Search
- Page Path
- HOME > Search
Review Article
- Molecular Mechanisms of Antibiotic Resistance in Uropathogenic Escherichia coli: A Narrative Review
- Nakjun Choi, Dong Uk Kim, Eun-Jin Lee
- Urogenit Tract Infect 2025;20(2):96-106. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550018009
-
 Abstract
Abstract
 PDF
PDF PubReader
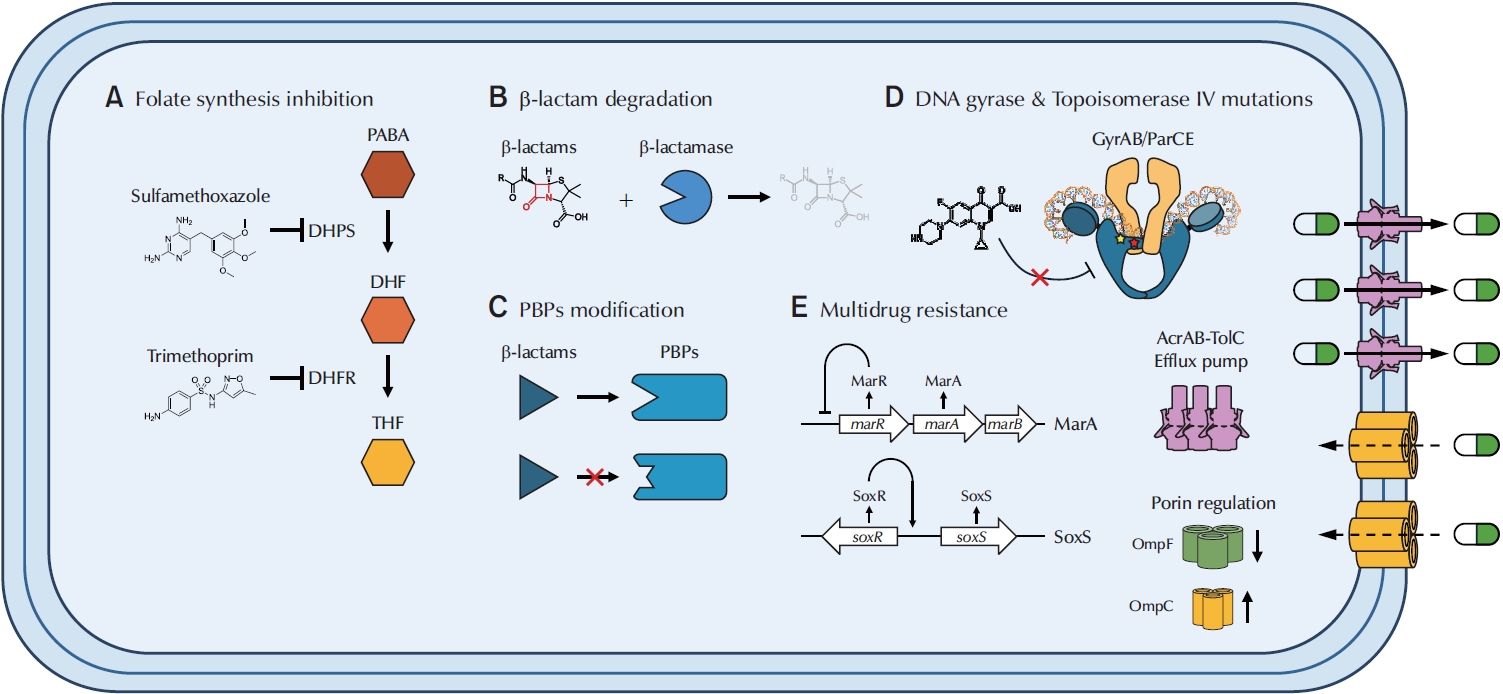
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections worldwide, with uropathogenic Escherichia coli (UPEC) serving as the primary causative agent. Although antibiotic therapy remains the standard of care for UTI treatment, the increasing prevalence of antimicrobial resistance has substantially reduced the effectiveness of commonly prescribed antibiotics. Resistance to trimethoprim-sulfamethoxazole (TMP-SMX), β-lactams, and fluoroquinolones is particularly concerning, as these agents constitute the principal therapeutic options for UTIs. This review examines the molecular mechanisms underlying UPEC resistance to these three classes of antibiotics, including target site modifications, efflux pump overexpression, porin regulation, and enzymatic degradation. Furthermore, it explores how these resistance determinants contribute to the development of multidrug-resistant (MDR) UPEC strains, which demonstrate cross-resistance to multiple antibiotics and present significant challenges for clinical management. Novel therapeutic strategies, such as efflux pump inhibitors, bacteriophage therapy, and genomic-guided precision medicine, are under investigation as potential solutions to address the growing global burden of MDR UPEC, alongside alternative non-antibiotic treatments. This review aims to provide a comprehensive overview of the genetic and regulatory pathways driving antibiotic resistance in UPEC, offering insights that may guide the development of effective treatment strategies and help mitigate the ongoing spread of antimicrobial resistance.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,951 View
- 111 Download
- 1 Crossref

Original Article
- Clinical Characteristics and Antimicrobial Susceptibility of Elderly Women with Acute Pyelonephritis
- Ji Kang Yun, Woong Bin Kim, Sang Wook Lee, Kwang Woo Lee, Jun Mo Kim, Young Ho Kim
- Urogenit Tract Infect 2020;15(3):71-78. Published online December 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.3.71
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: Acute pyelonephritis in older patients can lead to a poorer treatment response and prognosis. The objective of this study was to classify older female patients with acute pyelonephritis according to age and compare their clinical characteristics and antibiotic susceptibility.
Materials and Methods: In this retrospective study, 360 patients aged 65 years or older and hospitalized for acute pyelonephritis in a single tertiary medical facility from 2012 to 2016 were selected as research subjects. The patients were divided into three groups according to their age. Their clinical symptoms, blood tests and urinalysis, underlying diseases, causative organisms for urinary tract infections (UTIs), and antibiotic susceptibility were compared.
Results: One hundred and seventy-six patients aged 69.9±2.7 years, 142 patients aged 79.4±3.1 years, and 42 patients aged 87.3±3.1 years were assigned into the young-old, old-old, and oldest-old groups, respectively. The duration of hospitalization and fever due to acute pyelonephritis increased with age. On the other hand, the maximum body temperature was similar among the three groups. In blood tests, erythrocyte sedimentation rate and C-reactive protein increased with age. Among the underlying diseases, the incidence of diabetes and chronic renal disease was similar among the three groups, while cerebrovascular diseases, heart failure, and urinary stones were associated with aging. Older patients were more likely to have UTIs over the past year. Older groups showed a more significant decrease in sensitivity to carbapenems, amikacin, and ciprofloxacin.
Conclusions: Choosing appropriate antibiotics, considering the patientʼs age, is important when treating acute pyelonephritis.
- 3,723 View
- 24 Download


 KAUTII
KAUTII

 First
First Prev
Prev


