-
Asymptomatic Bacteriuria in Older Adults – Diagnosis, Management, and Future Directions: A Narrative Review
-
Ki Hong Kim, Hee Jo Yang
-
Urogenit Tract Infect 2025;20(2):58-66. Published online August 31, 2025
-
DOI: https://doi.org/10.14777/uti.2550002001
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader
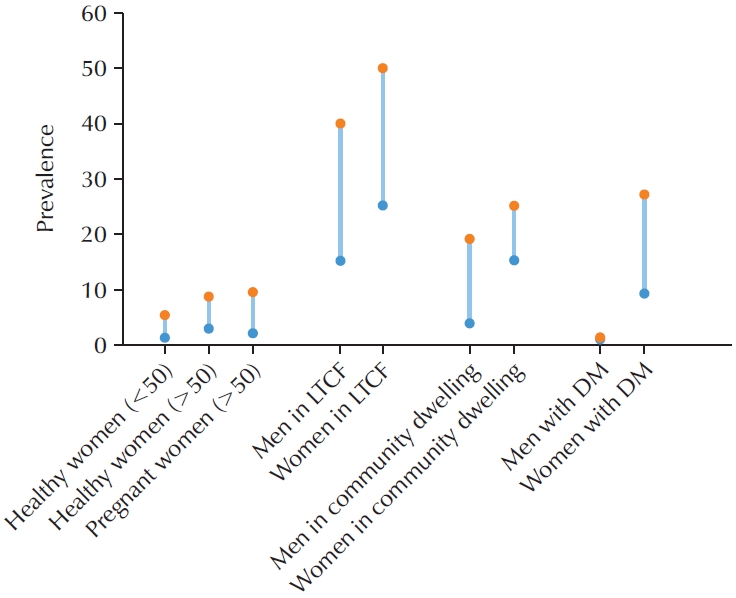
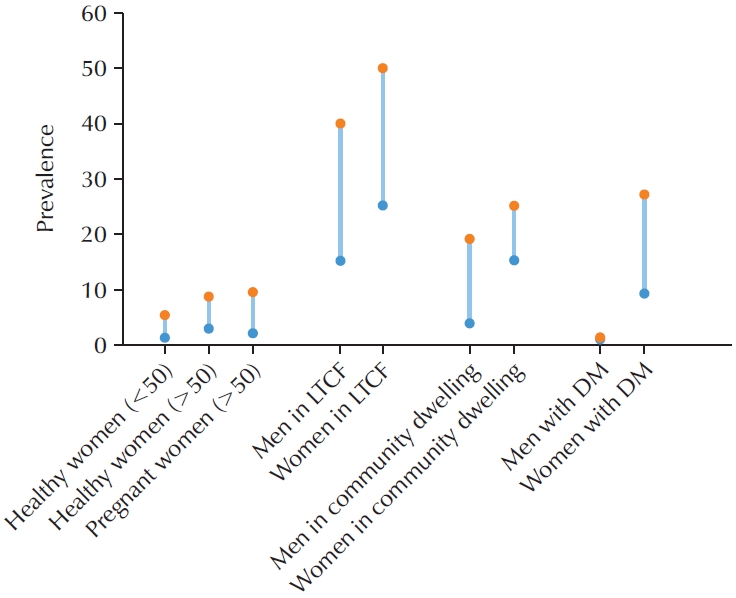
- Asymptomatic bacteriuria (ASB) is defined as the presence of bacteria in the urine in the absence of urinary tract infection (UTI) symptoms. The prevalence of ASB increases with advancing age, particularly among older patients with underlying health conditions. ASB is especially common among residents of long-term care facilities; however, distinguishing ASB from symptomatic UTI in this population remains a significant clinical challenge. The frequent occurrence of ASB often results in unnecessary antibiotic administration, thereby contributing to the development of antibiotic resistance. Current clinical guidelines recommend screening for and treating ASB only in certain circumstances, such as prior to urological procedures or in pregnant women. There is a pressing need for improved diagnostic approaches to differentiate ASB more accurately from UTI, particularly in older adults. Reducing unnecessary urine testing and inappropriate antibiotic use may help prevent over-treatment and minimize associated risks, including Clostridium difficile infection and increased antimicrobial resistance.
-
Citations
Citations to this article as recorded by  - Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
-
11,534
View
-
116
Download
-
1
Crossref
-
Artificial Intelligence for Autonomous Robotic Surgery in Urology: A Narrative Review
-
Dae Young Lee, Hee Jo Yang
-
Urogenit Tract Infect 2024;19(3):80-88. Published online December 31, 2024
-
DOI: https://doi.org/10.14777/uti.2448020010
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Artificial intelligence (AI) has emerged as a transformative force in various sectors, including medicine, where it processes high-dimensional data to improve diagnostics and treatment outcomes. This review explores AI applications in urological surgery, highlighting advancements such as image classification and robotic assistance in surgical procedures. AI has demonstrated exceptional diagnostic accuracy, with some systems achieving up to 99.38% in detecting prostate cancer. Additionally, AI facilitates real-time anatomical recognition and instrument delineation, increasing surgical precision. While current robotic systems operate under human supervision, ongoing research aims to advance autonomous surgical capabilities. The future of AI in robotic surgery is promising, especially regarding the possibility of improved outcomes; nonetheless, challenges related to autonomy, safety, and ethics remain.
-
Prophylactic Antimicrobial Therapy and Antimicrobial Stewardship in Urologic Surgery
-
Hee Jo Yang
-
Urogenit Tract Infect 2023;18(1):8-14. Published online April 30, 2023
-
DOI: https://doi.org/10.14777/uti.2023.18.1.8
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Postoperative infectious complications are a worrying problem for surgeons. Urological surgery has a higher risk of postoperative urinary tract infection than other surgeries because of the common use of various types of catheters. Due to the recent increase in antibiotic resistance, antimicrobial stewardship recommends using appropriate antibiotics for a suitable period. It is generally advocated that prescribing antibiotics in the absence of infection is equivalent to the inappropriate use of antibiotics. Based on numerous studies reported by several academic societies, appropriate use of antibiotics before surgery has been suggested. It was confirmed that using antibiotics according to these guidelines reduces the use of antibiotics without increasing the incidence of postoperative infectious complications. Furthermore, endourological surgery reports have proved the efficacy of antibiotics given once before surgery. Differences in antibiotic resistance by region must be taken into consideration when selecting the appropriate antibiotic type.
-
The Effects of Short-Chain Fatty Acids in Urological Diseases
-
Hee Jo Yang, Doo Sang Kim
-
Urogenit Tract Infect 2022;17(1):8-13. Published online April 30, 2022
-
DOI: https://doi.org/10.14777/uti.2022.17.1.8
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- The gut microbiome, believed to serve as a second genome within the human body, is involved in the regulation of several metabolic processes. These include human gene expression, development, nutrition and homeostasis. Dysbiosis, is an imbalance in the gut microbiome, which is known to be associated with various disease conditions such as Crohn's disease and Clostridium infections. The gut microbiota communicates with the host through a variety of biomolecules, nutrient signal-independent pathways, and epigenetic mechanisms. The gut microbiota supports the digestion and absorption of food, metabolizes fiber into bioactive short-chain fatty acids (SCFA), produces vitamins and nutrients, maintains gut integrity, and modulates host immunity. Among the above, there has been great interest in SCFA in microbiome research due to its beneficial effects on the intestinal barrier function and systemic anti-inflammatory effects. Recent reports have also indicated the role of SCFA in obesity, insulin resistance, and type 2 diabetes. While SCFA are associated with reduced risk of various diseases, dysbiosis and altered SCFA fermentative pathways could result in disease. This article is a review on the role of SCFA in urological diseases.
-
Citations
Citations to this article as recorded by  - Role of microbiome and its metabolite, short chain fatty acid in prostate cancer
Hee Jo Yang, Jae Heon Kim
Investigative and Clinical Urology.2023; 64(1): 3. CrossRef - The Urinary Microbiome; Axis Crosstalk and Short-Chain Fatty Acid
Hee Jo Yang, Doo Sang Kim, Kwang Woo Lee, Young Ho Kim
Diagnostics.2022; 12(12): 3119. CrossRef
-
2,687
View
-
13
Download
-
2
Crossref
-
Recent Antimicrobial Susceptibilities for Uropathogenic Escherichia coli in Patients with Community Acquired Urinary Tract Infections: A Multicenter Study
-
Woong Bin Kim, Kyu Hyoung Cho, Sang Wook Lee, Hee Jo Yang, Jong Hyun Yun, Kwang Woo Lee, Jun Mo Kim, Young Ho Kim, Youn Soo Jeon, Min Eui Kim
-
Urogenit Tract Infect 2017;12(1):28-34. Published online April 30, 2017
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: The aim of this study was to determine the prevalence and disease-specific antimicrobial susceptibility of Escherichia coli in urinary tract infections (UTIs).
Materials and Methods: A total of 862 patients older than 18 years of age, who were diagnosed with UTI between January 2013 and December 2015, were included. The results of urine culture, prevalence of extended-spectrum beta lactamase (ESBL)-producing E. coli, and antimicrobial susceptibility by disease were also examined.
Results: A total of 862 uropathogens were isolated. Among then, E. coli accounted for 756 (87.7%) isolates. The susceptibility rates of E. coli to the following antimicrobial agents were as follows: ampicillin 29.4%, cefazolin 70.5%, ceftazidime 75.1%, cefotaxime 75.0%, cefepime 76.2%, cefoxitin 88.8%, amoxicillin-clavulanic acid 63.6%, trimethoprim-sulfamethoxazole 60.6%, gentamicin 71.4%, ciprofloxacin 73.0%, piperacillin/tazobactam 93.9%, amikacin 99.2%, imipenem 99.1%, and ertapenem 99.3%. The frequency of ESBL-producing E. coli strains was 24.6%. The antimicrobial susceptibility of UTI varied by each disease, but without statistical significance.
Conclusions: It is necessary to regularly examine the disease-specific resistance rates to determine the appropriate empiric antibiotic treatment, and the national antibiotic usage policies must be reorganized according to the data obtained from these studies.
|