using nonsteroidal anti-inflammatory drugs or cyclooxygenase-2 inhibitors. Intravesical hyaluronate and chondroitin sulfate reduce the incidence of recurrent bacterial cystitis, and treatment with hyaluronate targets bacterial adherence to the bladder mucosa in interstitial cystitis/bladder pain syndrome. This article reviews the pathophysiology of chronic inflammation of the bladder and investigates the association between chronic inflammation and recurrent urinary tract infection.
-
Infectious Complications after Prostate Biopsy: A Prospective Multicenter Prostate Biopsy Study
-
Eu Chang Hwang, Ho Song Yu, Seung Il Jung, Dong Deuk Kwon, Sun Ju Lee, Tae-Hyoung Kim, In Ho Chang, Hana Yoon, Bongsuk Shim, Kwang Hyun Kim, Donghyun Lee, Jung-Sik Huh, Dong Hoon Lim, Won Jin Jo, Seung Ki Min, Gilho Lee, Ki Ho Kim, Tae Hwan Kim, Seo Yeon Lee, Seung Ok Yang, Jae Min Chung, Sang Don Lee, Chang Hee Han, Sang Rak Bae, Hyun Sop Choe, Seung-Ju Lee, Hong Chung, Yong Gil Na, Seung Woo Yang, Sung Woon Park, Young Ho Kim, Tae Hyo Kim, Won Yeol Cho, June Hyun Han, Yong-Hyun Cho, U-Syn Ha, Heung Jae Park, The Korean Association of Urogenital Tract Infection and Inflammation (KAUTII)
-
Urogenit Tract Infect 2016;11(1):17-24. Published online April 30, 2016
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: Recent studies have highlighted an increasing trend of infectious complications due to fluoroquinolone-resistant organisms among men undergoing transrectal prostate biopsy. This study evaluated the current incidence of infective complications after trans-rectal prostate biopsy for identification of risk factors in Korean men who received fluoroquinolone prophylaxis.
Materials and Methods: A prospective, multicenter study was conducted in Korea from January to December 2015. Prostate biopsies performed with fluoroquinolone prophylaxis during 3 months in each center were included. A pre-biopsy questionnaire was used for identification of patient characteristics. Clinical variables including underlying disease, antibiotic prophylaxis, enema, povidoneiodine cleansing of the rectum, and infectious complications were evaluated. The primary outcome was the post-biopsy infection rate after fluoroquinolone prophylaxis. Univariable and multivariable analyses were used for identification of risk factors for infectious complications.
Results: The study included 827 patients, of whom 93 patients (11.2%) reported receiving antibiotics in the previous 6 months and 2.5% had a history of prostatitis. The infectious complication rate was 2.2%. Post-biopsy sepsis was reported in 2 patients (0.2%). In multivariable analysis predictors of post-biopsy sepsis included person performing biopsy (adjusted odds ratio [OR], 4.05; 95% confidence interval [CI], 1.31-12.5; p=0.015) and operation history within 6 months (adjusted OR, 5.65; 95% CI, 1.74-18.2; p=0.004).
Conclusions: The post-prostate biopsy infectious complication rate in this study was 2.2%. Person performing biopsy (non-urologists) and recent operation history were independent risk factors for infectious complications after trans-rectal prostate biopsy.
-
Challenge of Developing a Herpes Simplex Virus Vaccine
-
Hong Chung
-
Korean J Urogenit Tract Infect Inflamm 2014;9(2):74-78. Published online October 31, 2014
-
-
-
 Abstract Abstract
 PDF PDF
- Herpes simplex virus 1 and 2 (HSV-1 and HSV-2), also known as human herpes virus 1 and 2 (HHV-1 and HHV-2), are two members of the herpes virus family, herpes viridae, which infect humans. Both HSV-1 (which produces most cold sores) and HSV-2 (which produces most genital herpes) are ubiquitous and contagious. They can be spread when an infected person is producing and shedding the virus. Herpes Simplex can be spread through contact with saliva, such as sharing drinks. HSV-2 is one of the most prevalent sexually transmitted infections worldwide. In addition to recurrent genital ulcers, HSV-2 causes neonatal herpes, and is associated with a 3-fold increased risk for HIV acquisition. Many HSV-2 vaccines have been studied in animal models, however, few have reached clinical trials, and those that have been tested in humans were not consistently effective. Here, I review HSV-2 pathogenesis, with a focus on novel understanding of mucosal immunobiology of HSV-2, and vaccine efforts to date, in an attempt to stimulate thinking about future directions for development of effective prophylactic and therapeutic HSV-2 vaccines.
-
Chronic Prostatitis/Chronic Pelvic Pain Syndrome: What Are the Starting and Worsening Factors?
-
Hong Chung
-
Korean J Urogenit Tract Infect Inflamm 2013;8(1):7-12. Published online April 30, 2013
-
-
-
 Abstract Abstract
 PDF PDF
- Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) in the absence of any identifiable pathology such as cancer, curable infection, or anatomic abnormalities is defined as “urologic pain or discomfort in the pelvic region, associated with urinary symptoms and/or sexual dysfunction, lasting for at least 3 of the previous 6 months”. However, etiologic factors of CP/CPPS remain unknown. The traditional marker of inflammation, namely white blood cells in prostatic fluids, dose not correlate with the predominant symptom of pelvic pain. The role of normal bacterial flora in prostate in inciting the inflammatory response has also been reconsidered. Nanobacterial infection might be an important etiologic factor of type III prostatitis. An imbalance toward increased proinflammatory and decreased anti-inflammatory cytokines has been implicated, and its correlation with pelvic pain has also been observed to some extent. Pelvic pain also correlates with the neurotrophin (nerve growth factor) implicated in neurogenic inflammation and central sensitization. Finally, psychological stress may produce measurable biochemical changes and affect other processes. Here, the author reviewed the existing literature on etiology involved in the mechanisms of CP/CPPS.
-
Can Betadine Gauze Compression Be Decreased Significant Complications after Prostate Needle Biopsy under Transrectal Ultrasound at Outpatient Department?: Single Clinician’s Experience
-
Hong Chung, Hong Sup Kim, Sang-Kuk Yang
-
Korean J Urogenit Tract Infect Inflamm 2012;7(1):43-49. Published online April 30, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: Recently, the number of patients undergoing prostate biopsy has increased due to the development of cancer screening test with prostate specific antigen. Prostate needle biopsy under transrectal ultrasound (Bx-TRUS) is the standard procedure to diagnose prostate cancer. We evaluated the incidence of significant infectious and bleeding complications performed by a single urologist with unique methods of betadine gauze compression after Bx-TRUS. Materials and Methods: We retrospectively evaluated the medical records of 299 patients, who underwent Bx-TRUS, from March 2007 to December 2011. All patients received oral levofloxacin 500mg for 4 days. Significant complications, related to infection with fever and persistent rectal bleeding, were evaluated within 4 weeks after biopsy. Patients who presented infectious complications were treated with intravenous ceftriaxone 2.0gm for 5 or 7 days. Patients who present significant anal bleeding were managed with primary closure by colorectal clinic in the department of surgery. Results: Among 299 patients, 4patients (1.3%) developed post-biopsy infections and hemorrhage. Those major complications were catergorized as acute prostatitis (2 patients, 0.7%) and rectal bleeding (2 patients, 0.7%). Of the 2 cases with post-biopsy infection, 1 case (Escherichia coli) had positive urine and blood culture. E. coli was sensitive to cephalosporine, but was resistant to fluoroquinolone. Conclusions: The results of this study suggest that betadine compression after Bx-TRUS may play the role of decreasing or preventing the significant complications, such as febrile infections and persistent rectal bleeding. Further, well designed study is needed to evaluate the clinical implication of betadine gauze compression after Bx-TRUS."
-
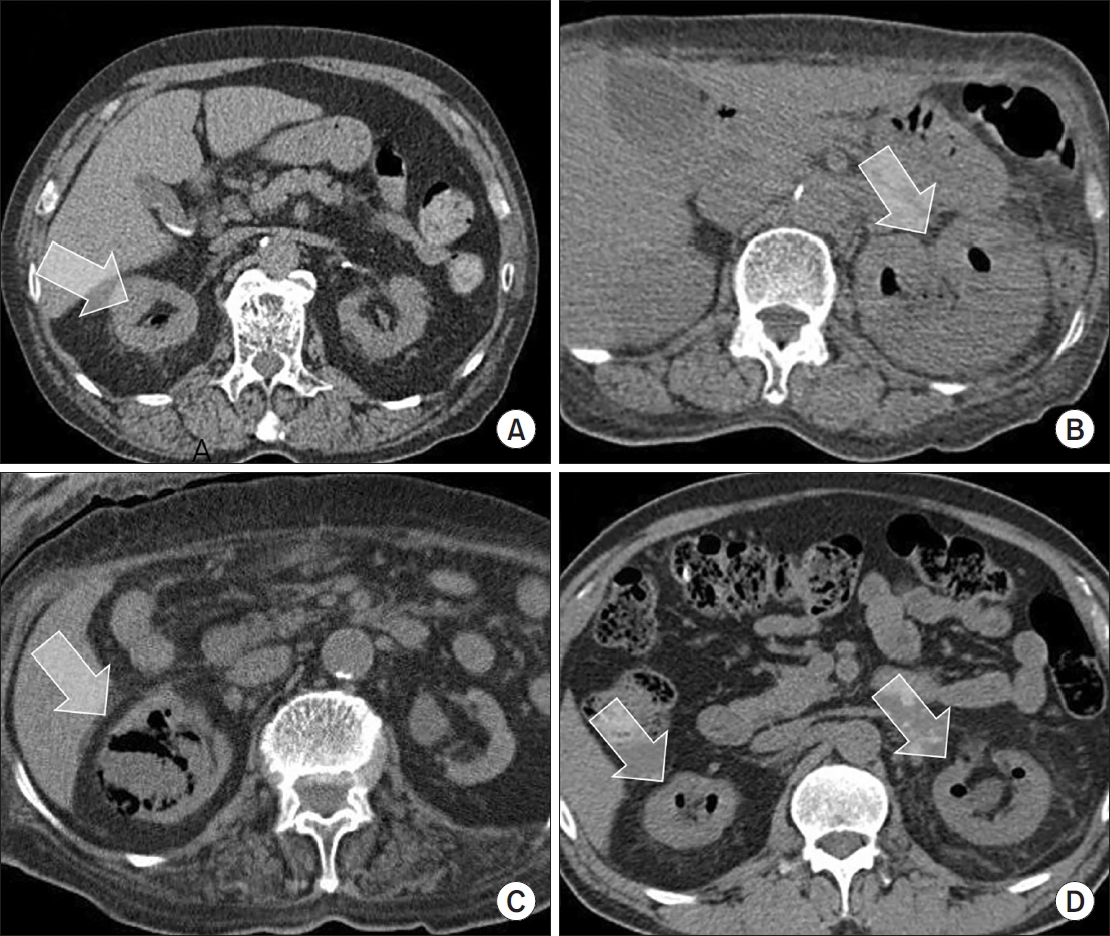
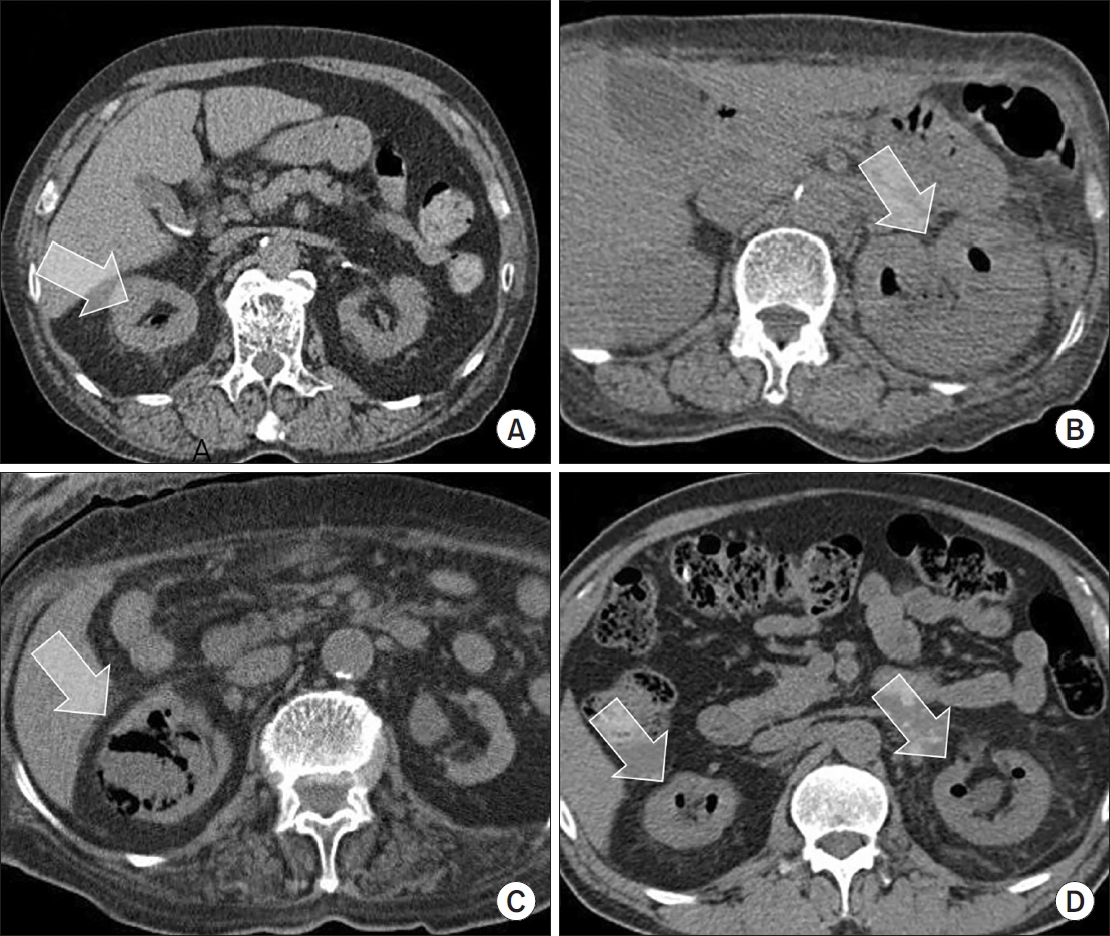
Percutaneous Management of Renal Abscess in Polycystic Kidney Disease
-
Hong Chung, Yong Ik Lee, Hong Sup Kim, Sang-Kuk Yang
-
Korean J Urogenit Tract Infect Inflamm 2011;6(2):209-212. Published online October 31, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- Autosomaldominant polycystic kidney disease (ADPKD) is one of the commonest hereditary disorders and the most common life-threatening genetic disease, affecting an estimated 12.5 million people worldwide. PKD are congenital and bilateral diseases, and those symptoms almost never appear until after age 40. Urinary tract infection occurs with increased frequency in ADPKD and infection in ADPKD is a particularly serious complication. Here, we report a 79-year-old man with an intermittent high fever during 2 months and bulging mass at the right flank.
|