Previous issues
- Page Path
- HOME > Browse Articles > Previous issues
Editorial
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- Koo Han Yoo
- Urogenit Tract Infect 2025;20(1):1-3. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2025edi01
- 1,783 View
- 24 Download

Review Articles
- Emerging Insights Into Microbiome Therapeutics for Urinary Tract Infections: A Narrative Review
- Hoonhee Seo, Md Abdur Rahim, Indrajeet Barman, Mohammed Solayman Hossain, Hanieh Tajdozian, Fatemeh Ghorbanian, Md Sarower Hossen Shuvo, Jiho Choi, Sukyung Kim, Heejo Yang, Ho-Yeon Song
- Urogenit Tract Infect 2025;20(1):4-16. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2448034017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary tract infections (UTIs) are among the most common bacterial infections worldwide, affecting millions annually and posing a significant global health concern. Traditional therapies for UTIs are becoming increasingly ineffective due to rising drug resistance and their tendency to disrupt the host's healthy microbiota, leading to further side effects. Consequently, there is an urgent need to develop alternative therapeutic agents that differ from conventional regimens and have fewer or no side effects. In this context, microbiome therapeutics offer a promising solution, given their demonstrated efficacy against various infectious diseases. Advances in scientific technology, particularly next-generation sequencing, have deepened our understanding of urinary microbiome dynamics, revealing a complex interplay within the urobiome that influences the onset and progression of UTIs. Uropathogenic bacteria do not solely cause UTIs; shifts in the composition of the urinary microbiome and interactions within the microbial community, known as host-microbiota interactions, also play a significant role. Although recent studies underscore the potential of targeting the urinary microbiome to manage UTIs and related complications, this field is still emerging and faces numerous regulatory and technical challenges. Further in-depth and comprehensive research is required to advance this pioneering concept into clinical practice.
-
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Efficacy and safety of N-acetylcysteine vs. probiotics in in-vivo biofilm prevention on ureteral stents: a prospective randomized controlled pilot in vivo study
Iqbal Singh, Himanshu Agrawal, Shailender Maurya, Himanshu Tanwar, Sanjay Gupta, N. P. Singh
International Urology and Nephrology.2025; 58(3): 811. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 14,182 View
- 168 Download
- 2 Crossref

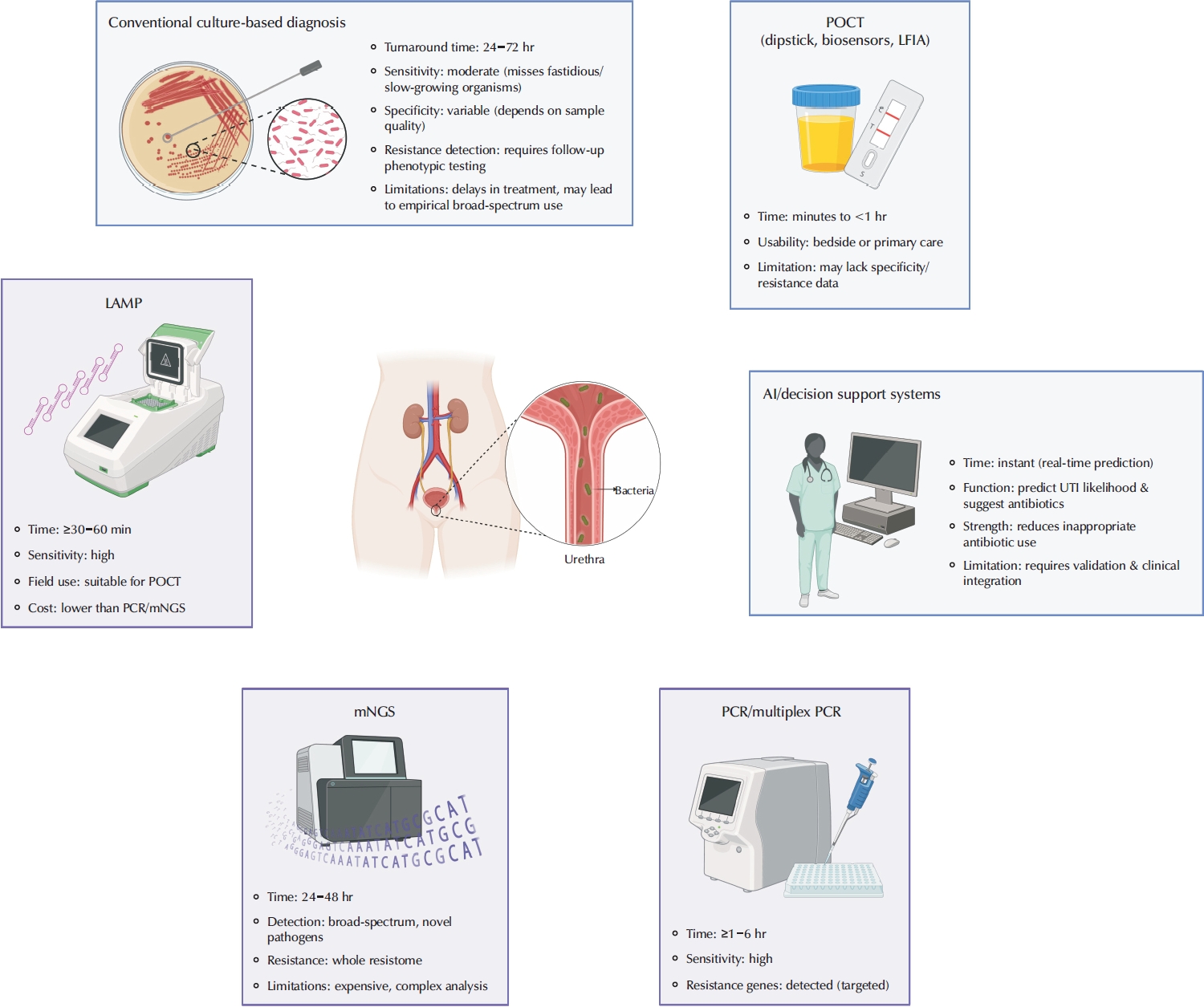
- Advances in the Diagnosis of Urinary Tract Infection: A Narrative Review
- Juan Victor Ariel Franco, Nicolás Meza
- Urogenit Tract Infect 2025;20(1):17-27. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550020010
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary tract infections are among the most frequent bacterial infections, significantly impacting patient morbidity and healthcare resources. Prompt and accurate diagnosis is crucial to ensure effective treatment, prevent complications such as pyelonephritis or sepsis, and reduce inappropriate antibiotic use, contributing to antimicrobial resistance (AMR). Despite consensus across international guidelines from organizations, challenges persist, particularly in distinguishing true infections from asymptomatic bacteriuria or nonspecific symptoms, especially in older adults. Recent advancements in diagnostic technology have emerged to address these limitations, including molecular diagnostics, point-of-care testing (POCT), and artificial intelligence (AI)-driven predictive models. Molecular techniques, notably polymerase chain reaction, loop-mediated isothermal amplification, and metagenomic next-generation sequencing, offer enhanced sensitivity and specificity, rapid detection times, and comprehensive identification of pathogens and resistance profiles. POCT innovations, such as lateral flow immunoassays, enzymatic-based rapid tests, and novel biosensors, facilitate prompt bedside diagnosis, although specificity challenges remain. Meanwhile, AI and machine learning models demonstrate significant potential for risk stratification, prediction of infection, and improving antibiotics prescription practices yet face barriers related to validation, practical integration, and clinical acceptability. Despite promising developments, significant gaps remain, including limited real-world implementation evidence, high costs, and insufficient data from diverse populations. Further rigorous clinical studies, economic evaluations, and practical implementation assessments are urgently required. Addressing these research gaps could substantially improve patient outcomes, optimize antibiotic stewardship, and reduce the global burden of AMR.
-
Citations
Citations to this article as recorded by- Diagnosis of urinary tract infections in the pediatric population – current practices, advances and progress
Maria Bitsori, Roza-Ioanna Poulaki, Emmanouil Galanakis
Expert Review of Anti-infective Therapy.2026; : 1. CrossRef - Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
- Diagnosis of urinary tract infections in the pediatric population – current practices, advances and progress
- 10,119 View
- 302 Download
- 2 Crossref

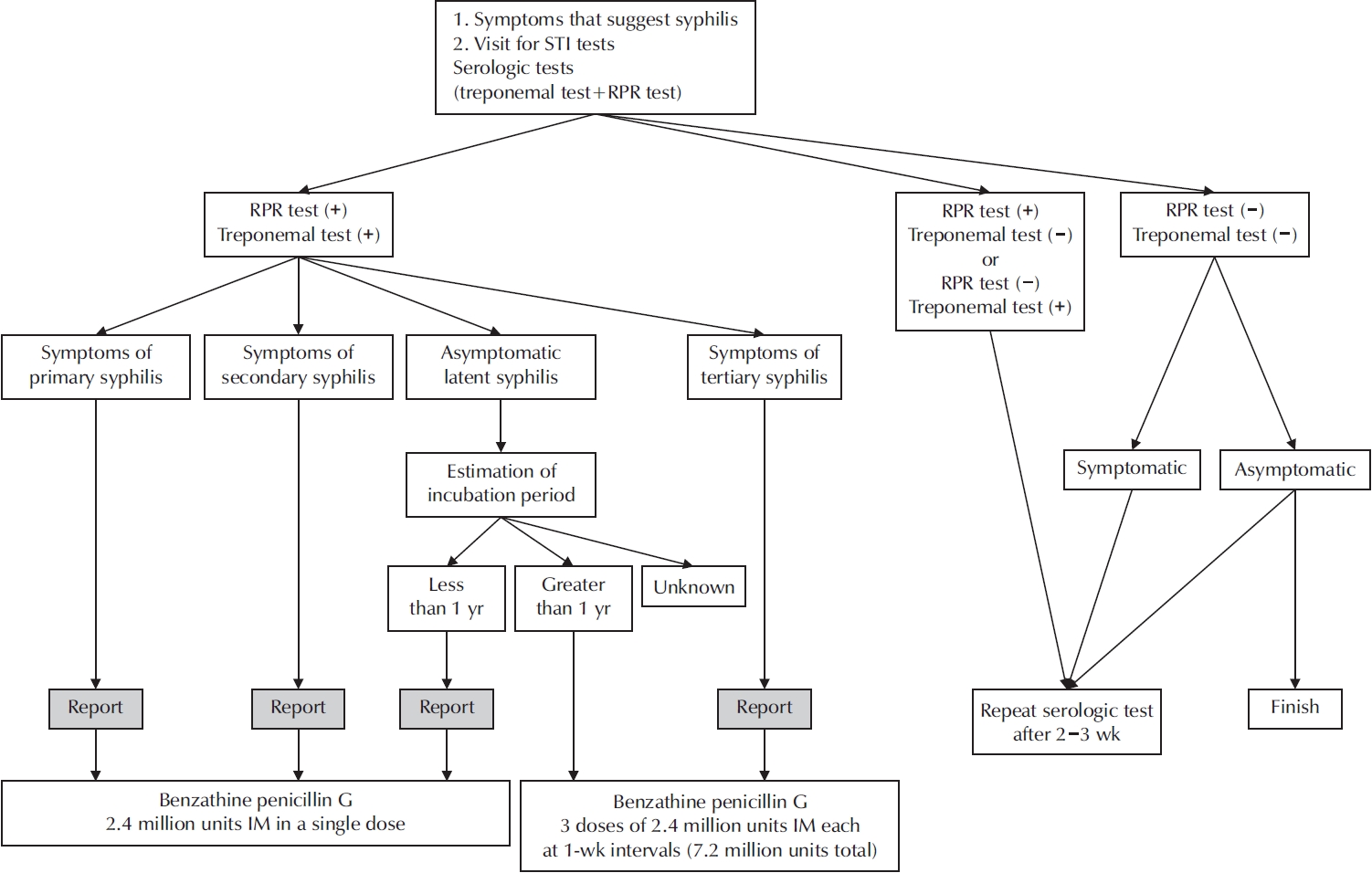
- A Narrative Review of Syphilis Notification Systems in Korea: Change to Mandatory Surveillance System
- Seung-Ju Lee, Jin Bong Choi
- Urogenit Tract Infect 2025;20(1):28-33. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550004002
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - New cases of syphilis are clearly showing an increasing trend worldwide. However, in a sentinel surveillance system, the collection of information on disease outbreaks is limited, making it difficult to understand the overall outbreak situation and perform detailed analyses of patients' demographic characteristics and disease stages. In accordance with the revision of the Infectious Disease Prevention Act, syphilis was converted from a grade 4 infectious disease subject to sentinel surveillance to a grade 3 infectious disease subject to mandatory surveillance from January 1, 2024, with all medical institutions required to report syphilis diagnosis within 24 hours.
-
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Adult Syphilis: A Narrative Review of Clinical Insights and Public Health Implications in Urology
Seung-Ju Lee, Jin Bong Choi
Urogenital Tract Infection.2025; 20(3): 123. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,279 View
- 38 Download
- 2 Crossref

Original Articles
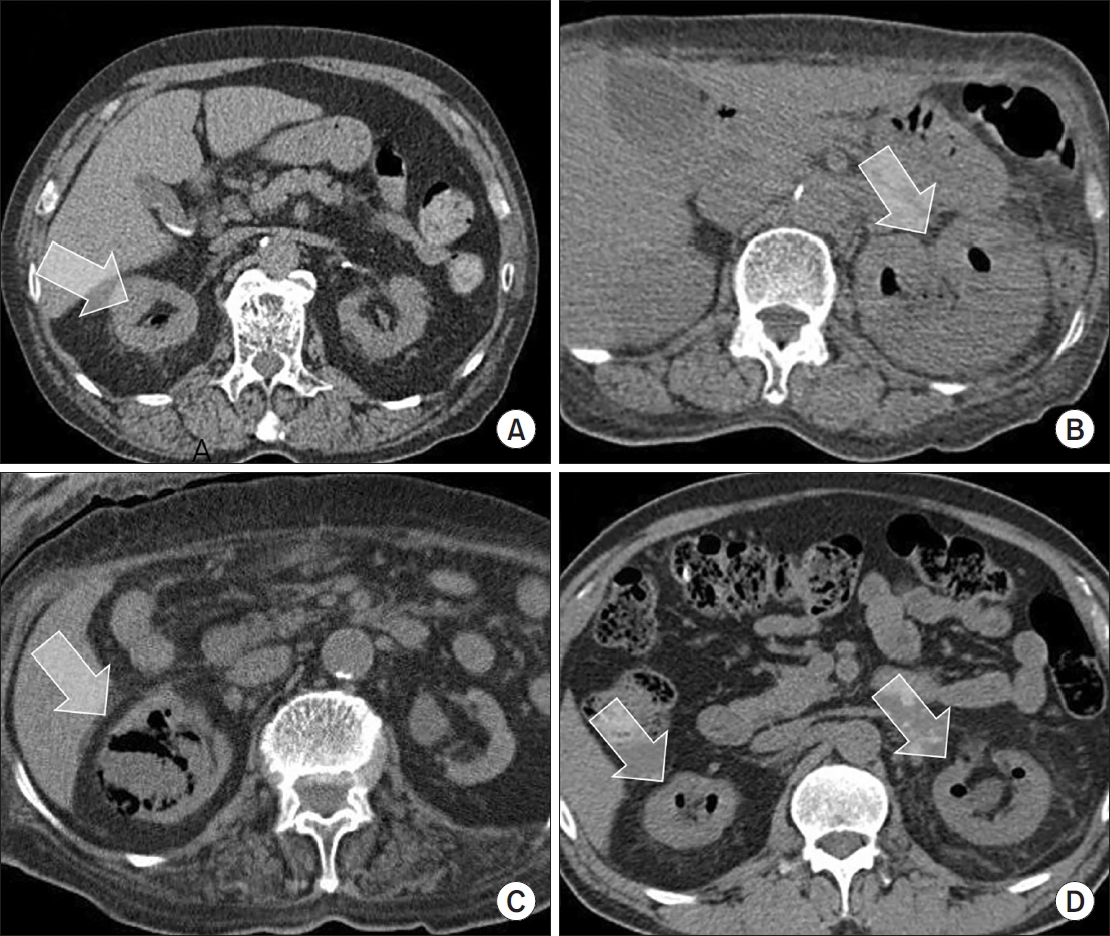
- Mortality and Risk Factors for Emphysematous Pyelonephritis in Korea: A Multicenter Retrospective Cohort Study
- Seung-Kwon Choi, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
- Urogenit Tract Infect 2025;20(1):34-41. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550006003
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
Emphysematous pyelonephritis (EPN) is a life-threatening disease requiring immediate treatment. This multicenter retrospective cohort study aimed to analyze the mortality rate and risk factors associated with EPN. Materials and Methods: Between January 2011 and February 2021, 217 patients diagnosed with EPN via computed tomography who visited 14 teaching hospitals were retrospectively analyzed. Clinical data, including age, sex, comorbidities, Huang and Tseng classification, hydronephrosis, acute kidney injury, blood and urine tests, surgical interventions, percutaneous drainage, and conservative treatments, were compared between the survival and death groups. Risk factors for mortality due to EPN were analyzed using univariate and multivariate methods.
Results
The mean age of survivors and deceased patients was 67.8 and 69.0 years, respectively (p=0.136). The sex distribution (male/female) was 48/146 and 8/15, respectively (p=0.298). Of the 217 patients, 23 died, resulting in a mortality rate of 10.6%. In univariate analysis, the Huang and Tseng classification (p=0.004), platelet count (p=0.005), and acute kidney injury (p=0.007) were significantly associated with mortality from EPN. In multivariate analysis, only the Huang and Tseng classification (p=0.029) was identified as a risk factor. Mortality rates according to the Huang and Tseng classification were as follows: class I (5.88%), class II (7.50%), class IIIa (14.28%), class IIIb (25.00%), and class IV (23.07%).
Conclusions
EPN is associated with a high mortality rate. Among various clinical factors, the Huang and Tseng classification was the most significant indicator for predicting mortality. -
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 3,368 View
- 60 Download
- 1 Crossref

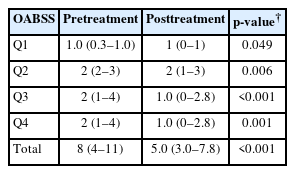
- Efficacy of Urovaxom for Improving Chronic Pelvic Pain Syndrome Symptoms in Prostate Cancer Patients Who Underwent Radical Prostatectomy: A Multicenter, Prospective Cohort Study
- Jun-Koo Kang, Yun-Sok Ha, Sungchan Park, Tae Gyun Kwon, Tae-Hwan Kim
- Urogenit Tract Infect 2025;20(1):42-47. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550014007
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
Chronic pelvic pain syndrome (CPPS) is a multifactorial condition that can significantly diminish quality of life. Although some patients have reported persistent pelvic pain after radical prostatectomy (RP), the prevalence and direct causal relationship between CPPS and RP remain unclear. This multicenter prospective study aimed to evaluate the efficacy of Urovaxom for improving CPPS symptoms. Materials and Methods: A total of 52 prostate cancer patients who underwent RP were enrolled and administered Urovaxom (60 mg/day) for 12 weeks. Changes in National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI), overactive bladder symptom score (OABSS), International Prostate Symptom Score (IPSS), and inflammation markers (white blood cell [WBC], C-reactive protein [CRP]) were analyzed using the Wilcoxon signed-rank test.
Results
After 12 weeks of treatment, the NIH-CPSI total score significantly decreased from 19 (interquartile range [IQR], 16–23) to 12.5 (IQR, 8.0–16.8) (p<0.001). The OABSS total score decreased from 8 (IQR, 4–11) to 5 (IQR, 3.0–7.8), and the IPSS total score decreased from 13.5 (IQR, 10.0–22.8) to 10.5 (IQR, 5.0–17.0) (p<0.001). WBC levels showed a slight increase (p=0.028), but the clinical relevance of this change is uncertain and warrants further investigation. CRP changes were not statistically significant (p=0.274).
Conclusions
Urovaxom demonstrated significant efficacy in improving CPPS symptoms, particularly pain and reduced quality of life, in patients following RP. These findings suggest Urovaxom as a potential therapeutic option for CPPS after management using RP. -
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Addressing an Unmet Need in Postprostatectomy Care: Perspectives on Urovaxom
Byeong Jin Kang
Urogenital Tract Infection.2025; 20(2): 118. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,152 View
- 44 Download
- 2 Crossref

Case Report
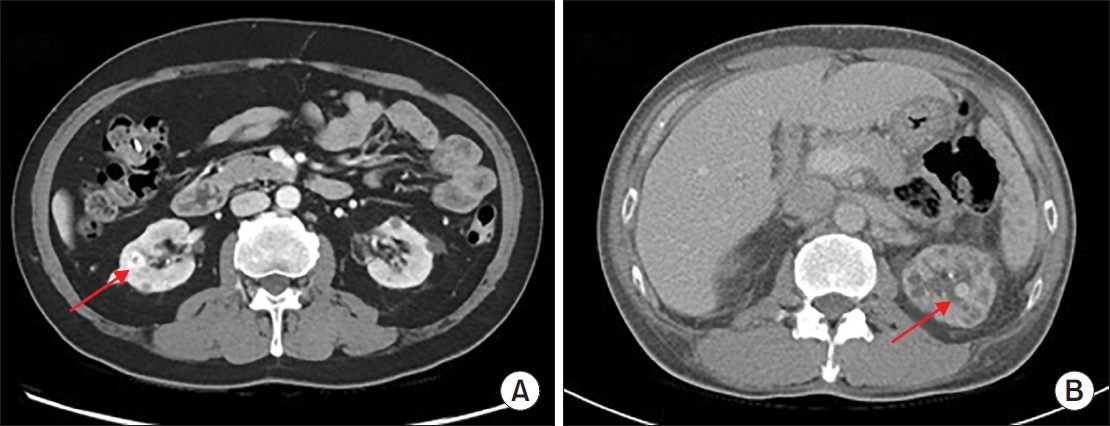
- Hemangioma Mistaken for Renal Cell Carcinoma in a Patient With End-Stage Renal Disease: A Case Report
- Hyung-Lae Lee, Dong-Gi Lee, Jeong Woo Lee, Jeonghyouk Choi
- Urogenit Tract Infect 2025;20(1):48-51. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550008004
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Hemangiomas are rare, benign vascular neoplasms that are more common in patients with end-stage renal disease. Here, we describe 2 cases of hemangioma misdiagnosed as renal cell carcinoma before renal transplantation. The key finding in our case was the misdiagnosis of hemangiomas as renal cell carcinoma based on computed tomography and magnetic resonance imaging in patients with end-stage renal disease. Because living transplantation was planned for our patients, we performed rapid surgical resection of the heterogeneously enhancing renal masses to avoid delays in transplantation. Our case highlights the importance of rapid surgical resection of enhanced renal masses to confirm diagnosis, thereby avoiding delays in patients scheduled for renal transplantation.
-
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 2,050 View
- 18 Download
- 1 Crossref

Letter to the Editor
- A Commentary on “Outbreak of Cystoscopy-Related Urinary Tract Infections With Pseudomonas aeruginosa in South Korea, 2022: A Case Series”
- Byoungkyu Han
- Urogenit Tract Infect 2025;20(1):52-54. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550010005
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 1,529 View
- 18 Download
- 1 Crossref


 KAUTII
KAUTII



 First
First Prev
Prev


