-
Mortality and Risk Factors for Emphysematous Pyelonephritis in Korea: A Multicenter Retrospective Cohort Study
-
Seung-Kwon Choi, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2025;20(1):34-41. Published online April 30, 2025
-
DOI: https://doi.org/10.14777/uti.2550006003
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose
Emphysematous pyelonephritis (EPN) is a life-threatening disease requiring immediate treatment. This multicenter retrospective cohort study aimed to analyze the mortality rate and risk factors associated with EPN.
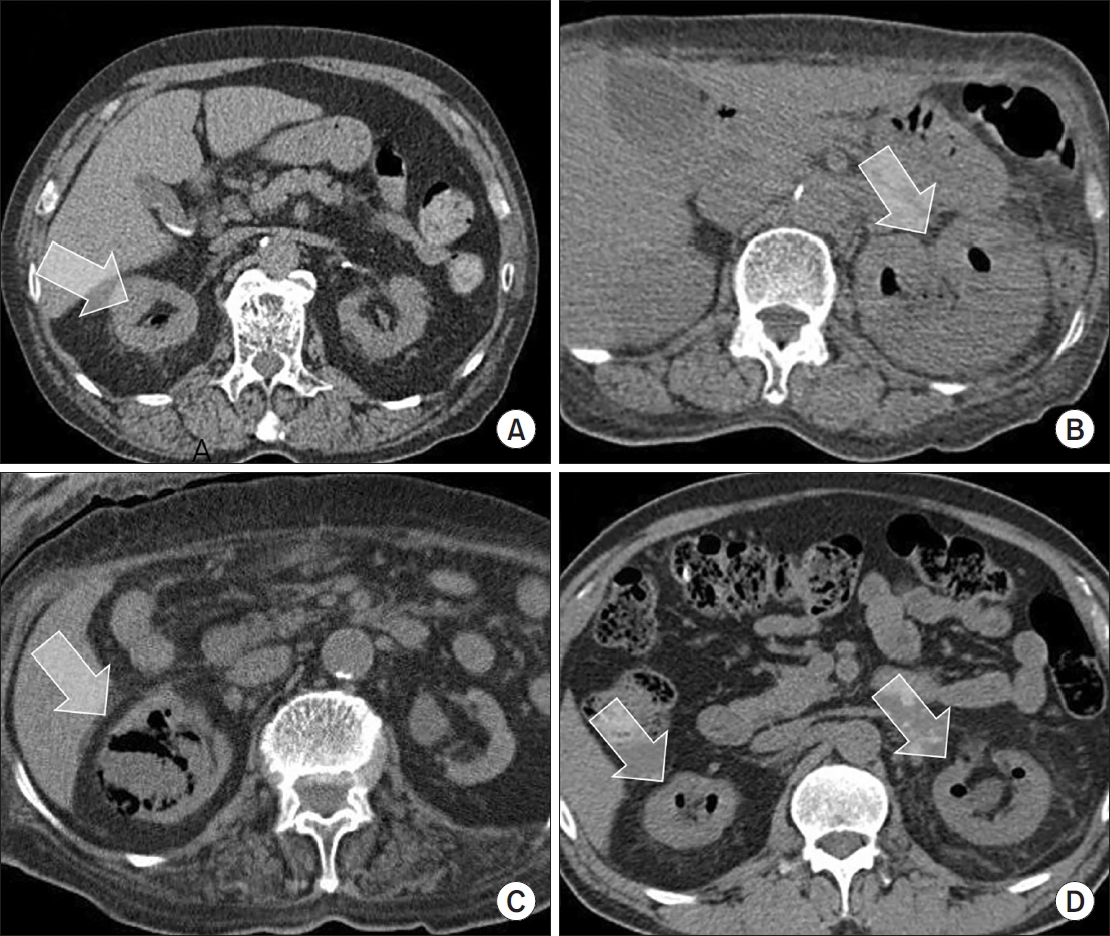
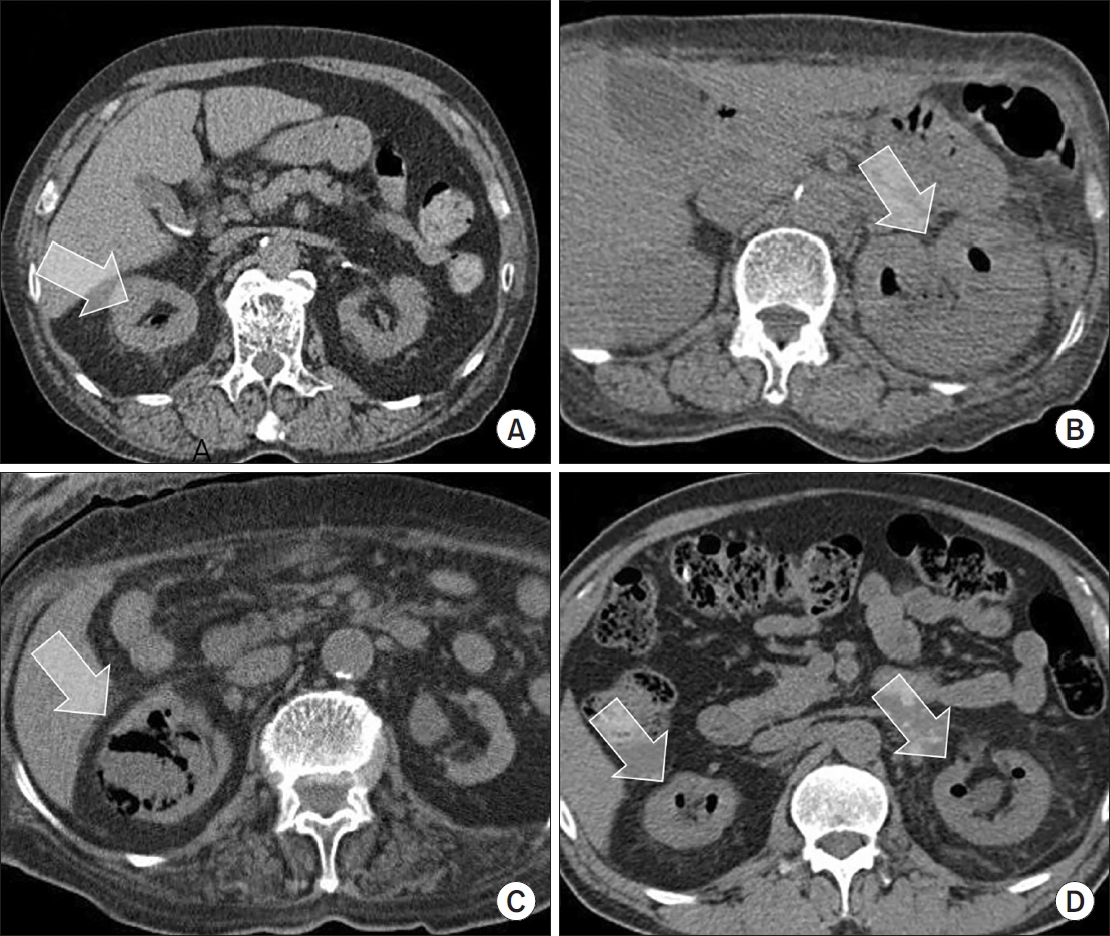
Materials and Methods: Between January 2011 and February 2021, 217 patients diagnosed with EPN via computed tomography who visited 14 teaching hospitals were retrospectively analyzed. Clinical data, including age, sex, comorbidities, Huang and Tseng classification, hydronephrosis, acute kidney injury, blood and urine tests, surgical interventions, percutaneous drainage, and conservative treatments, were compared between the survival and death groups. Risk factors for mortality due to EPN were analyzed using univariate and multivariate methods.
Results
The mean age of survivors and deceased patients was 67.8 and 69.0 years, respectively (p=0.136). The sex distribution (male/female) was 48/146 and 8/15, respectively (p=0.298). Of the 217 patients, 23 died, resulting in a mortality rate of 10.6%. In univariate analysis, the Huang and Tseng classification (p=0.004), platelet count (p=0.005), and acute kidney injury (p=0.007) were significantly associated with mortality from EPN. In multivariate analysis, only the Huang and Tseng classification (p=0.029) was identified as a risk factor. Mortality rates according to the Huang and Tseng classification were as follows: class I (5.88%), class II (7.50%), class IIIa (14.28%), class IIIb (25.00%), and class IV (23.07%).
Conclusions
EPN is associated with a high mortality rate. Among various clinical factors, the Huang and Tseng classification was the most significant indicator for predicting mortality.
-
Citations
Citations to this article as recorded by  - Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef
-
3,370
View
-
60
Download
-
1
Crossref
-
Differences in Urine Microbiome of Acute Cystitis and Chronic Recurrent Cystitis in Women
-
Woong Bin Kim
-
Urogenit Tract Infect 2023;18(1):1-7. Published online April 30, 2023
-
DOI: https://doi.org/10.14777/uti.2023.18.1.1
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- The diagnosis of urinary tract infection (UTI) relies on urine culture tests to identify aerobic or anaerobic urinary tract pathogens. This method has limitations in identifying anaerobic bacteria, and there is uncertainty in identifying all bacteria. A new next-generation sequencing (NGS) method has gradually helped overcome these limitations, and the microorganisms present in the human urinary tract are gradually being revealed. This review introduces studies on the microbiome analyzed using NGS of urine from patients with acute cystitis and recurrent UTIs and discusses whether NGS may reveal the pathophysiology of the disease.
-
Characteristics and Treatment Trends for Emphysematous Pyelonephritis in Korea: A 10-Year Multicenter Retrospective Study
-
Seung-Kwon Choi, Koo Han Yoo, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
-
Urogenit Tract Infect 2021;16(2):49-54. Published online August 31, 2021
-
DOI: https://doi.org/10.14777/uti.2021.16.2.49
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study examined the characteristics, current treatment trends, and outcomes of patients with emphysematous pyelonephritis (EPN) in Korea.
Materials andMethods: Two hundred and seventeen patients diagnosed with EPN were evaluated using abdominal computed tomography in 2011-2021 at 15 institutes in Korea. The patients’ demographic and clinical characteristics, treatment modalities, and treatment outcomes were analyzed. The total study period was divided arbitrarily into groups A (2011-2014), B (2015-2017), and C (2018-2021) to analyze the trends in the EPN treatment.
Results: The mean age of the patients was 65.1 years; there were more female patients (74.2%) than male patients. The overall mortality rate was 10.6%. Ninety-five (43.8%), 98 (45.2%), and 24 (11.0%) patients were treated with medical, minimally invasive, and surgical management, respectively; the corresponding mortality rates were 13.7%, 6.1%, and 16.7%. There was no significant change in the proportion of patients treated with medical management over time (group A=46.5%, group B=47.0%, and group C=38.8%). The proportion of patients treated with minimally invasive management gradually increased over time (group A=35.2%; group B=43.9%; group C=55.0%), while those who underwent surgical management decreased gradually over time (group A=18.3%, group B=9.1%, and group C=6.3%). No differences in mortality rates were observed between the groups.
Conclusions: EPN with medical and minimally invasive management had a relatively high treatment success rate, which increased gradually, while surgical management decreased gradually over time in Korea. The mortality rate was relatively lower than that reported in studies published before the 2010s.
-
Clinical Characteristics and Antimicrobial Susceptibility of Elderly Women with Acute Pyelonephritis
-
Ji Kang Yun, Woong Bin Kim, Sang Wook Lee, Kwang Woo Lee, Jun Mo Kim, Young Ho Kim
-
Urogenit Tract Infect 2020;15(3):71-78. Published online December 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.3.71
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: Acute pyelonephritis in older patients can lead to a poorer treatment response and prognosis. The objective of this study was to classify older female patients with acute pyelonephritis according to age and compare their clinical characteristics and antibiotic susceptibility.
Materials and Methods: In this retrospective study, 360 patients aged 65 years or older and hospitalized for acute pyelonephritis in a single tertiary medical facility from 2012 to 2016 were selected as research subjects. The patients were divided into three groups according to their age. Their clinical symptoms, blood tests and urinalysis, underlying diseases, causative organisms for urinary tract infections (UTIs), and antibiotic susceptibility were compared.
Results: One hundred and seventy-six patients aged 69.9±2.7 years, 142 patients aged 79.4±3.1 years, and 42 patients aged 87.3±3.1 years were assigned into the young-old, old-old, and oldest-old groups, respectively. The duration of hospitalization and fever due to acute pyelonephritis increased with age. On the other hand, the maximum body temperature was similar among the three groups. In blood tests, erythrocyte sedimentation rate and C-reactive protein increased with age. Among the underlying diseases, the incidence of diabetes and chronic renal disease was similar among the three groups, while cerebrovascular diseases, heart failure, and urinary stones were associated with aging. Older patients were more likely to have UTIs over the past year. Older groups showed a more significant decrease in sensitivity to carbapenems, amikacin, and ciprofloxacin.
Conclusions: Choosing appropriate antibiotics, considering the patientʼs age, is important when treating acute pyelonephritis.
-
How Women Evaluate Syndromic Recurrent Urinary Tract Infections
-
Woong Bin Kim, Sang Wook Lee, Kwang Woo Lee, Jun Mo Kim, Young Ho Kim, Min Eui Kim
-
Urogenit Tract Infect 2019;14(2):46-54. Published online August 30, 2019
-
DOI: https://doi.org/10.14777/uti.2019.14.2.46
-
-
 Abstract Abstract
 PDF PDF
- Purpose: To investigate the clinical manifestations of patients with the principal complaint of syndromic recurrent urinary tract infection (UTI), correlate these symptoms with the results of urine cultures, and identify the characteristics that can be used to differentiate UTI from similar diseases.
Materials and Methods: A total of 212 consecutive patients with syndromic recurrent UTIs over a 24 month period were evaluated. The major symptoms were recorded using the UTISA questionnaire and VAS. The patients were divided into group A (n=98; positive urine and urethral swab cultures) and group B (n=114; negative cultures), and the symptoms were compared. For group B, cystoscopy was used to diagnose 61 patients who complained of pain levels ≥6 on the VAS.
Results: The proportion of patients with the classic symptoms of UTI (dysuria, urinary frequency, lower abdominal discomfort during bladder filling, and urgency) was similar in groups A and B. Significantly more patients complained of urethral pain in group B, and significantly fewer patients had gross hematuria, low back pain, a post-voiding sensation of residual urine, and general symptoms compared to group A. Of the 61 patients with a VAS ≥6, 29, 28, and four were diagnosed with bladder pain syndrome, interstitial cystitis, and urethral pain syndrome, respectively.
Conclusions: In patients with syndromic recurrent UTI, the classic symptoms were not sufficiently characteristic to allow bacterial cystitis to be differentiated from other bladder diseases. Diagnostic cystoscopy and VAS can assist in making a differential diagnosis in patients with non-bacterial syndromic recurrent UTIs.
-
Recent Antimicrobial Susceptibilities for Uropathogenic Escherichia coli in Patients with Community Acquired Urinary Tract Infections: A Multicenter Study
-
Woong Bin Kim, Kyu Hyoung Cho, Sang Wook Lee, Hee Jo Yang, Jong Hyun Yun, Kwang Woo Lee, Jun Mo Kim, Young Ho Kim, Youn Soo Jeon, Min Eui Kim
-
Urogenit Tract Infect 2017;12(1):28-34. Published online April 30, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: The aim of this study was to determine the prevalence and disease-specific antimicrobial susceptibility of Escherichia coli in urinary tract infections (UTIs).
Materials and Methods: A total of 862 patients older than 18 years of age, who were diagnosed with UTI between January 2013 and December 2015, were included. The results of urine culture, prevalence of extended-spectrum beta lactamase (ESBL)-producing E. coli, and antimicrobial susceptibility by disease were also examined.
Results: A total of 862 uropathogens were isolated. Among then, E. coli accounted for 756 (87.7%) isolates. The susceptibility rates of E. coli to the following antimicrobial agents were as follows: ampicillin 29.4%, cefazolin 70.5%, ceftazidime 75.1%, cefotaxime 75.0%, cefepime 76.2%, cefoxitin 88.8%, amoxicillin-clavulanic acid 63.6%, trimethoprim-sulfamethoxazole 60.6%, gentamicin 71.4%, ciprofloxacin 73.0%, piperacillin/tazobactam 93.9%, amikacin 99.2%, imipenem 99.1%, and ertapenem 99.3%. The frequency of ESBL-producing E. coli strains was 24.6%. The antimicrobial susceptibility of UTI varied by each disease, but without statistical significance.
Conclusions: It is necessary to regularly examine the disease-specific resistance rates to determine the appropriate empiric antibiotic treatment, and the national antibiotic usage policies must be reorganized according to the data obtained from these studies.
|