Abstract
Syphilis continues to pose a major global public health concern, with more than 7 million cases reported worldwide in 2022, and its incidence continues to rise in numerous regions. In Korea, the shift from sentinel to universal notification in 2024 has revealed a markedly greater disease burden, particularly among men who have sex with men and among younger adults, underscoring changing epidemiological patterns and the urgent need for revised control strategies. In urological practice, syphilis presents with a wide range of often misleading symptoms, including painless genital ulcers, urethritis, and sexual dysfunction, that frequently resemble other genitourinary disorders and complicate diagnostic evaluation. Accurate identification relies on integrating a thorough clinical assessment with serologic testing while remaining alert to diagnostic challenges such as early latent infection, serofast states, and human immunodeficiency virus coinfection. Penicillin G remains the mainstay of therapy, with treatment regimens tailored to the stage of disease and to the presence or absence of central nervous system involvement. Effective partner notification, targeted screening, and consistent follow-up are essential to prevent reinfection and limit further transmission. At a public health level, a multifaceted strategy—strengthened surveillance systems, focused testing in high-risk populations, and embedding syphilis screening within broader sexually transmitted infection care frameworks—is critical to curbing its resurgence. In summary, prompt recognition, adherence to evidence-based management, and coordinated public health measures, together with ongoing advances in diagnostics and prevention, remain fundamental to reducing the continued spread of syphilis and mitigating its impact on both individual and population health.
-
Keywords: Sexually transmitted diseases, Syphilis, Public health, Epidemiology, Urology
HIGHLIGHTS
Adult syphilis has re-emerged as a global concern, and its incidence in Korea has risen significantly after the shift to nationwide surveillance in 2024. Urologists play a pivotal role in facilitating early recognition, as patients with syphilis may present with genital ulcers, urethritis, or sexual dysfunction that can imitate other urologic illnesses. Reliable diagnosis necessitates carefully integrating comprehensive clinical assessment with serological laboratory tests, and penicillin remains the treatment of choice for all disease stages. Ongoing follow-up and management of sexual partners are crucial for reducing the risk of reinfection and curbing transmission. Promising future strategies include artificial intelligence-powered risk assessment, point-of-care diagnostic technologies, and syphilis vaccine development, which may contribute to more effective disease management.
INTRODUCTION
Syphilis, caused by the spirochete
Treponema pallidum (
T. pallidum), is a significant sexually transmitted infection (STI) with the potential to affect multiple organ systems—such as the nervous, cardiovascular, and genitourinary systems—if it is not treated [
1,
2]. Although effective antibiotic treatments are widely available, syphilis persists as a public health issue. After a substantial decrease in incidence following penicillin’s introduction in the mid-20th century, the disease has resurged worldwide in recent decades [
3,
4]. This resurgence has been especially marked among younger adults, men, and men who have sex with men (MSM), largely attributable to evolving sexual behaviors, reduced condom use, and increased rates of human immunodeficiency virus (HIV) coinfection [
5,
6].
Within urology, syphilis holds clinical importance due to its frequent involvement of the genitourinary tract. In addition to the classic painless chancre seen during primary infection, syphilis may present with urethritis, genital ulcers, sexual dysfunction, and inflammatory conditions of the prostate or seminal vesicles [
7]. These manifestations are often subtle and may be missed, which can result in delayed diagnosis. Furthermore, early latent syphilis is asymptomatic, highlighting the necessity of serologic testing for identification [
8]. It is essential that urologists recognize the disease’s wide range of clinical features, understand diagnostic methods, implement appropriate treatment, and adhere to follow-up protocols. Prompt detection and management are vital for improving patient outcomes and for limiting further transmission. This review outlines recent epidemiological developments in adult syphilis—with emphasis on modifications to Korea’s national surveillance system—and explores its clinical presentations, diagnosis, therapeutic approaches, and public health relevance from a urological standpoint.
EPIDEMIOLOGY AND CHANGES IN SURVEILLANCE SYSTEMS
Globally, the annual incidence of syphilis exceeded 7 million cases in 2022, with many countries subsequently documenting a persistent rise in infections. Findings from a recent systematic analysis demonstrate a consistent global increase in syphilis incidence over the past decade, with an average annual growth rate of approximately 6%–8% [
9]. In Asia, this upward trend is particularly evident. In Japan, a rapid post–COVID-19 resurgence of syphilis has been documented, with reported cases reaching record levels since 2022, primarily driven by increased transmission among young heterosexuals and MSM [
10]. These findings suggest that changes in sexual behavior patterns and reduced STI screening during the pandemic may have contributed to the accelerated spread observed in recent years.
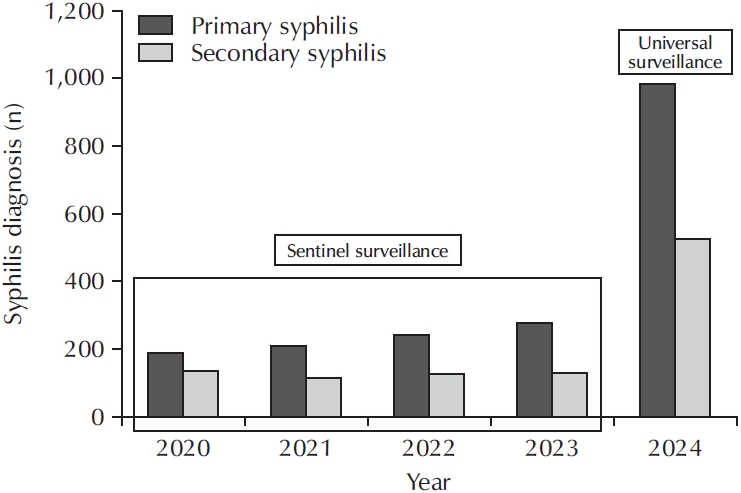
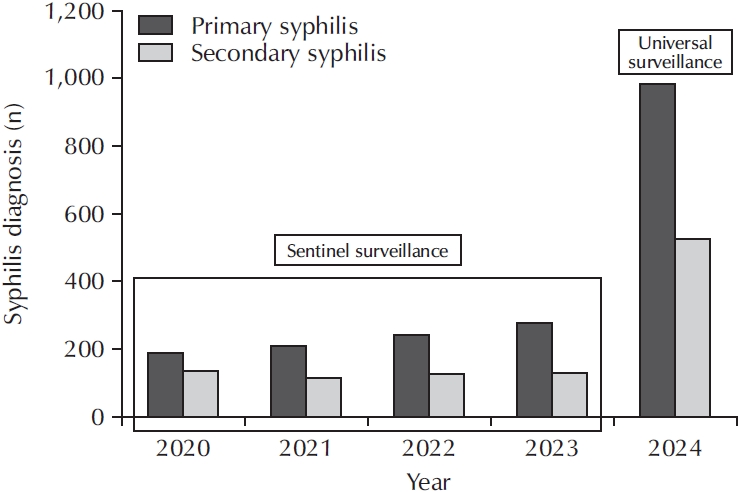
This pattern is also evident in Korea. According to the Korea Disease Control and Prevention Agency, following the implementation of a nationwide surveillance system in 2024, reported syphilis cases surged to approximately 2,800, compared to only a few hundred cases recorded under the former sentinel surveillance model [
11] (
Fig. 1). While the number of reported cases nearly doubled between 2019 and 2024, this increase should be interpreted with caution because the expansion of the surveillance system in 2024 incorporated early latent and tertiary syphilis, which had previously been excluded from national reporting. The current incidence rate is 5.4 per 100,000 population, with the greatest prevalence among men in their 20s and 30s, as well as in MSM populations [
11].
This apparent rise therefore reflects both a genuine increase in infections and enhanced case detection following modifications in the surveillance framework. The previous sentinel surveillance system documented only primary, secondary, and congenital syphilis, which resulted in substantial underreporting of early and late latent infections. The implementation of universal notification now ensures that all syphilis stages are included, providing a more accurate and comprehensive depiction of the epidemiological burden in Korea [
12]. These improved data are essential for developing evidence-based prevention strategies and refining both diagnostic and therapeutic approaches.
Recent national surveillance data illustrate noteworthy changes in Korea's syphilis epidemiology over the last 5 years. Between 2019 and 2024, annual reported cases nearly doubled from around 1,500 to 2,800 [
11]. The continuing increase in cases cannot be solely attributed to improved reporting, indicating that transmission is actively expanding within the community. In addition, a shift in the demographics of those affected has emerged. Historically, syphilis was predominantly reported among MSM, but there is an ongoing rise in heterosexual transmission, highlighting evolving sexual behaviors and network patterns within the population [
9,
11].
Sex-based differences in infection patterns have become even more marked. Men still represent approximately 70%–75% of reported cases in the most recent surveillance data, yet the proportion of cases in women is steadily rising [
11]. This pattern carries significant public health implications, especially concerning the risk of congenital syphilis, and highlights the urgent need to strengthen antenatal screening and prevention programs. Additionally, age distribution analysis reveals a significant clustering of cases among individuals aged 20–39 years, indicating the necessity for focused sexual health education and earlier testing strategies for younger age groups.
Patterns of geographic distribution further highlight the distinct regional variability present in the syphilis epidemic in Korea. Metropolitan centers such as Seoul, Busan, and Incheon consistently report the highest incidence rates, which are associated with elevated population density, highly connected sexual networks, and a broader spectrum of sexual behaviors [
11]. These observations reinforce the critical need for interventions designed to address the specific epidemiological context of each region through localized public health strategies.
Taken together, these epidemiological trends demonstrate the dynamic shifts occurring in syphilis transmission in Korea and signal the necessity for comprehensive prevention efforts. Broadening the scope of routine screening to include populations beyond the conventional high-risk groups, promoting the integration of syphilis screening into both primary care and urology, and developing specifically tailored public health initiatives are fundamental in controlling the growing disease burden.
PATHOGENESIS AND TRANSMISSION MECHANISMS
T. pallidum, a helical spirochete, exhibits high infectivity and can initiate infection with very limited exposure [
8]. The primary mode of transmission is sexual contact, during which the pathogen infiltrates microabrasions present on the skin or mucosal surfaces. After penetration, the bacterium undergoes local multiplication and disseminates through both lymphatic and hematogenous pathways, resulting in extensive systemic involvement [
13].
The natural progression of syphilis is marked by well-defined stages. Typically, after an incubation period of approximately 3 weeks (range, 10–90 days) postexposure, primary syphilis presents with a localized, painless ulcer termed a chancre. If not treated, the infection often advances to secondary syphilis within 6–12 weeks, which is characterized by systemic findings such as skin rashes, lymphadenopathy, and mucosal lesions. Subsequent to this, a latent phase occurs in which the infection is asymptomatic but can still be identified serologically. In the absence of therapy, a subset of patients may eventually develop tertiary syphilis, potentially affecting the cardiovascular system, central nervous system, or other organ systems decades after initial exposure [
1,
8].
CLINICAL MANIFESTATIONS IN UROLOGY
Within urology, syphilis presents with a diverse array of clinical features, many resembling other genitourinary conditions and resulting in notable diagnostic difficulties (
Table 1). The hallmark lesion of primary syphilis is a solitary, painless chancre that is generally firm and indurated, usually arising on the glans penis, foreskin, scrotum, or pubic region [
8]. Less frequently, lesions may emerge on the urethral meatus, perineum, or rectal mucosa, particularly among individuals who participate in receptive anal intercourse [
14]. Despite typically resolving on their own within 3 to 6 weeks, these ulcers do not eradicate the underlying systemic infection in untreated patients [
7]. Regional lymphadenopathy, most commonly of the inguinal nodes, is often seen alongside the chancre and presents as painless enlargement of the nodes, sometimes leading to confusion with other STIs or local traumatic events [
7,
8,
14].
Secondary syphilis commonly emerges 6 to 12 weeks after the initial infection and is defined by systemic symptoms including generalized rash, malaise, and lymphadenopathy [
7,
8]. From a urological standpoint, mucocutaneous lesions referred to as condylomata lata often appear in the perineal, perianal, or scrotal areas. These broad-based, moist, highly infectious plaques closely mimic condyloma acuminata caused by human papillomavirus, which can result in misdiagnosis [
7,
14]. Urethral involvement occurs with some frequency and may present with urethral discharge, dysuria, increased urinary frequency, or perineal discomfort. These symptoms are often indistinguishable from nongonococcal urethritis, chronic prostatitis, or other inflammatory diseases [
14]. Rarely, syphilitic balanitis or erosive lesions of the glans penis may develop, further complicating the differential diagnosis [
15].
Chronic inflammation or vascular complications related to late-stage syphilis may also disrupt sexual function [
5]. Erectile dysfunction, premature ejaculation, or reduced libido can arise from neurovascular injury secondary to endarteritis or the direct involvement of the cavernous nerves [
16-
18]. Since these symptoms are frequently subtle and show gradual progression, healthcare providers may incorrectly assign them to more prevalent conditions such as diabetes mellitus, atherosclerosis, or psychogenic disorders, causing delays in accurate diagnosis [
7,
14].
Given the wide range of clinical presentations, clinicians must maintain a high index of suspicion, particularly in patients who exhibit persistent or unexplained urogenital symptoms that are unresponsive to conventional therapy [
19]. Clinical scenarios such as recurrent urethritis, atypical genital ulcerations, unexplained genital dermatoses, or idiopathic sexual dysfunction should raise suspicion for syphilis, particularly in individuals with risk factors including multiple sexual partners, MSM activity, or a prior history of other STIs. A comprehensive sexual history and targeted physical examination—with careful evaluation of genital, perineal, and mucocutaneous regions—should be routinely accompanied by serologic testing to confirm the diagnosis [
7,
14].
DIAGNOSTIC STRATEGIES
Definitive diagnosis of syphilis necessitates an integration of clinical evaluation, thorough sexual history, and laboratory investigations. Given that clinical features are frequently nonspecific and can mirror other genitourinary conditions, serologic testing remains fundamental to confirming the diagnosis. Serologic assays are generally categorized as nontreponemal and treponemal tests, which provide complementary information regarding detection, disease stage, and monitoring response to therapy [
1,
4].
Nontreponemal tests, such as the venereal disease research laboratory test and the rapid plasma reagin test, serve as standard initial screening tools [
1,
8]. These assays detect antibodies to lipoidal antigens derived from both host cells and
T. pallidum, with titers that reflect the current activity of the disease. Nontreponemal tests are essential for monitoring therapeutic efficacy, as a fourfold decline in titer is generally considered indicative of successful treatment [
4,
20]. Nevertheless, false-negative results may appear in early primary syphilis prior to the development of detectable antibody levels, and also in late-stage disease due to spontaneous reduction in titers. In addition, false-positive results can be observed in individuals with autoimmune conditions, during pregnancy, or in the context of chronic infections [
20].
Treponemal tests, such as the fluorescent treponemal antibody absorption test, the
T. pallidum particle agglutination assay, and enzyme immunoassays (EIAs), demonstrate greater specificity and are utilized to confirm the diagnosis [
4,
14]. Following a positive result, treponemal test reactivity generally persists for life, rendering these assays unsuitable for monitoring treatment response or detecting reinfection.
Currently, 2 diagnostic algorithms are recommended [
4,
21]. The standard algorithm initiates with a nontreponemal test, followed by a confirmatory treponemal test. By contrast, the reverse sequence algorithm starts screening with a treponemal EIA or chemiluminescent immunoassay, then uses a nontreponemal test to evaluate disease activity. When test results are discordant (for example, treponemal positive but nontreponemal negative), additional evaluation with a second treponemal test or clinical correlation is necessary. Selection of the diagnostic algorithm should consider patient demographics, prevailing disease rates, and available laboratory capabilities [
21].
In urologic settings, diagnostic evaluation is recommended for patients presenting with persistent or unexplained urethritis, atypical genital ulcers, or unclear sexual dysfunction, particularly among individuals with a history of high-risk sexual exposure. Cerebrospinal fluid analysis is indicated when neurosyphilis is suspected based on clinical findings [
4,
14,
20]. Additional modalities, such as polymerase chain reaction testing or histopathologic assessment, can be valuable in cases with atypical clinical features or inconclusive serological tests [
13].
Test interpretation must always be integrated with the overall clinical scenario. Patients with early latent syphilis may show positive serological findings without symptoms, requiring cautious, ongoing follow-up. Additionally, a “serofast” condition, defined as persistent low non-treponemal titers despite effective treatment, may develop in up to 15% of cases and should not be confused with therapeutic failure [
4,
20]. Moreover, coinfection with HIV has the potential to modify serological profiles, possibly causing delayed seroconversion or atypical antibody titer responses [
14].
TREATMENT AND FOLLOW-UP
The primary aim of syphilis therapy is the complete elimination of
T. pallidum, which serves to stop disease progression, avert complications, and reduce transmission [
22]. Penicillin G remains the preferred treatment at all stages of infection, and to date, there have been no reports of clinically significant resistance [
4,
20]. The therapeutic regimen, choice of dose, and treatment duration are tailored according to disease stage, length of infection, nervous system involvement, and coexisting medical conditions (
Table 2).
For early syphilis, including primary, secondary, and early latent phases, a single intramuscular dose of 2.4 million units of benzathine penicillin G is indicated [
4,
14,
20]. If late latent syphilis is present or the duration of infection is unclear, the same dosage should be administered weekly for 3 successive weeks. For individuals diagnosed with neurosyphilis, ocular syphilis, or otosyphilis, a high-dose intravenous regimen capable of penetrating the blood–brain barrier is necessary, most commonly involving 18–24 million units of aqueous crystalline penicillin G delivered daily by intravenous infusion for 10–14 days [
4,
20]. Patients with documented penicillin allergy may be prescribed alternatives such as doxycycline (100 mg orally twice a day for 14 days in early syphilis or 28 days for late syphilis) or ceftriaxone (1–2 g daily for 10–14 days) [
4,
14,
20]. Nevertheless, for pregnant women and those with neurosyphilis, penicillin desensitization followed by standard treatment continues to be favored, given the limited data supporting the efficacy of alternative agents in these populations [
4,
14,
20,
21].
Monitoring treatment response is crucial for evaluating therapeutic efficacy and for the early detection of reinfection or inadequate therapy. Follow-up serologic assessment is generally conducted at 6, 12, and 24 months after treatment for early syphilis, with a fourfold reduction in nontreponemal titers serving as a reliable marker of satisfactory response [
21]. In cases of late syphilis, the decline in serologic markers may be delayed, and persistent low-level titers (“serofast” state) do not always indicate unsuccessful treatment. However, an increase in titers should lead to assessment for possible reinfection or inadequate response to therapy.
Partner notification and simultaneous treatment represent fundamental measures for the effective control of syphilis, as untreated partners remain a source for both reinfection and ongoing transmission [
5]. All sexual contacts occurring within 90 days preceding diagnosis should be provided with empiric therapy, regardless of their serologic status. It is essential for patients to avoid sexual contact for at least 7 days following treatment and until complete resolution of all lesions [
21].
Management must be individualized for patients with comorbidities or specific populations. In individuals co-infected with HIV, the recommended penicillin regimen remains unchanged, but more intensive follow-up is required due to a higher risk of suboptimal treatment response [
4]. Pregnant patients must receive timely therapy to reduce the risk of congenital syphilis; desensitization to penicillin should be pursued in cases of allergy [
14]. Furthermore, urologists should recognize that persistent sexual dysfunction following therapy may suggest irreversible neurovascular injury or the presence of other comorbidities, necessitating comprehensive evaluation.
PUBLIC HEALTH IMPLICATIONS AND FUTURE PERSPECTIVES
Syphilis continues to be a significant public health issue worldwide, reflecting ongoing transmission trends and shifting epidemiological profiles. The notable global resurgence over the last decade has exposed deficiencies in current control programs and emphasizes the urgent need to revisit and strengthen prevention strategies [
9]. Particularly, the marked rise in early latent and asymptomatic infections, driven by evolving sexual practices, increased partner concurrency, and the widespread adoption of dating apps, has fueled persistent disease spread—often evading traditional surveillance efforts [
23]. The recent adoption of universal notification in Korea has significantly enhanced case identification and improved the precision of epidemiologic data, yet it has also exposed a greater disease burden that was previously unrecognized when relying on sentinel surveillance alone [
11,
12].
In the domain of public health, prompt diagnosis, partner notification, and focused screening among high-risk groups represent essential elements for effective syphilis management. Routine screening practices targeting MSM, those with multiple sexual partners, and individuals living with HIV have demonstrated substantial benefits in curbing transmission and ensuring timely intervention [
24]. Incorporating syphilis screening into standard sexual health protocols, notably within HIV pre-exposure prophylaxis settings and urology outpatient facilities, can significantly broaden diagnostic efforts [
25]. Providing education about safe sexual behaviors, alongside accessible screening and treatment options, is vital—particularly for adolescent and young adult populations, among whom infection incidence is escalating.
Addressing the intersection of syphilis with other public health issues necessitates coordinated, multidisciplinary strategies. Coinfection can accelerate disease progression, modify serological responses, and complicate therapeutic outcomes [
5]. Integrating syphilis surveillance and management into broader STI and HIV programs enhances patient care and promotes efficient utilization of health system resources. Moreover, advances in molecular epidemiology and genomic surveillance can facilitate the identification of transmission clusters, thereby supporting more targeted public health actions [
26].
Looking forward, novel approaches will be essential to address future syphilis control challenges. These involve the use of digital contact tracing technologies, artificial intelligence-enabled risk assessment models, and innovative diagnostic tools capable of providing rapid, point-of-care detection of treponemal infection. Additionally, ongoing vaccine research, though promising, continues to face major biological obstacles [
27]. The development of a syphilis vaccine has been hampered by
T. pallidum’s extremely limited surface antigen expression, antigenic variation, and its unique ability to evade both innate and adaptive immune responses, which together complicate the induction of durable protective immunity [
28,
29]. Despite these challenges, continued progress in molecular immunology and antigen discovery may eventually provide new avenues for preventive strategies. For clinicians, including urologists, maintaining heightened clinical suspicion and reinforcing collaboration with public health authorities will be critical for addressing the sustained resurgence of syphilis and averting its associated complications.
CONCLUSIONS
Syphilis continues to represent a significant global and national public health challenge, with its resurgence reflecting evolving sexual behaviors and the shortcomings of current preventive measures. In Korea, universal disease surveillance has exposed a previously underestimated burden of syphilis, emphasizing the importance of ongoing monitoring and prompt intervention. Within urological practice, syphilis may present as a variety of genitourinary conditions, necessitating clinical vigilance, comprehensive sexual history assessment, and appropriate serological evaluation for correct diagnosis. Timely administration of antimicrobials, notification of partners, and focused screening among high-risk groups are crucial for effective management. Future advancements in diagnostic methods, digital contact tracing, and vaccine development have the potential to enhance disease control efforts. Continued cooperation between healthcare providers and public health authorities is fundamental to reversing the rising trend of syphilis and mitigating its effects on individual and public health.
NOTES
-
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
-
Conflict of Interest
The authors have nothing to disclose.
-
Author Contribution
Conceptualization: SJL, JBC; Visualization: JBC; Writing - original draft: JBC; Writing - review & editing: SJL, JBC.
Fig. 1.Trends in reported early-stage syphilis during the sentinel surveillance period (2020–2023) and after the nationwide transition to universal surveillance in 2024. Data from the Korea Disease Control and Prevention Agency. Total reported cases in 2024 (approximately 2,800), including tertiary, early latent, and congenital syphilis, exceed the primary and secondary syphilis cases shown in this graph.
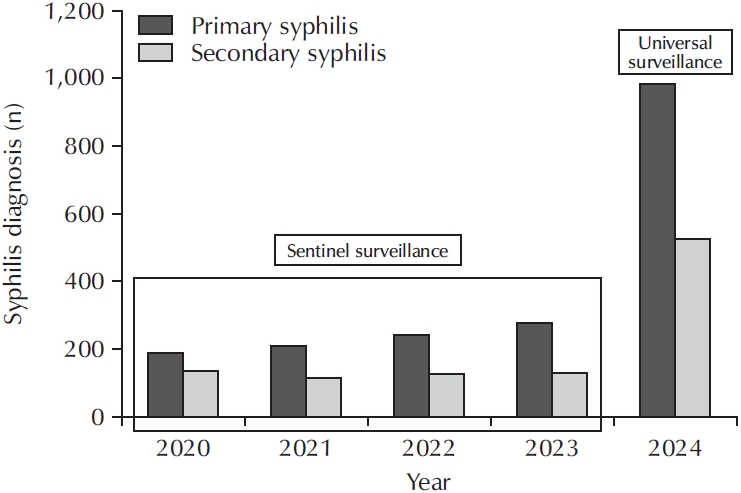
Table 1.Clinical manifestations of syphilis relevant to urological practice
|
Stage of syphilis |
Typical clinical features |
Urological manifestations |
Differential diagnoses |
|
Primary |
Single, painless chancre at the inoculation site accompanied by regional lymphadenopathy |
Ulceration affecting genital or perineal regions (including glans, foreskin, scrotum, urethral meatus, perineum, or rectum); typically presents with painless inguinal lymph nodes |
Genital herpes, chancroid, traumatic ulcer, Behçet's disease |
|
Secondary |
Widespread rash, fever, malaise, generalized lymphadenopathy, mucocutaneous lesions (condylomata lata) |
Broad-based, moist condyloma lata in the perineal or perianal area; possible urethral discharge, dysuria, or perineal pain; may also manifest as syphilitic balanitis |
HPV-related condyloma, candidiasis, nongonococcal urethritis, prostatitis |
|
Latent |
No clinical symptoms but positive serological findings |
Predominantly asymptomatic; may manifest as unexplained positive serology |
Other latent STIs, false-positive serology |
|
Tertiary |
Cardiovascular syphilis, gummatous involvement, neurosyphilis |
Sexual dysfunction (erectile dysfunction, reduced libido), LUTS secondary to neurogenic bladder or vascular compromise |
Diabetes-associated ED, atherosclerotic ED, idiopathic LUTS, neurogenic bladder from different etiologies |
Table 2.Recommended treatment regimens for adult syphilis
|
Stage/condition |
Recommended regimen |
Alternative regimen (penicillin allergy) |
Notes |
|
Primary, secondary, or early latent (<1 year) |
Benzathine penicillin G 2.4 million units IM as a single dose |
Doxycycline 100 mg orally twice daily for 14 days, or ceftriaxone 1–2 g IV/IM daily for 10–14 days*
|
High rates of cure; assess serologic response at 6, 12, and 24 months |
|
Late latent (≥1 year) or of unknown duration |
Benzathine penicillin G 2.4 million units IM once weekly for 3 weeks |
Doxycycline 100 mg orally twice daily for 28 days, or ceftriaxone 1–2 g IV/IM daily for 10–14 days*
|
Serologic response may be slower; monitor titers on a regular basis |
|
Neurosyphilis, ocular syphilis, and otosyphilis |
Administer aqueous crystalline penicillin G 18–24 million units/day IV (3–4 million units every 4 hours) for 10–14 days |
Ceftriaxone 1–2 g IV/IM daily for 10–14 days*
|
Re-examination of CSF may be indicated; desensitization is preferred during pregnancy |
|
Pregnancy |
Use benzathine penicillin G as previously described |
Desensitization followed by penicillin administration |
Penicillin is the only agent effective in preventing congenital syphilis |
REFERENCES
- 1. Peeling RW, Mabey D, Chen XS, Garcia PJ. Syphilis. Lancet 2023;402:336-46.ArticlePubMed
- 2. Peeling RW, Mabey D, Fitzgerald DW, Watson-Jones D. Avoiding HIV and dying of syphilis. Lancet 2004;364:1561-3.ArticlePubMed
- 3. Stamm LV. Syphilis: Re-emergence of an old foe. Microb Cell 2016;3:363-70.ArticlePubMedPMC
- 4. Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med 2020;382:845-54.ArticlePubMed
- 5. Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin Infect Dis 2007;44:1222-8.ArticlePubMed
- 6. Rowley J, Vander Hoorn S, Korenromp E, Low N, Unemo M, Abu-Raddad LJ, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ 2019;97:548-62.ArticlePubMedPMC
- 7. Goh BT. Syphilis in adults. Sex Transm Infect 2005;81:448-52.ArticlePubMedPMC
- 8. French P. Syphilis. BMJ 2007;334:143-7.ArticlePubMedPMC
- 9. Rosset F, Celoria V, Delmonte S, Mastorino L, Sciamarrelli N, Boskovic S, et al. The epidemiology of syphilis worldwide in the last decade. J Clin Med 2025;14:5308.ArticlePubMedPMC
- 10. Komori A, Mori H, Xie W, Valenti S, Naito T. Rapid resurgence of syphilis in Japan after the COVID-19 pandemic: a descriptive study. PLoS One 2024;19:e0298288.ArticlePubMedPMC
- 11. Kim E, Han S, Yu J. Epidemiological characteristics of syphilis in the Republic of Korea in 2024. Public Health Wkly Rep 2025;18:1343-59.
- 12. Lee SJ, Choi JB. A narrative review of syphilis notification systems in Korea: change to mandatory surveillance system. Urogenit Tract Infect 2025;20:28-33.ArticlePDF
- 13. Singh AE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microbiol Rev 1999;12:187-209.ArticlePubMedPMCPDF
- 14. Janier M, Unemo M, Dupin N, Tiplica GS, Potočnik M, Patel R. 2020 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol 2021;35:574-88.ArticlePubMedPDF
- 15. Vezzoni R, Colli C, Rebez G, Trombetta C, Boltar A, Zalaudek I, et al. Syphilitic balanitis of follmann: can dermoscopy be useful tool in the differential diagnosis? Dermatol Pract Concept 2022;12:e2022022.ArticlePubMedPMC
- 16. Kim JW, Chae JY, Kim JW, Yoon CY, Oh MM, Kim JJ, et al. Stuttering priapism in a patient with neurosyphilis. World J Mens Health 2013;31:76-8.ArticlePubMedPMC
- 17. Skalnaya A, Fominykh V, Ivashchenko R, Averchenkov D, Grazhdantseva L, Frigo N, et al. Neurosyphilis in the modern era: literature review and case series. J Clin Neurosci 2019;69:67-73.ArticlePubMed
- 18. Zhou J, Zhang H, Tang K, Liu R, Li J. An updated review of recent advances in neurosyphilis. Front Med (Lausanne) 2022;9:800383.ArticlePubMedPMC
- 19. Sobhan T, Rowe HM, Ryan WG, Munoz C. Unusual case report: three cases of psychiatric manifestations of neurosyphilis. Psychiatr Serv 2004;55:830-2.ArticlePubMed
- 20. Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 2021;70:1-187.Article
- 21. Seña AC, White BL, Sparling PF. Novel Treponema pallidum serologic tests: a paradigm shift in syphilis screening for the 21st century. Clin Infect Dis 2010;51:700-8.ArticlePubMed
- 22. WHO Guidelines Approved by the Guidelines Review Committee. WHO Guidelines for the Treatment of Treponema pallidum (Syphilis). Geneva (Switzerland): World Health Organization; 2016.
- 23. Peterman TA, Heffelfinger JD, Swint EB, Groseclose SL. The changing epidemiology of syphilis. Sex Transm Dis 2005;32(10 Suppl):S4-10.ArticlePubMed
- 24. Refugio ON, Klausner JD. Syphilis incidence in men who have sex with men with human immunodeficiency virus comorbidity and the importance of integrating sexually transmitted infection prevention into HIV care. Expert Rev Anti Infect Ther 2018;16:321-31.ArticlePubMedPMC
- 25. Jarolimova J, Yan J, Govere S, Shezi S, Ngcobo LM, Sagar S, et al. Sexually transmitted infection testing integrated with HIV prevention and contraceptive services in hair salons in urban South Africa. J Acquir Immune Defic Syndr 2025;99:359-67.ArticlePubMedPMC
- 26. Beale MA, Marks M, Sahi SK, Tantalo LC, Nori AV, French P, et al. Genomic epidemiology of syphilis reveals independent emergence of macrolide resistance across multiple circulating lineages. Nat Commun 2019;10:3255.ArticlePubMedPMCPDF
- 27. Waugh S, Cameron CE. Syphilis vaccine development: aligning vaccine design with manufacturing requirements. Hum Vaccin Immunother 2024;20:2399915.ArticlePubMedPMC
- 28. Ávila-Nieto C; Pedreño-López N, Mitjà O, Clotet B, Blanco J, Carrillo J. Syphilis vaccine: challenges, controversies and opportunities. Front Immunol 2023;14:1126170.ArticlePubMedPMC
- 29. Cameron CE, Lukehart SA. Current status of syphilis vaccine development: need, challenges, prospects. Vaccine 2014;32:1602-9.ArticlePubMed
 , Jin Bong Choi2
, Jin Bong Choi2


 KAUTII
KAUTII
 ePub Link
ePub Link Cite
Cite

