Search
- Page Path
- HOME > Search
Original Articles
- Efficacy of Urovaxom for Improving Chronic Pelvic Pain Syndrome Symptoms in Prostate Cancer Patients Who Underwent Radical Prostatectomy: A Multicenter, Prospective Cohort Study
- Jun-Koo Kang, Yun-Sok Ha, Sungchan Park, Tae Gyun Kwon, Tae-Hwan Kim
- Urogenit Tract Infect 2025;20(1):42-47. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550014007
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
Chronic pelvic pain syndrome (CPPS) is a multifactorial condition that can significantly diminish quality of life. Although some patients have reported persistent pelvic pain after radical prostatectomy (RP), the prevalence and direct causal relationship between CPPS and RP remain unclear. This multicenter prospective study aimed to evaluate the efficacy of Urovaxom for improving CPPS symptoms. Materials and Methods: A total of 52 prostate cancer patients who underwent RP were enrolled and administered Urovaxom (60 mg/day) for 12 weeks. Changes in National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI), overactive bladder symptom score (OABSS), International Prostate Symptom Score (IPSS), and inflammation markers (white blood cell [WBC], C-reactive protein [CRP]) were analyzed using the Wilcoxon signed-rank test.
Results
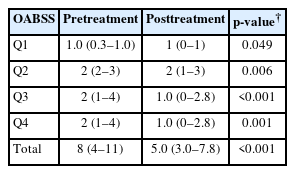
After 12 weeks of treatment, the NIH-CPSI total score significantly decreased from 19 (interquartile range [IQR], 16–23) to 12.5 (IQR, 8.0–16.8) (p<0.001). The OABSS total score decreased from 8 (IQR, 4–11) to 5 (IQR, 3.0–7.8), and the IPSS total score decreased from 13.5 (IQR, 10.0–22.8) to 10.5 (IQR, 5.0–17.0) (p<0.001). WBC levels showed a slight increase (p=0.028), but the clinical relevance of this change is uncertain and warrants further investigation. CRP changes were not statistically significant (p=0.274).
Conclusions
Urovaxom demonstrated significant efficacy in improving CPPS symptoms, particularly pain and reduced quality of life, in patients following RP. These findings suggest Urovaxom as a potential therapeutic option for CPPS after management using RP. -
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Addressing an Unmet Need in Postprostatectomy Care: Perspectives on Urovaxom
Byeong Jin Kang
Urogenital Tract Infection.2025; 20(2): 118. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,152 View
- 44 Download
- 2 Crossref

- Does Music Have a Calming Effect on Pain and Anxiety in Patients Undergoing Cystoscopy?
- Ye Chan Joo, Ji Eun Yu, Jae Hyun Baik, Young Seop Chang, Jin Bum Kim, Hyung Joon Kim, Dong Hoon Koh, Hong Wook Kim
- Urogenit Tract Infect 2024;19(1):3-9. Published online April 30, 2024
- DOI: https://doi.org/10.14777/uti.2024.19.1.3
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Purpose: Cystoscopy is a diagnostic test performed frequently in urology outpatient clinics. Despite the large number of inspections, the associated pain, discomfort, or anxiety can markedly affect patient compliance and adherence to subsequent surveillance protocols. This study conducted a prospective, randomized study to investigate the potential efficacy of music and pyuria on pain or anxiety during outpatient cystoscopy.
Materials and Methods: In this single-institution, randomized study, the participants were assigned to a music-intervention or non-music control group. The music-intervention group underwent an identical procedure with the addition of Johann Sebastian Bach’s “Air on the G String” from Suite No. 3 in D major, BWV 1068. Urinalysis was performed to determine if pyuria affects pain during the procedure.
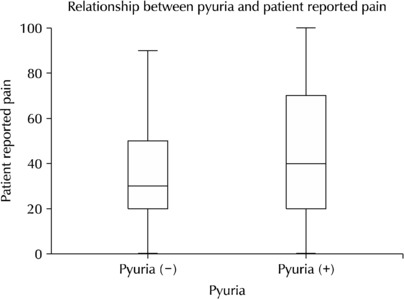
Results: The patient-reported outcomes, encompassing the changes in the STAI-X-1 (State-Trait Anxiety Inventory-X-1) scores, subjective levels of discomfort, embarrassment, satisfaction, and pain, were similar in the two groups. In contrast, the surgeons reported statistically significant differences in their evaluations of the same items as patient-reported outcomes of the two groups. The patient-reported pain showed no significant differences between the pyuria-negative group (0-2 and 3-5 WBC/HPF) and pyuria-positive group (>5 WBC/HPF).
Conclusions: The data from this study do not support the hypothesis that musical intervention during cystoscopy alleviates pain or anxiety to any significant extent. In addition, pyuria did not affect the patient’s reported pain. Nevertheless, a notable impact was observed in the surgeons’ assessments, suggesting that the musical accompaniment may alter the surgeons’ perception of patient pain and anxiety levels throughout the procedure.
- 2,849 View
- 34 Download

- Pelvic Pain in Men with Mycoplasma Genitalium
- Yumi Seo
- Urogenit Tract Infect 2024;19(1):16-23. Published online April 30, 2024
- DOI: https://doi.org/10.14777/uti.2024.19.1.16
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: There are debates about Mycoplasma genitalium (M. genitalium) causing prostate infection and inducing pelvic pains. Consequently, M. genitalium-associated pelvic pains were characterized and their manifestation in male pelvic pain syndrome (MPPS) was evaluated through a case-control study.
Materials and Methods: The presence of M. genitalium-associated pelvic pains was examined in 113 M. genitalium-infected men, and the typical presentations of mycoplasma-associated MPPS were characterized through a case-control study involving 80 mycoplasma-infected and 234 case-matched uninfected controls. Finally, changes in symptoms following antimicrobial treatments were compared between 27 cured and 14 persistently infected cases.
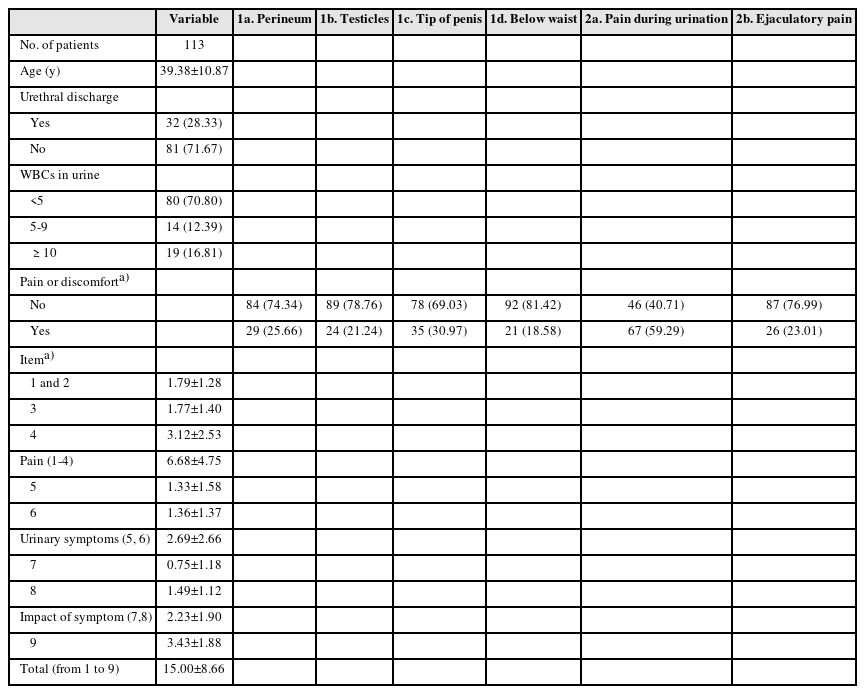
Results: Pain locations from 113 men were followed as items-1a for 25.7%, 1b for 21.2%, 1c for 31%, 1d for 18.6%, 2a for 59.3%, and 2b for 23% from the Korean National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) questionnaire. In addition, the sum scores from the pain domain, voiding domain and total score were 6.68±4.75, 2.69±2.66, and 15.00±8.66, respectively. Successful antibiotic therapy significantly reduced the total score from baseline (15.148±6.798 vs. 5.357±7.025, p=0.001). From the case-control study, mycoplasma-infected men had pains more frequently during urination (1c) and on the tip of the penis (2a) (all p=0.0001) than the controls.
Conclusions: It was found that M. genitalium infection is associated with clinically significant male pelvic pains, which improved with adequate antimicrobial therapies. Urethral irritation symptoms without pyuria may be the typical characteristics of mycoplasma-associated pelvic pains in MPPS.
- 7,235 View
- 33 Download

- The Feasibility of Radical Prostatectomy for Medication Refractory Chronic Prostatitis/Chronic Pelvic Pain Syndrome
- Seung Chan Jeong
- Urogenit Tract Infect 2022;17(3):76-80. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.76
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: The purpose of this study was to compare the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) scores of patients with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) given pharmacological treatment with those who additionally had prostate cancer and underwent surgical treatment.
Materials and Methods: From January 2000 to March 2021, a total of 7,650 patients were diagnosed with chronic prostatitis (N41.1) at our hospital, of which 234 patients were additionally diagnosed with prostate cancer. After excluding patients with severe benign prostatic hyperplasia (>100 g)-related lower urinary tract symptoms or neurological and psychiatric abnormalities, or advanced prostate cancer, 52 patients undergoing pharmacological treatment with a combination of drugs and 20 patients who underwent radical prostatectomy due to additional prostate cancer were included in the analysis. The NIH-CPSI scores of the two groups were compared at the first outpatient visit, 3 months, and 6 months after the first visit. The p-values were calculated using the Mann-Whitney U test, and the Wilcoxon signed rank test.
Results: Patients who underwent radical prostatectomy for prostate cancer showed significant reductions in the voiding and quality of life scores in the NIH-CPSI, but not the pain score at 3 months. After 6 months, there was a significant decrease in the overall NIH-CPSI. On the other hand, in the group on pharmacological therapy, the decrease was statistically significant only in the voiding score at 6 months. However, in the surgery group, 3 patients were found to be suffering from urinary incontinence, and 7 patients from erectile dysfunction.
Conclusions: Radical prostatectomy, therefore, appears to be a promising treatment that can be carefully considered for patients with refractory CP/CPPS who do not receive adequate treatment and thus have a poor quality of life.
- 3,087 View
- 9 Download

- Pilot Study of Cystochon® (Cranberry Extract, Chondroitin Sulfate, and Hyaluronic Acid Complex) in Interstitial Cystitis/Bladder Pain Syndrome
- Kwang Taek Kim, Jeong Woo Lee, Hyun-Sop Choe
- Urogenit Tract Infect 2022;17(2):36-41. Published online August 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.2.36
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study examined whether Cystochon® (cranberry extract, chondroitin sulfate, and hyaluronic acid complex) effectively improves the symptoms and problems of interstitial cystitis/bladder pain syndrome (IC/BPS) patients.
Materials and Methods: From December 2021 to May 2022, the medical records of IC/BPS patients who visited St. Vincent’s Hospital, Kyung Hee University Medical Center, or Gachon University Gil Medical Center were collected. For the treatment of IC/BPS, the patients were given pentosan polysulfate (PPS) for 12 weeks, with Cystochon® then added and maintained for an additional eight weeks. The OʼLeary–Sant symptom and problem index (Interstitial Cystitis Symptom Index [ICSI], Interstitial Cystitis Problem Index [ICPI]) was used to measure the treatment response.
Results: After 12 weeks of PPS treatment, ICSI and ICPI improved in all patients. After adding Cystochon® for eight weeks, the ICSI and ICPI indicators improved further. In the ICSI category, significant improvement in symptoms was confirmed in the total ICSI score, particularly in the Q4 (pain-related) questionnaire after adding Cystochon®. In the ICPI category, significant problem improvement was confirmed in the total ICPI score, particularly in the Q1 (frequent urination) and Q4 (pain-related) questionnaires. Although not statistically significant, the remaining indicators generally tended to improve.
Conclusions: The orally administered combination of cranberry extract, chondroitin sulfate, and hyaluronic acid (Cystochon®) may have a clinically positive effect in patients with IC/BPS. Better clinical improvement can be expected when it is added to the PPS treatment, especially in the category of bladder pain. -
Citations
Citations to this article as recorded by- Anti-inflammatory effect of sea buckthorn in an HCl-induced cystitis rat model
Hyun Suk Yoon, Juyeon Yu, Shinhoon Kang, Hana Yoon
Investigative and Clinical Urology.2025; 66(1): 67. CrossRef - Pharmacological Properties of Shionone: Potential Anti-Inflammatory Phytochemical against Different Diseases
Varun Jaiswal, Hae-Jeung Lee
Molecules.2023; 29(1): 189. CrossRef
- Anti-inflammatory effect of sea buckthorn in an HCl-induced cystitis rat model
- 5,989 View
- 15 Download
- 2 Crossref

Review
- UPOINT System: A Diagnostic/Therapeutic Algorithm for Chronic Prostatitis/Chronic Pelvic Pain Syndrome
- Phil Hyun Song
- Urogenit Tract Infect 2020;15(2):27-32. Published online August 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.2.27
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a common condition that significantly affects the quality of life. On the other hand, urologists find it challenging to treat this disorder effectively. To date, the Urinary, Psychosocial, Organ-Specific, Infection, Neurological/Systemic, and Tenderness (UPOINT) system is the only classification tool that can improve the treatment outcomes significantly compared to monotherapy. This review focused on the most recent advances in the diagnosis and treatment of CP/CPPS.
-
Citations
Citations to this article as recorded by- Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
Gwon Kyeong Lee, Kyoung Ha Jang, Woo Seop Seong, Byeong Jin Kang, Kyung Hwan Kim, Hong Koo Ha
Urogenital Tract Infection.2022; 17(3): 96. CrossRef
- Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
- 9,725 View
- 65 Download
- 1 Crossref


 KAUTII
KAUTII

 First
First Prev
Prev


