Search
- Page Path
- HOME > Search
Review Article
- Asymptomatic Bacteriuria in Older Adults – Diagnosis, Management, and Future Directions: A Narrative Review
- Ki Hong Kim, Hee Jo Yang
- Urogenit Tract Infect 2025;20(2):58-66. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550002001
-
 Abstract
Abstract
 PDF
PDF PubReader
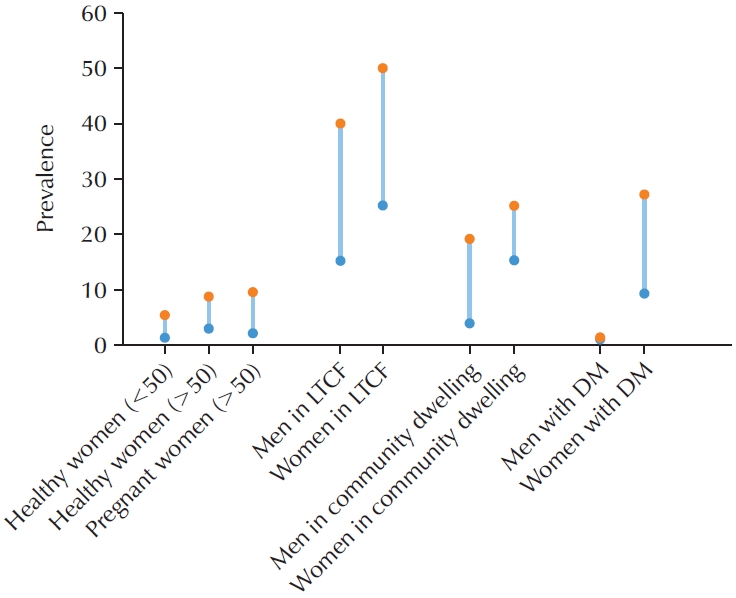
PubReader - Asymptomatic bacteriuria (ASB) is defined as the presence of bacteria in the urine in the absence of urinary tract infection (UTI) symptoms. The prevalence of ASB increases with advancing age, particularly among older patients with underlying health conditions. ASB is especially common among residents of long-term care facilities; however, distinguishing ASB from symptomatic UTI in this population remains a significant clinical challenge. The frequent occurrence of ASB often results in unnecessary antibiotic administration, thereby contributing to the development of antibiotic resistance. Current clinical guidelines recommend screening for and treating ASB only in certain circumstances, such as prior to urological procedures or in pregnant women. There is a pressing need for improved diagnostic approaches to differentiate ASB more accurately from UTI, particularly in older adults. Reducing unnecessary urine testing and inappropriate antibiotic use may help prevent over-treatment and minimize associated risks, including Clostridium difficile infection and increased antimicrobial resistance.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 11,540 View
- 116 Download
- 1 Crossref

Original Articles
- Efficacy of Urovaxom for Improving Chronic Pelvic Pain Syndrome Symptoms in Prostate Cancer Patients Who Underwent Radical Prostatectomy: A Multicenter, Prospective Cohort Study
- Jun-Koo Kang, Yun-Sok Ha, Sungchan Park, Tae Gyun Kwon, Tae-Hwan Kim
- Urogenit Tract Infect 2025;20(1):42-47. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550014007
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
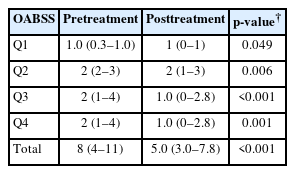
Chronic pelvic pain syndrome (CPPS) is a multifactorial condition that can significantly diminish quality of life. Although some patients have reported persistent pelvic pain after radical prostatectomy (RP), the prevalence and direct causal relationship between CPPS and RP remain unclear. This multicenter prospective study aimed to evaluate the efficacy of Urovaxom for improving CPPS symptoms. Materials and Methods: A total of 52 prostate cancer patients who underwent RP were enrolled and administered Urovaxom (60 mg/day) for 12 weeks. Changes in National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI), overactive bladder symptom score (OABSS), International Prostate Symptom Score (IPSS), and inflammation markers (white blood cell [WBC], C-reactive protein [CRP]) were analyzed using the Wilcoxon signed-rank test.
Results
After 12 weeks of treatment, the NIH-CPSI total score significantly decreased from 19 (interquartile range [IQR], 16–23) to 12.5 (IQR, 8.0–16.8) (p<0.001). The OABSS total score decreased from 8 (IQR, 4–11) to 5 (IQR, 3.0–7.8), and the IPSS total score decreased from 13.5 (IQR, 10.0–22.8) to 10.5 (IQR, 5.0–17.0) (p<0.001). WBC levels showed a slight increase (p=0.028), but the clinical relevance of this change is uncertain and warrants further investigation. CRP changes were not statistically significant (p=0.274).
Conclusions
Urovaxom demonstrated significant efficacy in improving CPPS symptoms, particularly pain and reduced quality of life, in patients following RP. These findings suggest Urovaxom as a potential therapeutic option for CPPS after management using RP. -
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Addressing an Unmet Need in Postprostatectomy Care: Perspectives on Urovaxom
Byeong Jin Kang
Urogenital Tract Infection.2025; 20(2): 118. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,155 View
- 44 Download
- 2 Crossref

- Trends in Age-Specific Prevalence of Lower Urinary Tract Dysfunction: A Nationwide Population-Based Cohort Study
- Young Hwan Kim, Se Hwa Hong, Tae Wook Kang, Hyun Chul Chung, Tae Hyoung Kim, Sae Chul Kim, Sang Baek Koh, Jae Hung Jung
- Urogenit Tract Infect 2023;18(3):101-106. Published online December 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.3.101
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
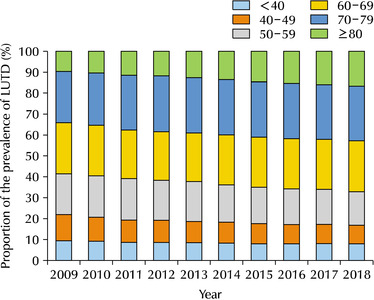
ePub - Purpose: To elucidate the longitudinal changes in the prevalence of lower urinary tract dysfunction (LUTD) according to age over the past 10 years.
Materials and Methods: The changes in the proportion of prevalence for LUTD, including benign prostatic hyperplasia (BPH) and urinary incontinence (UI) among South Koreans from 2009 to 2018, were analyzed using the National Health Information Database established by the Korean National Health Insurance Service. All conditions were defined according to the corresponding Korean Standard Classification of Diseases-8 for diagnosis and surgical procedures and Health Insurance Review & Assessment Service codes for drugs.
Results: The 60-69, 70-79, and over 80 age groups accounted for more than 60% of the LUTD cases from 2009 to 2018, while significant increases in the crude prevalence of LUTD were observed over a 10-year period in all age groups (p for trend <0.05). In age groups over 60 years, LUTD was more prevalent in men than women, but there was no statistically significant difference in proportion (p>0.05). The changes in the prevalence and prevalence proportion exhibited similar trends in BPH, UI, and LUTD.
Conclusions: LUTD was more prevalent in the elderly aged over 60 years old than in younger adults. Therefore, this study suggests the development of nationwide healthcare policies to manage LUTD in the elderly population of South Korea, which is expected to become the world’s most aged population. -
Citations
Citations to this article as recorded by- Nursing strategies for managing urological disorders in aging populations: a comprehensive review
Hong Liu, Jie Wu
BMC Urology.2026;[Epub] CrossRef
- Nursing strategies for managing urological disorders in aging populations: a comprehensive review
- 4,559 View
- 21 Download
- 1 Crossref

- The Feasibility of Radical Prostatectomy for Medication Refractory Chronic Prostatitis/Chronic Pelvic Pain Syndrome
- Seung Chan Jeong
- Urogenit Tract Infect 2022;17(3):76-80. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.76
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: The purpose of this study was to compare the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) scores of patients with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) given pharmacological treatment with those who additionally had prostate cancer and underwent surgical treatment.
Materials and Methods: From January 2000 to March 2021, a total of 7,650 patients were diagnosed with chronic prostatitis (N41.1) at our hospital, of which 234 patients were additionally diagnosed with prostate cancer. After excluding patients with severe benign prostatic hyperplasia (>100 g)-related lower urinary tract symptoms or neurological and psychiatric abnormalities, or advanced prostate cancer, 52 patients undergoing pharmacological treatment with a combination of drugs and 20 patients who underwent radical prostatectomy due to additional prostate cancer were included in the analysis. The NIH-CPSI scores of the two groups were compared at the first outpatient visit, 3 months, and 6 months after the first visit. The p-values were calculated using the Mann-Whitney U test, and the Wilcoxon signed rank test.
Results: Patients who underwent radical prostatectomy for prostate cancer showed significant reductions in the voiding and quality of life scores in the NIH-CPSI, but not the pain score at 3 months. After 6 months, there was a significant decrease in the overall NIH-CPSI. On the other hand, in the group on pharmacological therapy, the decrease was statistically significant only in the voiding score at 6 months. However, in the surgery group, 3 patients were found to be suffering from urinary incontinence, and 7 patients from erectile dysfunction.
Conclusions: Radical prostatectomy, therefore, appears to be a promising treatment that can be carefully considered for patients with refractory CP/CPPS who do not receive adequate treatment and thus have a poor quality of life.
- 3,088 View
- 9 Download

Review
- Comprehensive Review of COVID-19 on Benign Prostate Hyperplasia Patient Symptoms
- Joongwon Choi, Hong Jin Suh, Dong Hwan Lee, Tae-Kon Hwang, Jung Jun Kim
- Urogenit Tract Infect 2022;17(2):31-35. Published online August 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.2.31
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Since the outbreak of the global Coronavirus disease (COVID-19) pandemic in 2019, the number of confirmed cases has increased steadily worldwide. The most common symptom of COVID-19 (SARS-CoV-2) is respiratory symptoms. On the other hand, increased voiding frequency and lower urinary tract symptoms (LUTS) have also been reported. Regarding the relationship between LUTS and COVID-19, only small size (n<100) retrospective studies have been reported, but the post-International Prostate Symptom Score (IPSS) increases compared to pre-IPSS after a COVID-19 infection in those older than 50 years. α-blockers and phosphodiesterase-5 inhibitors are relatively safe, but there are conflicting reports on 5α-reductase inhibitors; hence, further research is needed. Four major theories have been argued regarding the relationship between LUTS and COVID-19: renin-angiotensin system-related, androgen-related, inflammation-related, and metabolic derangement-related. In conclusion, elderly male patients often have benign prostate hyperplasia as a co-morbidity, and the severity of COVID-19 is high in this group. Therefore, voiding symptoms in these patient groups is of particular concern.
- 2,213 View
- 8 Download


 KAUTII
KAUTII

 First
First Prev
Prev


