Search
- Page Path
- HOME > Search
Review Articles
- Molecular Mechanisms of Antibiotic Resistance in Uropathogenic Escherichia coli: A Narrative Review
- Nakjun Choi, Dong Uk Kim, Eun-Jin Lee
- Urogenit Tract Infect 2025;20(2):96-106. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550018009
-
 Abstract
Abstract
 PDF
PDF PubReader
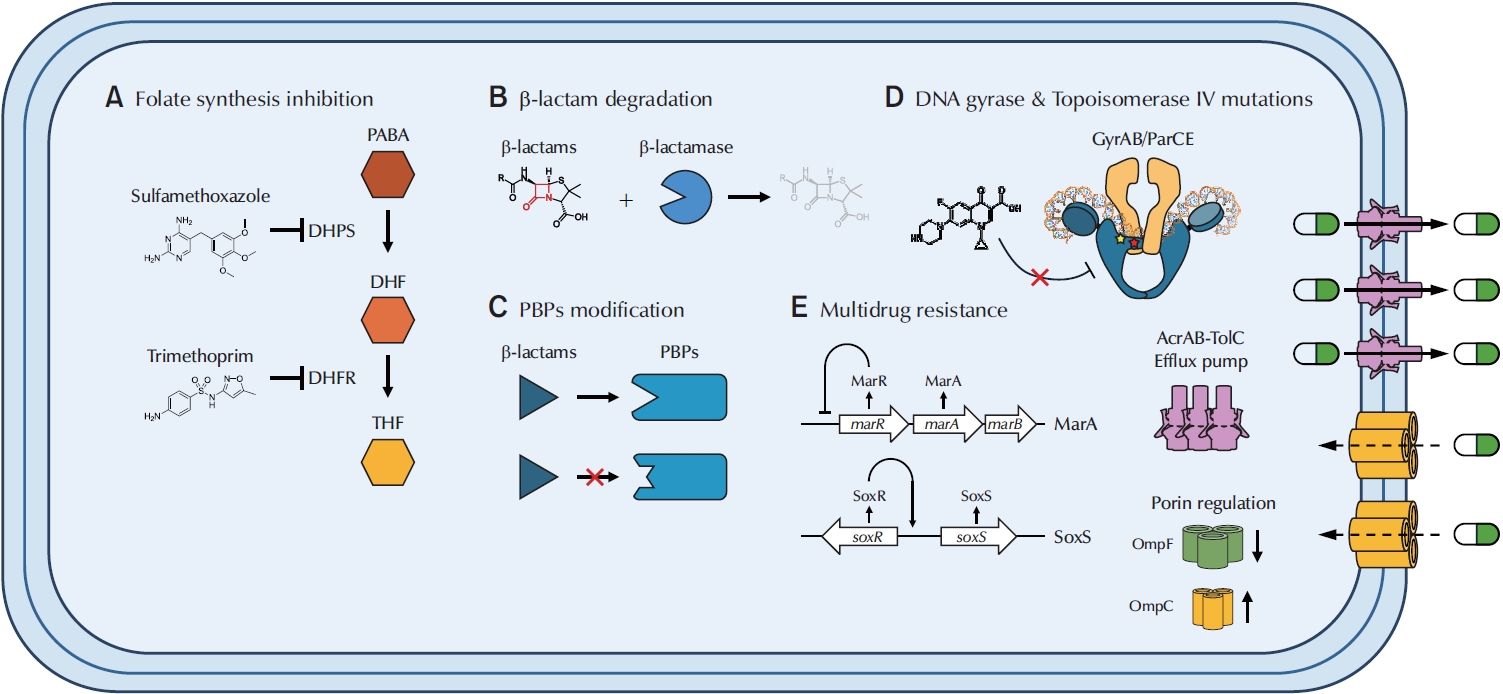
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections worldwide, with uropathogenic Escherichia coli (UPEC) serving as the primary causative agent. Although antibiotic therapy remains the standard of care for UTI treatment, the increasing prevalence of antimicrobial resistance has substantially reduced the effectiveness of commonly prescribed antibiotics. Resistance to trimethoprim-sulfamethoxazole (TMP-SMX), β-lactams, and fluoroquinolones is particularly concerning, as these agents constitute the principal therapeutic options for UTIs. This review examines the molecular mechanisms underlying UPEC resistance to these three classes of antibiotics, including target site modifications, efflux pump overexpression, porin regulation, and enzymatic degradation. Furthermore, it explores how these resistance determinants contribute to the development of multidrug-resistant (MDR) UPEC strains, which demonstrate cross-resistance to multiple antibiotics and present significant challenges for clinical management. Novel therapeutic strategies, such as efflux pump inhibitors, bacteriophage therapy, and genomic-guided precision medicine, are under investigation as potential solutions to address the growing global burden of MDR UPEC, alongside alternative non-antibiotic treatments. This review aims to provide a comprehensive overview of the genetic and regulatory pathways driving antibiotic resistance in UPEC, offering insights that may guide the development of effective treatment strategies and help mitigate the ongoing spread of antimicrobial resistance.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,264 View
- 87 Download
- 1 Crossref

- Beta-Lactamase-Mediated Antibiotic Resistance in Urinary Tract Infections: Mechanisms and Therapeutic Strategies
- Fanglin Shao, Dengxiong Li, Jie Wang, Zhouting Tuo, Zhipeng Wang, Wuran Wei, Ruicheng Wu, Dechao Feng
- Urogenit Tract Infect 2025;20(2):67-81. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550012006
-
 Abstract
Abstract
 PDF
PDF PubReader
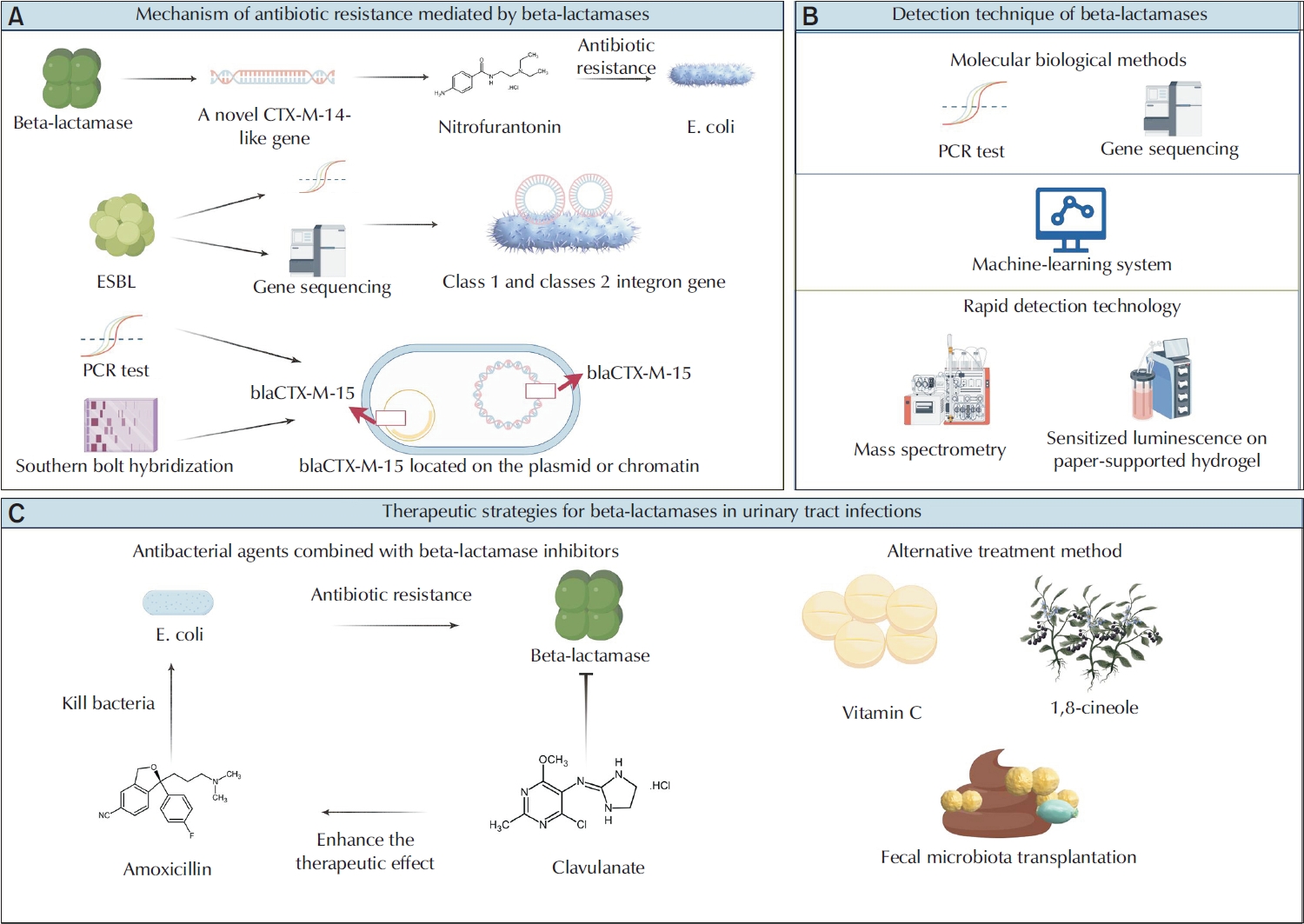
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections globally, and are primarily caused by Escherichia and Klebsiella. The overprescription and inappropriate use of antibiotics have accelerated the emergence of multidrug-resistant bacteria. Beta-lactamases play a critical role in mediating antibiotic resistance in UTIs. These enzymes promote bacterial resistance through multiple mechanisms, including gene mutation, plasmid-mediated horizontal gene transfer, and the involvement of integrons. Comprehensive knowledge of the ways in which beta-lactamases contribute to resistance in UTIs is essential for improving treatment strategies. Advances in detection technologies, such as gene sequencing and mass spectrometry, have greatly enhanced the ability to monitor and predict bacterial resistance. Current therapeutic strategies include the application of beta-lactamase inhibitors, the development of novel antibiotics, and alternative treatments that have shown efficacy against beta-lactamase-mediated antibiotic resistance. This paper reviews the mechanisms of beta-lactamase-mediated resistance in UTIs and provides an in-depth overview of several detection methods and therapeutic approaches.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,556 View
- 68 Download
- 1 Crossref

Original Articles
- Impact of Antibiotics on the Efficacy of Immune Checkpoint Inhibitors in Metastatic Urothelial Carcinoma
- Do Gyeong Lim, Ho Yeon Lee, Ho Seok Chung, Eu Chang Hwang, Seung Il Jung, Dong Deuk Kwon
- Urogenit Tract Infect 2023;18(3):75-81. Published online December 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.3.75
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
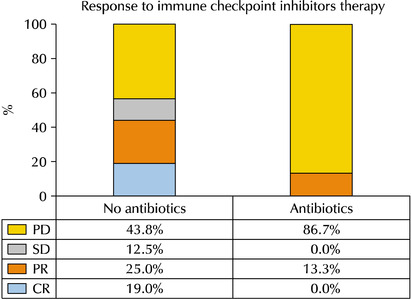
ePub - Purpose: Emerging evidence has suggested that prior or concurrent antibiotic (ATB) use may be associated with a poor response to immune checkpoint inhibitors (ICIs) in patients with some solid tumors. This study examined the effects of ATB use on the oncological outcomes of patients receiving ICIs for mUC.
Materials and Methods: Patients receiving ICIs for mUC between 2018 and 2020 were assessed retrospectively. Those with over three cycles of atezolizumab or pembrolizumab were included. ATB use, defined as ≥ three days within 60 days before or three months after ICI administration, was compared between groups for oncological outcomes.
Results: Thirty-one patients were examined. The ATB-use and no-ATB-use groups consisted of 15 (48.4%) and 16 patients (51.6%), respectively. The ATB-use group showed a lower disease control rate (56.3% vs. 13.3%, p=0.023) than the no-ATB-use group. The objective response rate in the ATB-use group was lower than the no-ATB-use group, but the difference was statistically insignificant (43.7% vs. 13.3%, p=0.113). The ATB-use group had shorter progression-free survival (median three vs. six months, log-rank p=0.045) and shorter overall survival (median three vs. 14 months, log-rank p=0.023) than the no-ATB-use group. The most commonly used antibiotics were fluoroquinolones (46.7%), cephalosporins (40.0%), non-cephalosporin beta-lactams (6.7%), and nitrofurantoin (6.7%).
Conclusions: ATB may be associated with poorer oncological outcomes in patients with mUC who received ICI therapy. Hence, further research will be needed to understand the relationship between the modulation of ATB-related dysbiosis and gut microbiota composition with the oncological outcomes in patients with mUC.
- 2,956 View
- 10 Download

- Fournier’s Gangrene: A 10-Year Clinical Experience at a Tertiary Academic Medical Center
- Woo Seop Seong, Byeong Jin Kang, A Reum Kim, Kyung Hwan Kim, Hong Koo Ha
- Urogenit Tract Infect 2023;18(2):64-69. Published online August 31, 2023
- DOI: https://doi.org/10.14777/uti.2023.18.2.64
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This retrospective study examined the factors influencing clinical outcomes and mortality in patients with Fournier's Gangrene (FG). The medical history, diagnostic procedures, treatment approaches, complications, and mortality factors associated with FG were analyzed.
Materials and Methods: This study retrospectively analyzed the medical records of 40 patients with FG treated over 10 years. The collected data included the patient demographics, comorbidities, vital signs, laboratory tests, Fournier’s Gangrene Severity Index (FGSI) scores, wound swab culture results, treatment approaches, and length of hospitalization.
Results: Among the patients with FG, diabetes mellitus and hypertension were the most common comorbidities. The hemodialysis dependence has been identified as a significant risk factor of mortality. In addition, septic shock and an FGSI >9 were associated with increased mortality. Escherichia coli was the most prevalent bacterium in wound swab cultures, and the presence of antibiotic-resistant bacteria was significantly higher in the non-survivors. Treatment involved broad-spectrum antibiotics, emergency surgical debridement, and subsequent adjustments based on culture results.
Conclusions: Early diagnosis and prompt initiation of treatment are essential for improving the outcomes of patients with FG. Hemodialysis dependency, septic shock, FGSI scores, and the presence of antibiotic-resistant bacteria are important factors associated with mortality in patients with FG. Further research will be needed to validate these findings and explore adjunctive therapies to enhance the patient outcomes and improve FG management. -
Citations
Citations to this article as recorded by- Prognostic factors and clinical outcomes in Fournier’s Gangrene: a retrospective study of 35 patients
Han Bee Hong, Jeong Woo Lee, Chan Hee Park
BMC Infectious Diseases.2024;[Epub] CrossRef
- Prognostic factors and clinical outcomes in Fournier’s Gangrene: a retrospective study of 35 patients
- 2,752 View
- 18 Download
- 1 Crossref

- Korean Multicenter Study of Infectious Complications after Transurethral Prostate Surgery in Patients with Preoperative Sterile Urine
- Seong Hyeon Yu, Seung Il Jung, Eu Chang Hwang, Tae-Hyoung Kim, Jae Duck Choi, Koo Han Yoo, Jeong Woo Lee, Dong Hoon Koh, Sangrak Bae, Seung Ok Yang, Joongwon Choi, Seung Ki Min, Hoon Choi
- Urogenit Tract Infect 2022;17(3):81-88. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.81
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: To evaluate the efficacy of antibiotic prophylaxis and determine the risk factors of infectious complications after transurethral surgery of the prostate.
Materials and Methods: Seven hundred and seventy-two patients who underwent transurethral resection of the prostate (TURP) or holmium laser enucleation of the prostate (HOLEP) were reviewed. Of these, this study enrolled 643 patients without bacteriuria who had not received antibiotics for urinary tract infections for two weeks before surgery. The patients were divided into two groups according to the duration of the antibiotics (Group 1: less than one day, n=396 vs. Group 2: more than one day, n=247).
Results: The overall incidence of postoperative infectious complications in 643 patients was 5.0% (32/643). When postoperative infectious complications were compared according to the duration of the antibiotics (Group 1 vs. Group 2), the infectious complications rates were 5.6% (22/396) vs. 4.0% (10/247), respectively (p=0.393). When postoperative infectious complications were compared according to the duration of antibiotics (Group 1 vs. Group 2) in the TURP and HOLEP groups, the infectious complications rates were 6.3% (12/192) vs. 1.0% (1/103) (p=0.035) and 4.9% (10/203) vs. 6.0% (8/134) (p=0.677), respectively. The duration of Foley catheterization was independently associated with infectious complications (p=0.003).
Conclusions: The results showed that prolonged postoperative catheterization affects postoperative infectious complications associated with transurethral prostate surgery. Although antibiotics administered for less than one day are effective for antibiotic prophylaxis of transurethral prostate surgery, a longer antibiotic therapy is recommended for TURP.
- 3,428 View
- 24 Download


 KAUTII
KAUTII

 First
First Prev
Prev


