Search
- Page Path
- HOME > Search
Original Article
- Efficacy of Urovaxom for Improving Chronic Pelvic Pain Syndrome Symptoms in Prostate Cancer Patients Who Underwent Radical Prostatectomy: A Multicenter, Prospective Cohort Study
- Jun-Koo Kang, Yun-Sok Ha, Sungchan Park, Tae Gyun Kwon, Tae-Hwan Kim
- Urogenit Tract Infect 2025;20(1):42-47. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550014007
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
Chronic pelvic pain syndrome (CPPS) is a multifactorial condition that can significantly diminish quality of life. Although some patients have reported persistent pelvic pain after radical prostatectomy (RP), the prevalence and direct causal relationship between CPPS and RP remain unclear. This multicenter prospective study aimed to evaluate the efficacy of Urovaxom for improving CPPS symptoms. Materials and Methods: A total of 52 prostate cancer patients who underwent RP were enrolled and administered Urovaxom (60 mg/day) for 12 weeks. Changes in National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI), overactive bladder symptom score (OABSS), International Prostate Symptom Score (IPSS), and inflammation markers (white blood cell [WBC], C-reactive protein [CRP]) were analyzed using the Wilcoxon signed-rank test.
Results
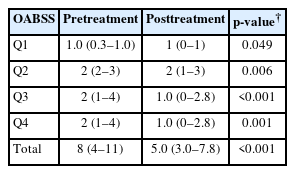
After 12 weeks of treatment, the NIH-CPSI total score significantly decreased from 19 (interquartile range [IQR], 16–23) to 12.5 (IQR, 8.0–16.8) (p<0.001). The OABSS total score decreased from 8 (IQR, 4–11) to 5 (IQR, 3.0–7.8), and the IPSS total score decreased from 13.5 (IQR, 10.0–22.8) to 10.5 (IQR, 5.0–17.0) (p<0.001). WBC levels showed a slight increase (p=0.028), but the clinical relevance of this change is uncertain and warrants further investigation. CRP changes were not statistically significant (p=0.274).
Conclusions
Urovaxom demonstrated significant efficacy in improving CPPS symptoms, particularly pain and reduced quality of life, in patients following RP. These findings suggest Urovaxom as a potential therapeutic option for CPPS after management using RP. -
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Addressing an Unmet Need in Postprostatectomy Care: Perspectives on Urovaxom
Byeong Jin Kang
Urogenital Tract Infection.2025; 20(2): 118. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,154 View
- 44 Download
- 2 Crossref

Case Report
- Case of Fournier’s Gangrene in a Patient with Long-Term Indwelling Catheterization due to Urinary Incontinence after Open Radical Prostatectomy
- Kyung Kgi Park, Sung Dae Kim, Young-Joo Kim, Jung-Sik Huh
- Urogenit Tract Infect 2020;15(1):6-9. Published online April 30, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.1.6
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Fournier’s gangrene is a life-threatening disease that needs to be treated as soon as possible. An 82-year-old male, who exchanged a urethral catheter once a month for urinary incontinence management after open radical prostatectomy, presented with an acute onset of mental change and general weakness. After ten days’ hospitalization, the disease was diagnosed. The scrotal wall was opened, and the infectious tissue was exposed to the air and kept open with an aseptic dressing. After 45 days, his scrotal wound healed and returned to its typical appearance without scarring and wound disruption. He recovered fully from the infection. This paper reports a case of Fournier’s gangrene in a patient with long-term indwelling catheterization due to urinary incontinence after an open radical prostatectomy with a literature review.
- 1,788 View
- 1 Download


 KAUTII
KAUTII

 First
First Prev
Prev


