Search
- Page Path
- HOME > Search
Review Article
- Asymptomatic Bacteriuria in Older Adults – Diagnosis, Management, and Future Directions: A Narrative Review
- Ki Hong Kim, Hee Jo Yang
- Urogenit Tract Infect 2025;20(2):58-66. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550002001
-
 Abstract
Abstract
 PDF
PDF PubReader
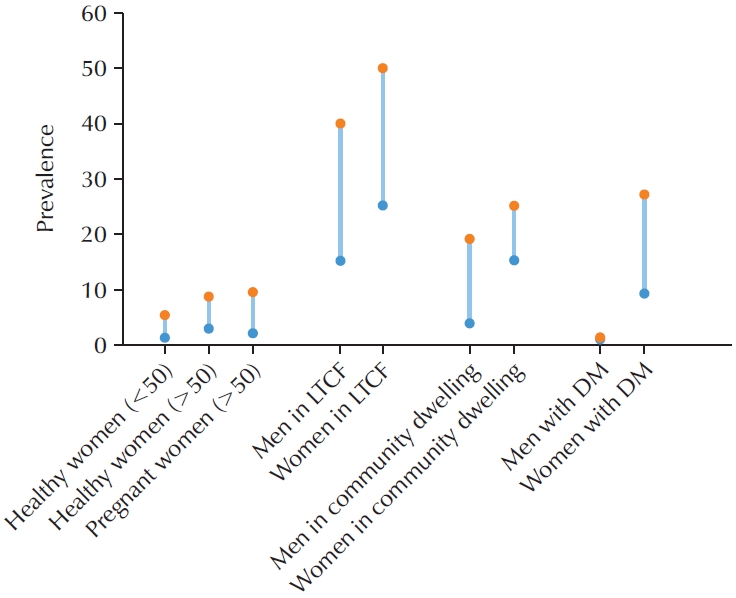
PubReader - Asymptomatic bacteriuria (ASB) is defined as the presence of bacteria in the urine in the absence of urinary tract infection (UTI) symptoms. The prevalence of ASB increases with advancing age, particularly among older patients with underlying health conditions. ASB is especially common among residents of long-term care facilities; however, distinguishing ASB from symptomatic UTI in this population remains a significant clinical challenge. The frequent occurrence of ASB often results in unnecessary antibiotic administration, thereby contributing to the development of antibiotic resistance. Current clinical guidelines recommend screening for and treating ASB only in certain circumstances, such as prior to urological procedures or in pregnant women. There is a pressing need for improved diagnostic approaches to differentiate ASB more accurately from UTI, particularly in older adults. Reducing unnecessary urine testing and inappropriate antibiotic use may help prevent over-treatment and minimize associated risks, including Clostridium difficile infection and increased antimicrobial resistance.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 11,529 View
- 116 Download
- 1 Crossref

Original Articles
- Predictor for Ureteral Stent Removal in Gynecological Cancer Patients with a Ureteral Obstruction
- Sung Hyun Ji, Young Kwon Hong, Young Dong Yu, Seung-Ryeol Lee
- Urogenit Tract Infect 2022;17(3):103-109. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.103
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study investigated the possibility of ureteral stent removal in patients with gynecological cancer and ureteral obstruction.
Materials and Methods: From February 2010 to March 2022, the records of 121 patients with gynecological cancer and ureteral obstruction undergoing periodic ureteral stent replacement were reviewed retrospectively. Ureteral stent removal was attempted in patients who showed improvement in hydronephrosis on abdominal computed tomography (CT) after ureteral stent insertion and who lost symptoms. Success was defined as not having to reinsert the stent because there were no uncomfortable symptoms. The following were evaluated as predictors for ureteral stent removal: pre-removal serum creatinine, hypertension, diabetes, asymptomatic bacteriuria, type of gynecologic malignancy, prior radiotherapy, hydronephrosis laterality, obstruction level, hydronephrosis etiology, ureteral stent size, and ureteral stent duration. The hydronephrosis changes on abdominal CT were also evaluated.
Results: Among 121 patients, 74 with 81 obstructed ureters were evaluated. Of the 81 ureters, successful removal occurred in 30 (37.0%). There were significant differences between the success and failure cases regarding asymptomatic bacteriuria, prior radiotherapy, and hydronephrosis etiology. Logistic regression analysis showed that asymptomatic bacteriuria and hydronephrosis etiology were significant predictors of ureteral stent removal (p<0.05). There were also significant differences in the hydronephrosis changes depending on asymptomatic bacteriuria and hydronephrosis etiology (p<0.05).
Conclusions: In patients with gynecological cancer who have a ureteral stent in place due to ureteral obstruction, ureteral stent removal may be considered in patients who do not have asymptomatic bacteriuria or other etiologies, such as external ureteral pressure or ureteral cancer metastasis.
- 2,653 View
- 3 Download

- Rates and Risk Factors of Bacteriuria in Patients with Bladder Cancer Who Underwent Treatment with Bacillus Calmette-Guérin
- Seong Jong Eun, Myung Soo Kim, Seung Il Jung, Hyun-Jung Choi, Ho Seok Chung, Eu Chang Hwang, Dong Deuk Kwon
- Urogenit Tract Infect 2020;15(2):47-53. Published online August 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.2.47
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study evaluated the rate and predictors of bacteriuria in patients who underwent transurethral resection of bladder tumor (TURBT) and Bacillus Calmette-Guérin (BCG) treatment.
Materials and Methods: We prospectively evaluated 266 patients who underwent TURBT and intravesical BCG treatment between January 2017 and September 2019. Urinalysis and urine culture were performed at the baseline, one to two weeks after TURBT and weekly during the BCG treatment period. The primary outcomes were the bacteriuria rates in BCG-treated patients, while the secondary outcomes were the risk factors of bacteriuria during BCG treatments.
Results: Of the 266 patients, the rate of bacteriuria was 4.5% before TURBT, 5.3% in the postoperative period, and 24.4% in the BCG treatment period. After BCG instillation, urinalysis showed that 204 and 38 patients tested positive for pyuria and nitrite, respectively. Multivariate analysis indicated that the risk factors associated with bacteriuria during BCG treatment included age (odds ratio [OR]: 1.06; p=0.003), sex (female) (OR, 5.41; p=0.007), diabetes mellitus (DM) (OR, 2.82; p=0.023), postoperative bacteriuria (OR, 8.08; p=0.032), bacterial counts>100/µl in urine flow cytometry (OR, 29.72; p<0.001), and positive urine nitrite test (OR, 6.20; p=0.001) at the time of positive urine culture sampling.
Conclusions: Approximately 25% of the patients suffered from bacteriuria during intravesical BCG treatment. Old age, female sex, DM, and postoperative bacteriuria were found to be the risk factors of bacteriuria during BCG treatment. Predictive factors could aid in clinical decisions during BCG treatments as well as decisions on BCG discontinuation. -
Citations
Citations to this article as recorded by- Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
Ali Bourgi, Omar Ghanem, Camille Brocail, Franck Bruyère
Surgical Infections.2025; 26(6): 390. CrossRef - MESANE KANSERİ ve ÜRİNER STOMASI OLAN HASTANIN EVDE BAKIMI
Neşe İşcan Ayyıldız
Paramedik ve Acil Sağlık Hizmetleri Dergisi.2024; 5(1): 31. CrossRef - Mesane Kanserinde İntravezikal Bacille Calmette- Guerin (BCG) Uygulaması ve Hemşirenin Sorumlulukları
Ayla YAVUZ KARAMANOĞLU, Ali Ersin ZÜMRÜTBAŞ
Adnan Menderes Üniversitesi Sağlık Bilimleri Fakültesi Dergisi.2023; 7(1): 256. CrossRef
- Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
- 3,997 View
- 13 Download
- 3 Crossref

- Performance of the Sysmex UF-1000i System in Screening for Significant Bacteriuria in Patients with Bladder Cancer Who Received Bacillus Calmette-Guérin Treatment
- Tae Hee Kim, Seung Il Jung, Myung Soo Kim, Hyun-Jung Choi, Ho Seok Chung, Eu Chang Hwang, Dong Deuk Kwon
- Urogenit Tract Infect 2020;15(2):38-46. Published online August 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.2.38
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: Diagnosing urinary tract infections by urine culture is time-consuming during a Bacillus Calmette-Guérin treatment. Because the urine culture results take time to collect, patients are treated presumptively, or Bacillus Calmette-Guérin is discontinued before the results. This study evaluated the ability of the Sysmex UF-1000i system to examine the urine bacterial count and determine if it could be used to predict a positive culture.
Materials and Methods: 180 patients who underwent transurethral resection for bladder tumors and received intravesical Bacillus Calmette-Guérin treatment between January 2017 and July 2018 were evaluated prospectively. For patients who received an intravesical Bacillus Calmette-Guérin treatment, urine flow cytometry, and urine cultures were assessed weekly during the treatment period.
Results: During Bacillus Calmette-Guérin instillation, 44, 146, and 27 patients had bacteriuria, pyuria, and positive urine nitrite, respectively. Multivariate analysis indicated that the predictors associated with bacteriuria included the urine flow cytometry results of >100 bacteria/µl (odds ratio, 22.73; p<0.001) and positive urine nitrite (odds ratio, 5.67; p=0.012) at the time of sampling for positive urine culture. The area under the receiver operative characteristic curve for diagnosing bacteriuria by urine flow cytometry was 0.825. A urine flow cytometry cutoff value of >100 bacteria/µl resulted in a sensitivity and specificity of 75% and 90.91%, respectively. Using the cutoff of >1,000 bacteria/µl, the sensitivity and specificity were 50% and 94.85%, respectively.
Conclusions: Rapid urinary tract infection diagnosis using Sysmex UF-1000i can be used to determine whether to treat an infection and to avoid unnecessary Bacillus Calmette-Guérin discontinuation and urine culture tests. -
Citations
Citations to this article as recorded by- Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
Ali Bourgi, Omar Ghanem, Camille Brocail, Franck Bruyère
Surgical Infections.2025; 26(6): 390. CrossRef
- Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
- 2,073 View
- 2 Download
- 1 Crossref


 KAUTII
KAUTII

 First
First Prev
Prev


