Search
- Page Path
- HOME > Search
Case Reports
- Klebsiella pneumoniae-Induced Emphysematous Prostatic Abscess Accompanied by a Spinal Cord Infarction: Case Report
- Seong Uk Jeh, Min Sung Choi, Chang Seok Kang, Dae Hyun Kim, Jae Hwi Choi, See Min Choi, Sung Chul Kam, Jeong Seok Hwa, Jae Seog Hyun
- Urogenit Tract Infect 2024;19(3):104-108. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448024012
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
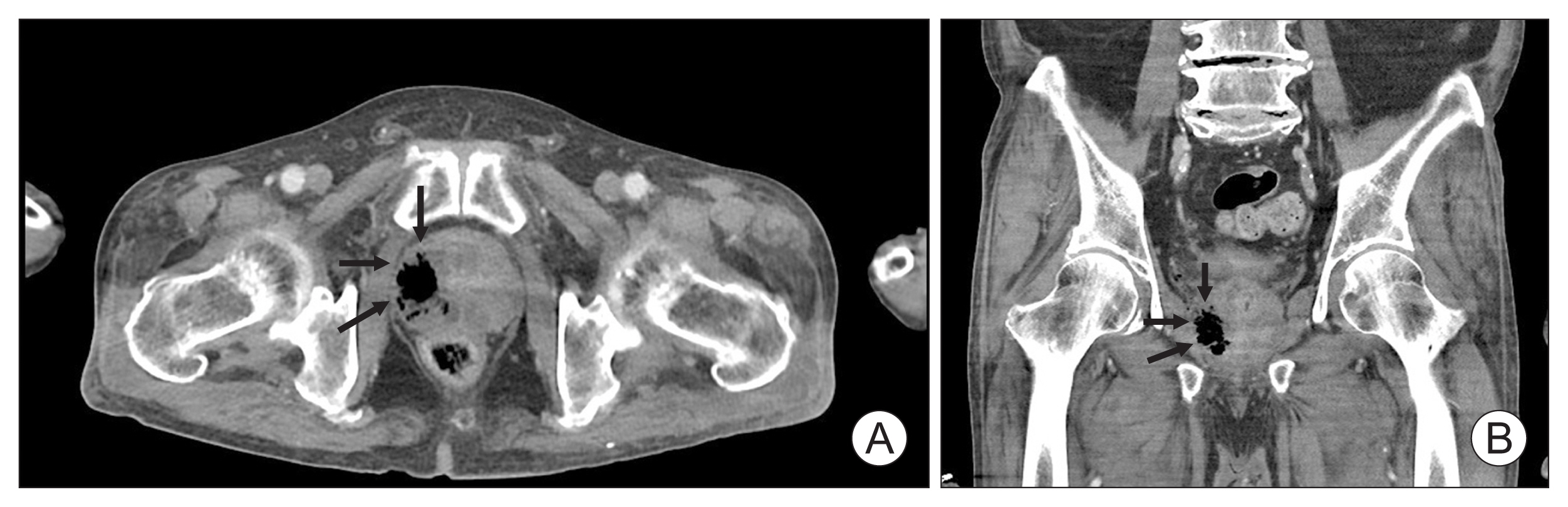
ePub - Various strains can be found in emphysematous prostatic abscesses (EPAs), but the most frequent causative organism is Klebsiella pneumoniae . Hypervirulent K. pneumoniae can disseminate to distant sites by forming a muco-polysaccharide network outside the capsule. Here, we present the first case of K. pneumoniae in an EPA accompanied by a spinal cord infarction. A 65-year-old man was referred to our hospital due to sudden-onset paraplegia after a 5-day history of fever, myalgia, and voiding difficulty. Abdominal computed tomography revealed a collection of air pockets in the prostate, and diffusion-weighted magnetic resonance imaging showed high signal intensity in the thoracic spinal cord. The patient was initially treated with antibiotics and surgical drainage. On the third hospital day, therapeutic heparin was added after discussion with a neurologist. The patient had no inflammatory symptoms, experienced some improvement in paraplegia, and was discharged on the 14th hospital day. This study adhered to the case report guidelines.
- 2,231 View
- 23 Download

- Case of Life-Threatening Pneumonia during the Treatment of a Patient with Acute Bacterial Prostatitis
- Kyung Kgi Park, Sung Dae Kim, Young-Joo Kim, Jung-Sik Huh
- Urogenit Tract Infect 2023;18(3):114-118. Published online December 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.3.114
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
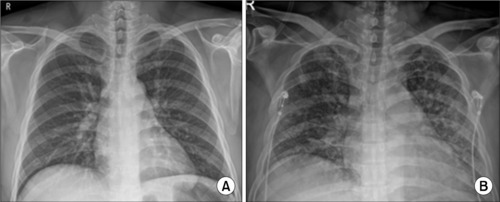
ePub - Acute bacterial prostatitis is an acute urinary tract infection associated with a bladder outlet obstruction or an immunosuppressed state. A 51-year-old man patient visited the hospital with fever, chills, and acute urinary retention that started the day before his visit after consuming a significant amount of alcohol. Conservative treatments, including catheterization for urinary drainage and antibiotics, were performed. On the third day of treatment for acute prostatitis, he complained of dyspnea. The level of oxygen differentiation was reduced significantly, and the tracheal insertion and ventilator were maintained after the radiological examination. The ventilator was discontinued, and the prostate abscess was operated on the eighth day of hospitalization. He was discharged without complications. This paper reports a case of life-threatening pneumonia and a prostate abscess during the treatment of a patient with acute bacterial prostatitis with a review of the relevant literature.
- 3,017 View
- 8 Download

Original Articles
- Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
- Gwon Kyeong Lee, Kyoung Ha Jang, Woo Seop Seong, Byeong Jin Kang, Kyung Hwan Kim, Hong Koo Ha
- Urogenit Tract Infect 2022;17(3):96-102. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.96
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study aimed to determine the treatment modality for prostatic abscesses according to size.
Materials and Methods: Twenty-five patients diagnosed with prostatic abscesses were retrospectively reviewed. All patients were treated with intravenous empirical and appropriate antibiotics according to culture results. They were grouped according to the size of the prostate abscess based on computed tomography results (group A, with prostate abscess ≤2 cm, n=10; group B, with prostate abscess size >2 cm, n=15), and their treatment modality and outcomes were compared.
Results: The prostatic abscess sizes were 1.31±0.37 and 3.49±1.06 cm for groups A and B, respectively. Prostate-specific antigen, prostatic volume, and comorbidity were not significantly different (p>0.05), whereas pelvic pain was significantly different (p=0.028). There was no difference in the microorganisms isolated from urine and blood culture, empirical antibiotics, and broad-spectrum antibiotics between the two groups (p>0.05). More patients in group B underwent transurethral abscess deroofing than those in group A (p=0.040). Patients in group B had a more extended hospitalization period and intravenous antibiotics duration than those in group A (p=0.024 and p=0.013, respectively). Group B had more cases of septic shock, intensive care unit admission, and mortality events than group A (p=0.024, p=0.001, and p=0.061, respectively). However, prostatic abscess recurrence and urological chronic complication did not significantly differ (p>0.05).
Conclusions: Appropriate use of antibiotics is crucial. This study shows that the treatment of patients with prostatic abscess >2 cm is more difficult, but transurethral abscess deroofing can lower mortality, prostatic abscess recurrence, and urological chronic complications.
- 4,856 View
- 27 Download

- Antibiotic Sensitivity of Bacterial Strains from Prostate Abscess Pus Aspirated Using Ultrasound Guidance
- Kyung Kgi Park, Sung Dae Kim, Young-Joo Kim, Jung-Sik Huh
- Urogenit Tract Infect 2022;17(1):26-30. Published online April 30, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.1.26
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: A prostate abscess is a rare occurrence often caused by immune dysfunction. The diagnostic modality for a prostate abscess is computed tomography or transrectal ultrasound. Transrectal ultrasound-guided aspiration is one such method. If treatment is dependent on the abscess size. This study examined the bacterial strains drained under transrectal ultrasound and their antibiotic sensitivity.
Materials and Methods: The medical records of eight patients diagnosed with a prostatic abscess and treated by transrectal ultrasound-guided aspiration from March 2009 to December 2020 were reviewed retrospectively. The general characteristics, associated diseases, and bacterial strains and their antibiotic sensitivities were identified in blood, urine, and pus cultures.
Results: Eight patients were hospitalized. The average age was 59.5±6.05 years, and the average length of hospitalization was 16.88±5.49 days; 75% had diabetes. No patients had catheterization, spinal injury, or prostate biopsy prior to diagnosis. The mean prostate volume was 47.05±27.3 ml, and the mean prostate abscess size was 2.08±0.83 ml. Under transrectal ultrasonography, the prostate abscess size was 5.43±5.31 ml, and catheters were inserted for treatment in four cases (50%). In the abscess culture test, Escherichia coli, Klebsiella pneumoniae, and Staphylococcus aureus were found in four, three, and one case, respectively. E. coli and K. pneumoniae responded well to amikacin treatment, while seven cases responded well to Piperacillin/Tazobactam treatment.
Conclusions: Prostate abscesses occur mainly in diabetic patients. The most common cultures are E. coli and K. pneumoniae. Intravenous injection of amikacin or Piperacillin/Tazobactam may be helpful as a treatment prior to bacterial identification. -
Citations
Citations to this article as recorded by- Case of Life-Threatening Pneumonia during the Treatment of a Patient with Acute Bacterial Prostatitis
Kyung Kgi Park, Sung Dae Kim, Young-Joo Kim, Jung-Sik Huh
Urogenital Tract Infection.2023; 18(3): 114. CrossRef - Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
Gwon Kyeong Lee, Kyoung Ha Jang, Woo Seop Seong, Byeong Jin Kang, Kyung Hwan Kim, Hong Koo Ha
Urogenital Tract Infection.2022; 17(3): 96. CrossRef
- Case of Life-Threatening Pneumonia during the Treatment of a Patient with Acute Bacterial Prostatitis
- 3,113 View
- 9 Download
- 2 Crossref


 KAUTII
KAUTII

 First
First Prev
Prev


