Search
- Page Path
- HOME > Search
Review Article
- Regenerative Medicine for the Kidney
- Vladimir Mashanov, Ji Hyun Kim
- Urogenit Tract Infect 2025;20(3):144-158. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550028014
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
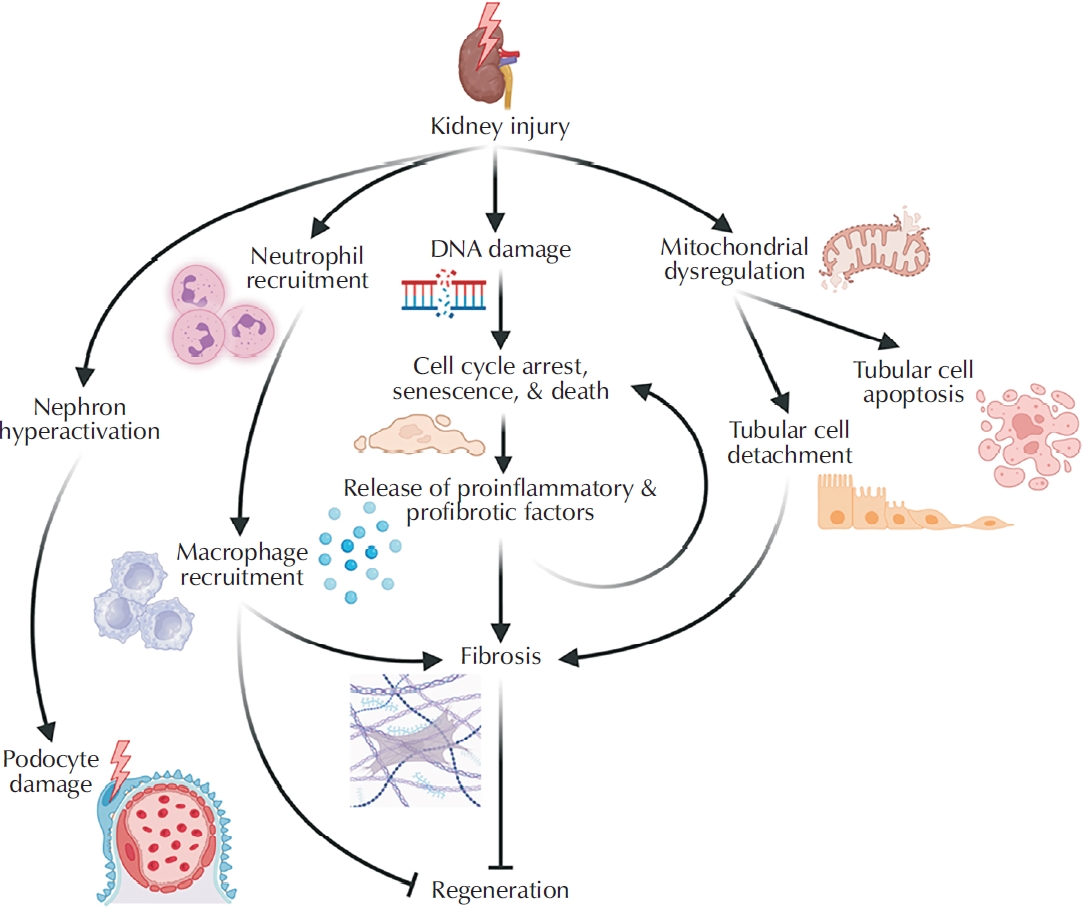
ePub - Kidney disease poses a major and growing global health challenge, with both prevalence and mortality continuing to rise. Current standard-of-care treatments, including dialysis and kidney transplantation, have significant limitations and do not adequately meet clinical needs. This unmet need has driven the development of next-generation regenerative medicine strategies, which can be broadly categorized into 3 areas: (1) approaches that enhance the kidney’s limited intrinsic regenerative capacity; (2) stem cell-based therapies; and (3) implantable bioengineered kidney constructs. This review summarizes recent advances in each of these domains and discusses the major biological, technical, and regulatory challenges that must be addressed to enable successful clinical translation.
- 597 View
- 8 Download

Case Reports
- Klebsiella pneumoniae-Induced Emphysematous Prostatic Abscess Accompanied by a Spinal Cord Infarction: Case Report
- Seong Uk Jeh, Min Sung Choi, Chang Seok Kang, Dae Hyun Kim, Jae Hwi Choi, See Min Choi, Sung Chul Kam, Jeong Seok Hwa, Jae Seog Hyun
- Urogenit Tract Infect 2024;19(3):104-108. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448024012
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
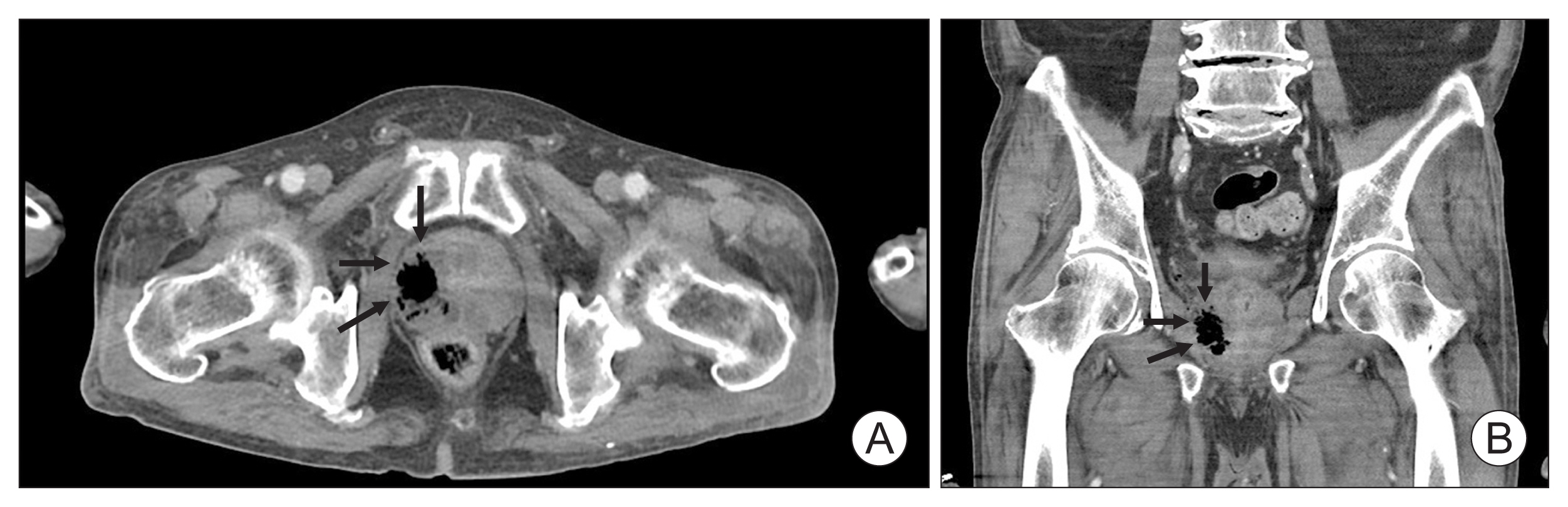
ePub - Various strains can be found in emphysematous prostatic abscesses (EPAs), but the most frequent causative organism is Klebsiella pneumoniae . Hypervirulent K. pneumoniae can disseminate to distant sites by forming a muco-polysaccharide network outside the capsule. Here, we present the first case of K. pneumoniae in an EPA accompanied by a spinal cord infarction. A 65-year-old man was referred to our hospital due to sudden-onset paraplegia after a 5-day history of fever, myalgia, and voiding difficulty. Abdominal computed tomography revealed a collection of air pockets in the prostate, and diffusion-weighted magnetic resonance imaging showed high signal intensity in the thoracic spinal cord. The patient was initially treated with antibiotics and surgical drainage. On the third hospital day, therapeutic heparin was added after discussion with a neurologist. The patient had no inflammatory symptoms, experienced some improvement in paraplegia, and was discharged on the 14th hospital day. This study adhered to the case report guidelines.
- 2,231 View
- 23 Download

- Hyperbaric Oxygen Therapy for the Treatment of Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Case Report
- Kwang Jin Kim, Yoonsuk Lee, Yong Sung Cha, Tae Wook Kang, Hyun Chul Chung, Hong Chung, Hyun Kim, Jae Hung Jung
- Urogenit Tract Infect 2024;19(2):44-47. Published online August 31, 2024
- DOI: https://doi.org/10.14777/uti.2024.19.2.44
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Hyperbaric oxygen therapy (HBOT) was conducted on two male patients with chronic prostatitis/chronic pelvic pain syndrome who were resistant to conventional medical therapies. Both patients underwent 20 sessions of 100% oxygen inhalation (2.0 atmosphere absolute for 90 min/day, five days/week for four weeks) in a hyperbaric chamber. The follow-up period was three months. Although the patients reported a slight improvement in the pain domain of the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) after HBOT, no changes were noted in the other domains of NIH-CPSI and International Prostate Symptom Score. No adverse events were encountered during or after HBOT.
- 5,283 View
- 35 Download

Original Articles
- Serum CCL11 Levels in Benign Prostatic Hyperplasia and Prostate Cancer
- Kyu-Shik Kim, Hong-Sang Moon, Sung-Yul Park, Hwan-Sik Hwang, Jung-Hyun Kim, Sang-Su Kim, Ik-Hwan Han, Ki-Jun Kim, Chang-Suk Noh, Jae-Sook Ryu
- Urogenit Tract Infect 2016;11(3):103-108. Published online December 31, 2016
-
 Abstract
Abstract
 PDF
PDF - Purpose: CC-chemokine ligand 11 (CCL11; eotaxin-1), an eosinophil chemoattractant chemokine, has been proposed as a serum marker for prostate cancer (PCa) by two research groups. We investigated the usefulness of CCL11 in diagnosing prostatic diseases, such as benign prostatic hyperplasia (BPH) and PCa.
Materials and Methods: CCL11 was measured in the sera of 139 men with BPH, 44 men with PCa, and 45 control men attending an outpatient health-screening clinic. A commercial enzyme-linked immunosorbent assay kit was used to measure CCL11.
Results: CCL11 concentrations were significantly higher in men with BPH and PCa than in normal men (72.9±3.15 and 80.0±4.91 pg/ml vs. 57.6±8.24). In addition, a receiver operating characteristic (ROC) analysis of serum CCL11 levels showed that the areas under the ROC curves were 0.661 (p=0.001) and 0.654 (p=0.012) for BPH and PCa, respectively, compared with normal men.
Conclusions: CCL11 may be helpful in diagnosing prostatic diseases, such as BPH and PCa.
- 432 View
- 0 Download

- Infectious Complications after Prostate Biopsy: A Prospective Multicenter Prostate Biopsy Study
- Eu Chang Hwang, Ho Song Yu, Seung Il Jung, Dong Deuk Kwon, Sun Ju Lee, Tae-Hyoung Kim, In Ho Chang, Hana Yoon, Bongsuk Shim, Kwang Hyun Kim, Donghyun Lee, Jung-Sik Huh, Dong Hoon Lim, Won Jin Jo, Seung Ki Min, Gilho Lee, Ki Ho Kim, Tae Hwan Kim, Seo Yeon Lee, Seung Ok Yang, Jae Min Chung, Sang Don Lee, Chang Hee Han, Sang Rak Bae, Hyun Sop Choe, Seung-Ju Lee, Hong Chung, Yong Gil Na, Seung Woo Yang, Sung Woon Park, Young Ho Kim, Tae Hyo Kim, Won Yeol Cho, June Hyun Han, Yong-Hyun Cho, U-Syn Ha, Heung Jae Park, The Korean Association of Urogenital Tract Infection and Inflammation (KAUTII)
- Urogenit Tract Infect 2016;11(1):17-24. Published online April 30, 2016
-
 Abstract
Abstract
 PDF
PDF - Purpose: Recent studies have highlighted an increasing trend of infectious complications due to fluoroquinolone-resistant organisms among men undergoing transrectal prostate biopsy. This study evaluated the current incidence of infective complications after trans-rectal prostate biopsy for identification of risk factors in Korean men who received fluoroquinolone prophylaxis.
Materials and Methods: A prospective, multicenter study was conducted in Korea from January to December 2015. Prostate biopsies performed with fluoroquinolone prophylaxis during 3 months in each center were included. A pre-biopsy questionnaire was used for identification of patient characteristics. Clinical variables including underlying disease, antibiotic prophylaxis, enema, povidoneiodine cleansing of the rectum, and infectious complications were evaluated. The primary outcome was the post-biopsy infection rate after fluoroquinolone prophylaxis. Univariable and multivariable analyses were used for identification of risk factors for infectious complications.
Results: The study included 827 patients, of whom 93 patients (11.2%) reported receiving antibiotics in the previous 6 months and 2.5% had a history of prostatitis. The infectious complication rate was 2.2%. Post-biopsy sepsis was reported in 2 patients (0.2%). In multivariable analysis predictors of post-biopsy sepsis included person performing biopsy (adjusted odds ratio [OR], 4.05; 95% confidence interval [CI], 1.31-12.5; p=0.015) and operation history within 6 months (adjusted OR, 5.65; 95% CI, 1.74-18.2; p=0.004).
Conclusions: The post-prostate biopsy infectious complication rate in this study was 2.2%. Person performing biopsy (non-urologists) and recent operation history were independent risk factors for infectious complications after trans-rectal prostate biopsy.
- 821 View
- 3 Download

- The Expression of CC Cytokine, Macrophage Inflammatory Protein in a Acute Cystitis and Bladder Pain Syndrome
- Jun Mo Kim, Chae Hyun Kim, Yong-Wha Lee, Kwang Woo Lee, Young Ho Kim, Min Eui Kim
- Korean J Urogenit Tract Infect Inflamm 2007;2(2):190-196. Published online October 31, 2007
-
 Abstract
Abstract
 PDF
PDF - "Purpose: Macrophage inflammatory protein-1alpha (MIP-1alpha) and MIP-1beta are members of the CC chemokine subfamily. To evaluate the changes of the expression of macrophage inflammatory protein-1 (MIP-1α and MIP-1β) by ELISA test in the patients with acute cystitis and bladder pain syndrome. Materials and Methods: From January 2007 to May 2007, urine samples were obtained from 13 female control group, 16 female patients (mean age 44.8 years) with acute cystitis and 26 female patients (mean age 48.2 years) with bladder pain syndrome. The urine level of MIP-1α and MIP-1β were compared by enzyme linked immunosorbent assay (ELISA) test. Results: The urine level of MIP-1α and MIP-1β was not significantly higher in both group than control group. But urine level of MIP-1α in patients with acute cystitis by E. coli was significantly higher than control group (p=0.006). Conclusions: Although urine level of MIP-1α and MIP-1β in patients with acute cystitis and bladder pain syndrome were not higher than control group, MIP-1α was increased in acute cystitis by E. coli. "
- 390 View
- 2 Download


 KAUTII
KAUTII
 First
First Prev
Prev


