-
Mortality and Risk Factors for Emphysematous Pyelonephritis in Korea: A Multicenter Retrospective Cohort Study
-
Seung-Kwon Choi, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2025;20(1):34-41. Published online April 30, 2025
-
DOI: https://doi.org/10.14777/uti.2550006003
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose
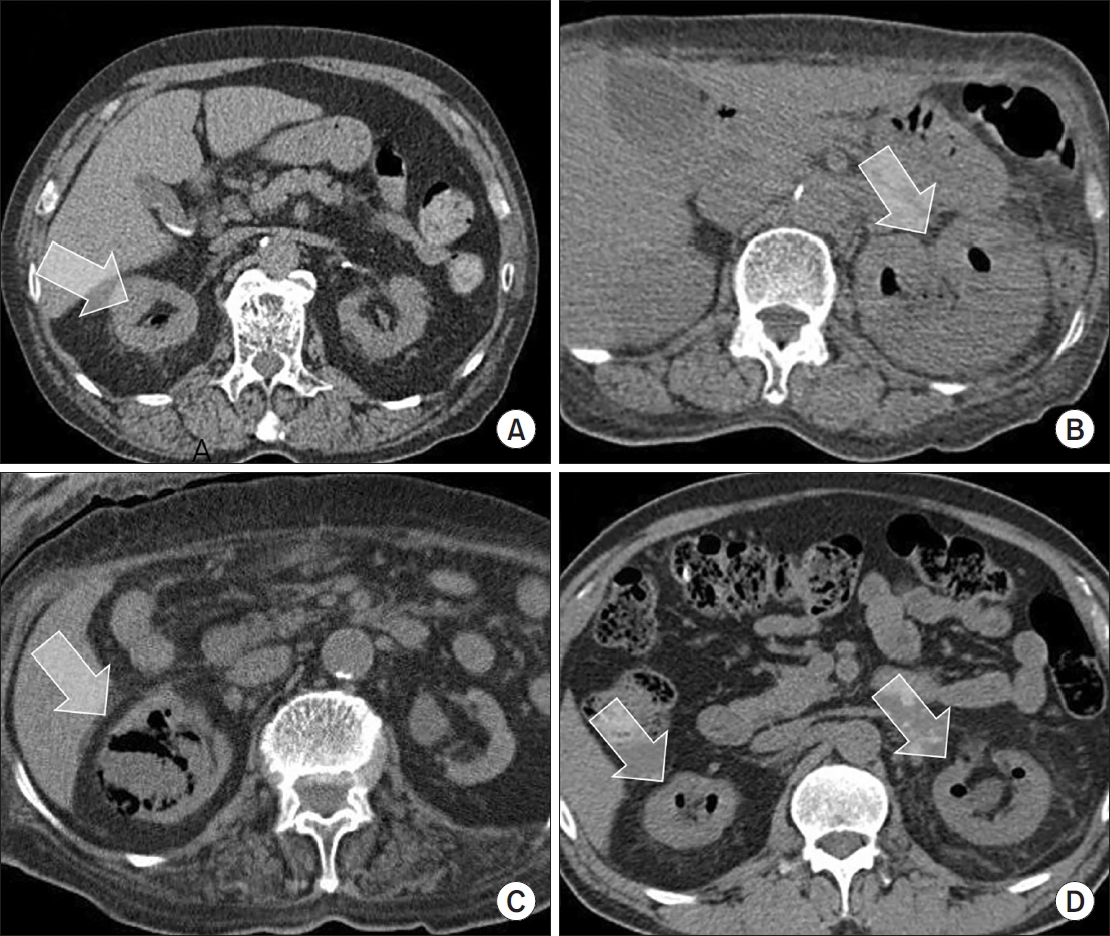
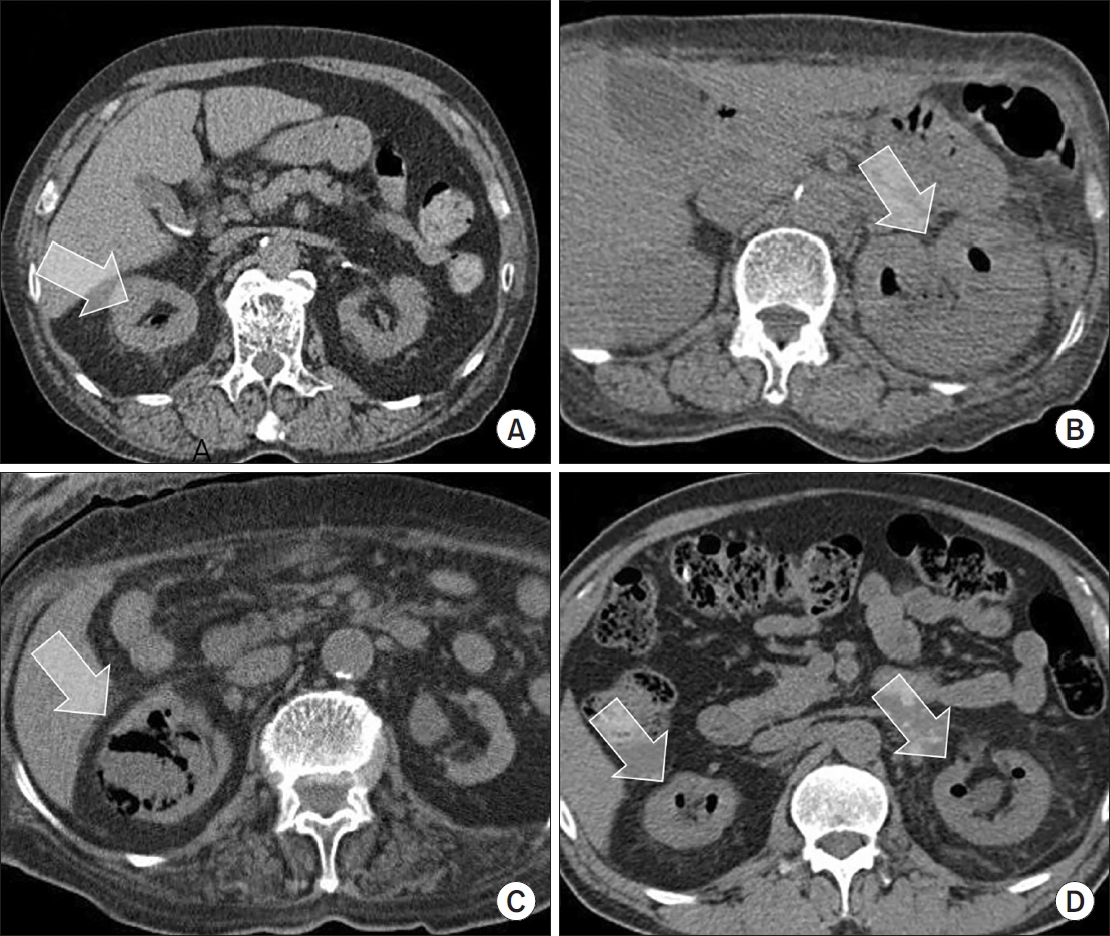
Emphysematous pyelonephritis (EPN) is a life-threatening disease requiring immediate treatment. This multicenter retrospective cohort study aimed to analyze the mortality rate and risk factors associated with EPN.
Materials and Methods: Between January 2011 and February 2021, 217 patients diagnosed with EPN via computed tomography who visited 14 teaching hospitals were retrospectively analyzed. Clinical data, including age, sex, comorbidities, Huang and Tseng classification, hydronephrosis, acute kidney injury, blood and urine tests, surgical interventions, percutaneous drainage, and conservative treatments, were compared between the survival and death groups. Risk factors for mortality due to EPN were analyzed using univariate and multivariate methods.
Results
The mean age of survivors and deceased patients was 67.8 and 69.0 years, respectively (p=0.136). The sex distribution (male/female) was 48/146 and 8/15, respectively (p=0.298). Of the 217 patients, 23 died, resulting in a mortality rate of 10.6%. In univariate analysis, the Huang and Tseng classification (p=0.004), platelet count (p=0.005), and acute kidney injury (p=0.007) were significantly associated with mortality from EPN. In multivariate analysis, only the Huang and Tseng classification (p=0.029) was identified as a risk factor. Mortality rates according to the Huang and Tseng classification were as follows: class I (5.88%), class II (7.50%), class IIIa (14.28%), class IIIb (25.00%), and class IV (23.07%).
Conclusions
EPN is associated with a high mortality rate. Among various clinical factors, the Huang and Tseng classification was the most significant indicator for predicting mortality.
-
Citations
Citations to this article as recorded by  - Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
-
3,370
View
-
60
Download
-
1
Crossref
-
Korean Multicenter Study of Infectious Complications after Transurethral Prostate Surgery in Patients with Preoperative Sterile Urine
-
Seong Hyeon Yu, Seung Il Jung, Eu Chang Hwang, Tae-Hyoung Kim, Jae Duck Choi, Koo Han Yoo, Jeong Woo Lee, Dong Hoon Koh, Sangrak Bae, Seung Ok Yang, Joongwon Choi, Seung Ki Min, Hoon Choi
-
Urogenit Tract Infect 2022;17(3):81-88. Published online December 31, 2022
-
DOI: https://doi.org/10.14777/uti.2022.17.3.81
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: To evaluate the efficacy of antibiotic prophylaxis and determine the risk factors of infectious complications after transurethral surgery of the prostate.
Materials and Methods: Seven hundred and seventy-two patients who underwent transurethral resection of the prostate (TURP) or holmium laser enucleation of the prostate (HOLEP) were reviewed. Of these, this study enrolled 643 patients without bacteriuria who had not received antibiotics for urinary tract infections for two weeks before surgery. The patients were divided into two groups according to the duration of the antibiotics (Group 1: less than one day, n=396 vs. Group 2: more than one day, n=247).
Results: The overall incidence of postoperative infectious complications in 643 patients was 5.0% (32/643). When postoperative infectious complications were compared according to the duration of the antibiotics (Group 1 vs. Group 2), the infectious complications rates were 5.6% (22/396) vs. 4.0% (10/247), respectively (p=0.393). When postoperative infectious complications were compared according to the duration of antibiotics (Group 1 vs. Group 2) in the TURP and HOLEP groups, the infectious complications rates were 6.3% (12/192) vs. 1.0% (1/103) (p=0.035) and 4.9% (10/203) vs. 6.0% (8/134) (p=0.677), respectively. The duration of Foley catheterization was independently associated with infectious complications (p=0.003).
Conclusions: The results showed that prolonged postoperative catheterization affects postoperative infectious complications associated with transurethral prostate surgery. Although antibiotics administered for less than one day are effective for antibiotic prophylaxis of transurethral prostate surgery, a longer antibiotic therapy is recommended for TURP.
-
Citations
Citations to this article as recorded by  - Evaluation of Postoperative Urinary Tract Infection and Sepsis Rates After Adding Cystolitholapaxy to HoLEP:
A Retrospective Analysis
Federico Rovegno, Rajiv Pillai, Zafar Maan, Soumendra Datta, Omar Nasir, Gerald Rix
International Journal of Clinical Urology.2026; 10(1): 1. CrossRef
-
3,722
View
-
24
Download
-
1
Crossref
-
Comprehensive Review of COVID-19 on Benign Prostate Hyperplasia Patient Symptoms
-
Joongwon Choi, Hong Jin Suh, Dong Hwan Lee, Tae-Kon Hwang, Jung Jun Kim
-
Urogenit Tract Infect 2022;17(2):31-35. Published online August 31, 2022
-
DOI: https://doi.org/10.14777/uti.2022.17.2.31
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader ePub ePub
- Since the outbreak of the global Coronavirus disease (COVID-19) pandemic in 2019, the number of confirmed cases has increased steadily worldwide. The most common symptom of COVID-19 (SARS-CoV-2) is respiratory symptoms. On the other hand, increased voiding frequency and lower urinary tract symptoms (LUTS) have also been reported. Regarding the relationship between LUTS and COVID-19, only small size (n<100) retrospective studies have been reported, but the post-International Prostate Symptom Score (IPSS) increases compared to pre-IPSS after a COVID-19 infection in those older than 50 years. α-blockers and phosphodiesterase-5 inhibitors are relatively safe, but there are conflicting reports on 5α-reductase inhibitors; hence, further research is needed. Four major theories have been argued regarding the relationship between LUTS and COVID-19: renin-angiotensin system-related, androgen-related, inflammation-related, and metabolic derangement-related. In conclusion, elderly male patients often have benign prostate hyperplasia as a co-morbidity, and the severity of COVID-19 is high in this group. Therefore, voiding symptoms in these patient groups is of particular concern.
-
Characteristics and Treatment Trends for Emphysematous Pyelonephritis in Korea: A 10-Year Multicenter Retrospective Study
-
Seung-Kwon Choi, Koo Han Yoo, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2021;16(2):49-54. Published online August 31, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.2.49
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study examined the characteristics, current treatment trends, and outcomes of patients with emphysematous pyelonephritis (EPN) in Korea.
Materials andMethods: Two hundred and seventeen patients diagnosed with EPN were evaluated using abdominal computed tomography in 2011-2021 at 15 institutes in Korea. The patients’ demographic and clinical characteristics, treatment modalities, and treatment outcomes were analyzed. The total study period was divided arbitrarily into groups A (2011-2014), B (2015-2017), and C (2018-2021) to analyze the trends in the EPN treatment.
Results: The mean age of the patients was 65.1 years; there were more female patients (74.2%) than male patients. The overall mortality rate was 10.6%. Ninety-five (43.8%), 98 (45.2%), and 24 (11.0%) patients were treated with medical, minimally invasive, and surgical management, respectively; the corresponding mortality rates were 13.7%, 6.1%, and 16.7%. There was no significant change in the proportion of patients treated with medical management over time (group A=46.5%, group B=47.0%, and group C=38.8%). The proportion of patients treated with minimally invasive management gradually increased over time (group A=35.2%; group B=43.9%; group C=55.0%), while those who underwent surgical management decreased gradually over time (group A=18.3%, group B=9.1%, and group C=6.3%). No differences in mortality rates were observed between the groups.
Conclusions: EPN with medical and minimally invasive management had a relatively high treatment success rate, which increased gradually, while surgical management decreased gradually over time in Korea. The mortality rate was relatively lower than that reported in studies published before the 2010s.
-
Systematic Literature Review of the Urological Field and Considerations in COVID-19
-
Joongwon Choi, Hyun Soo Ryoo, Jae Hyun Ryu, Yun Beom Kim, Seung Ok Yang, Jeong Kee Lee, Tae Young Jung, Jung Hoon Kim, Tae-Hyoung Kim
-
Urogenit Tract Infect 2021;16(1):1-7. Published online April 30, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.1.1
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Coronavirus disease 2019 (COVID-19) was declared a worldwide pandemic in March 2020 after originating in China. Widespread uncertainty resulting from the pandemic has revolutionized urology practice worldwide, similar to that observed in other fields. The urological manifestations of COVID-19 were investigated by performing a literature search using a combination of keywords related to COVID-19 and urology. To date, COVID-19 has not been associated with any lower urinary tract symptoms, and there is no level 1 evidence that associates it with urinary malignancy and urolithiasis. Viral RNA has been detected in urine (5.74%), but there is no evidence of actual infection via urine. COVID-19 has transformed the standard urological practice into crisis-based care and has changed the medical and surgical priorities dramatically in the field. Most hospitals have established quarantine guidelines for each hospital, and procedures must be performed according to the present circumstances. Furthermore, in the absence of high-level evidence, specific efforts are needed to minimize the risk of COVID-19 infections during care.
|