-
Primary Bladder and Ureteral Amyloidosis Initially Diagnosed as Chronic Cystitis: A Case Report
-
Seungsoo Lee, Dan Bee Lee, Hyun Jung Lee, Won Hoon Song, Sung-Woo Park, Jong Kil Nam
-
Urogenit Tract Infect 2025;20(3):167-172. Published online December 31, 2025
-
DOI: https://doi.org/10.14777/uti.2550038019
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
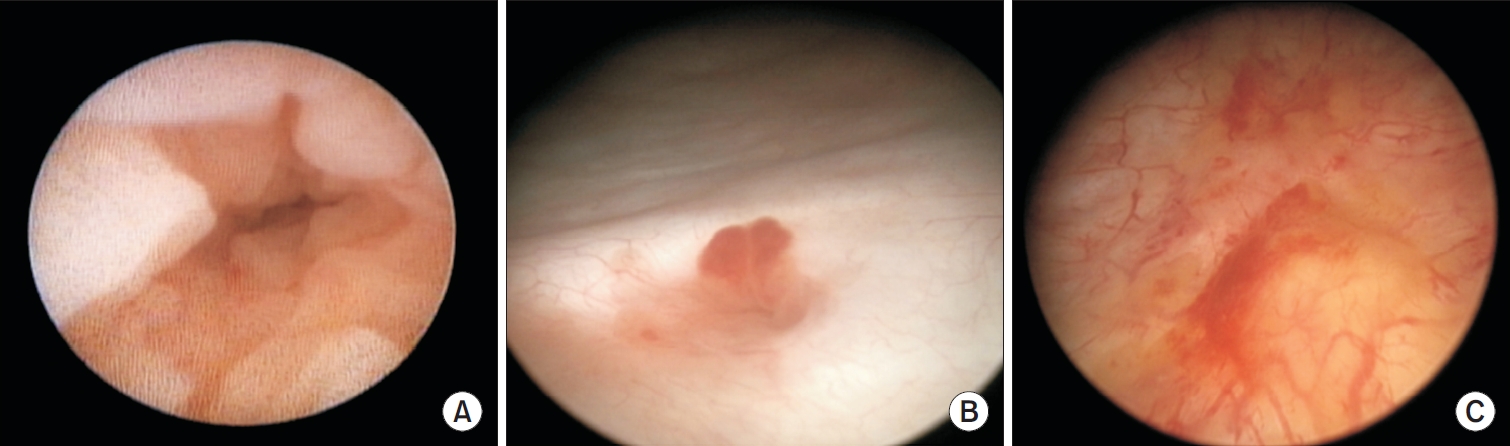
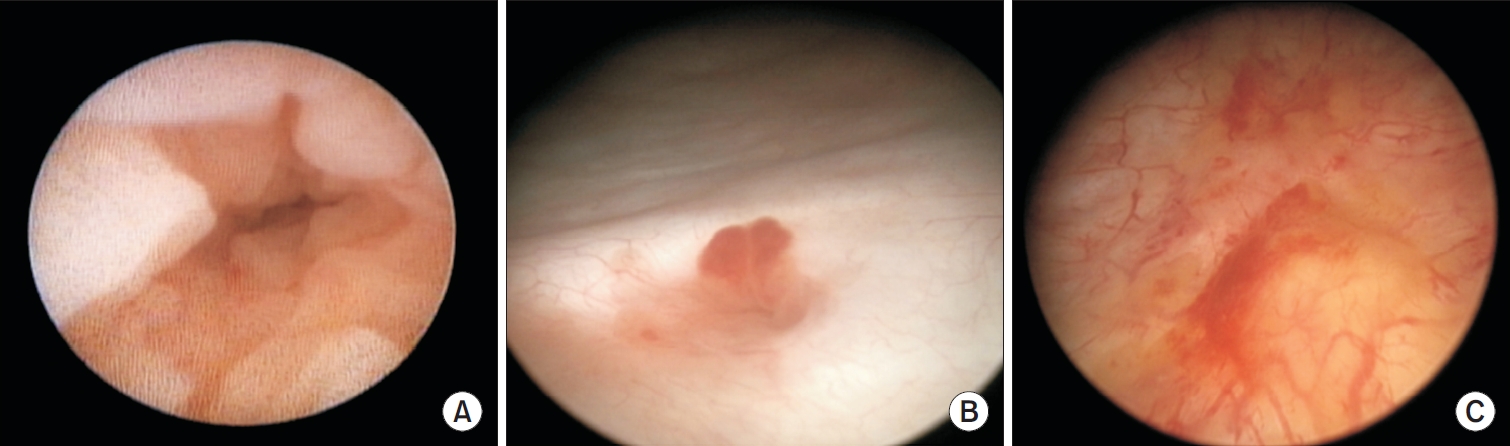
- Primary localized amyloidosis confined to the urinary tract is uncommon and frequently misinterpreted due to clinical and radiologic overlap with more prevalent conditions. We describe a 69-year-old woman who experienced recurrent gross hematuria over 2 years and underwent initial transurethral resection based on a presumptive diagnosis of chronic cystitis. Subsequent evaluation revealed a left ureteral mass with hydronephrosis, raising concern for malignancy. Histopathologic examination of both bladder and ureteral specimens demonstrated amorphous eosinophilic deposits that stained positive with Congo red and showed apple-green birefringence under polarized microscopy. Immunofluorescence confirmed λ-light-chain predominance, establishing AL (amyloid light chain)-type amyloidosis without systemic involvement. The patient underwent complete endoscopic resection and remains asymptomatic during ongoing surveillance. This case highlights the diagnostic challenges posed by localized urinary amyloidosis and underscores the importance of histologic confirmation in atypical inflammatory lesions.
-
Risk Factors of Febrile Urinary Tract Infection after Ureteral Reimplantation in Infant
-
Seungsoo Lee, Jae Min Chung, Sang Don Lee
-
Urogenit Tract Infect 2020;15(2):33-37. Published online August 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.2.33
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: Children with febrile urinary tract infection (fUTI) and vesicoureteral reflux (VUR) show significant morbidity. Few studies have examined the incidence of fUTI after ureteral reimplantation for congenital urinary tract anomalies, particularly in infants. Therefore, this study examined the incidence and risk factors of fUTI after ureteral reimplantation in infants.
Materials and Methods: Children under one year of age, who underwent ureteral reimplantation from July 2017 to December 2018, were reviewed retrospectively. The patients’ data were analyzed to evaluate the predictors of fUTI after ureteral reimplantation.
Results: Ureteral reimplantation was performed in 16 patients (25 ureters) at a mean of 8.9±2.8 months. The preoperative diagnosis was VUR 14 (87.5%), obstructive megaureter 1 (6.3%), duplicated ureter 1 (6.3%). Postoperative fUTI occurred in five patients (31.3%) during the follow-up period (average 9.6±5.9 months, range 3-18 months). UTI occurred at 40.8±16.6 (17-61) days after surgery. Fourteen ureters were implanted with a ureteral catheter for three days, and 11 ureters were implanted with a double J ureteral stent for six weeks. The children’s age, sex, surgical method, renal scar, reflux grade, laterality, persisting VUR, and presence of double J ureteral stent were not predictive factors for postoperative fUTI.
Conclusions: The incidence of fUTI after ureteral reimplantation in infants was 31.3%, and all fUTI occurred within two months after surgery. The risk factors associated with fUTI after ureteral reimplantation could not be predicted.
-
Citations
Citations to this article as recorded by  - Open vs. robot-assisted laparoscopic ureteral reimplantation in a contemporary pediatric cohort: a retrospective single-institution analysis
Suhaib Abdulfattah, Nicole J. Kye, Sanjay Aiyar, Emily Ai, Marina Quairoli, Meghan F. Davis, Karl Godlewski, Katherine Fischer, Christopher J. Long, Dana A. Weiss, Aseem R. Shukla, Arun K. Srinivasan, Sameer Mittal
Journal of Robotic Surgery.2026;[Epub] CrossRef - Etiological Agents of Urinary Tract Infection (UTI)
Rana Thamer Hadi Alkhafaji, M. Jayashankar
International Journal of Scientific Research in Science and Technology.2022; : 381. CrossRef
-
2,980
View
-
10
Download
-
2
Crossref
-
Is Preoperative Pyuria Associated with Postoperative Febrile Complication after Ureteroscopic Ureter or Renal Stone Removal?
-
Seungsoo Lee
-
Urogenit Tract Infect 2020;15(1):1-5. Published online April 30, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.1.1
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: The association between preoperative pyuria and postoperative febrile complications after ureteroscopic ureter or renal stone removal was examined.
Materials and Methods: From June 2014 to July 2016, 110 patients who underwent ureteroscopic ureter or renal stone removal by a single surgeon were evaluated. The patients were categorized as the “pyuria group” and “nonpyuria group.” The sex, age, stone laterality, stone location, stone size, preoperative urine culture results, and postoperative complications in each group were analyzed.
Results: The pyuria and nonpyuria groups were comprised of 55 patients each. The mean ages the pyuria and nonpyuria groups were 58.4±16.1 years and 54.4±13.2 years, respectively. There were respectively, 43 and 12 unilateral and bilateral stones in the pyuria group, and 53 and two in the nonpyuria group. The stone sizes of the pyuria and nonpyuria groups were 13.1±5.4 mm and 11.1±4.7 mm, respectively. The pyuria group contained more patients with bilateral stones and larger stones than the nonpyuria group. Five and two postoperative febrile complications were encountered in the pyuria group and the nonpyuria group, respectively. No significant difference in febrile complications was observed between the two groups. In logistic regression analysis, bilateral stones and larger stones were associated with pyuria.
Conclusions: In ureteroscopic stone removal surgery, preoperative pyuria was associated with bilateral and larger stones, but there were no associations with febrile complications.
-
Von Brunn’s Nest in an Incidental Bladder Mass Found during Holmium Laser Enucleation of the Prostate
-
Seungsoo Lee
-
Urogenit Tract Infect 2020;15(1):13-15. Published online April 30, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.1.13
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- A 62-year-old male with benign prostatic hyperplasia underwent holmium laser enucleation of the prostate. During surgery, a small nodular mass was found incidentally in the trigone of the bladder. The lesion was removed completely by a transurethral resection with a bipolar device. A pathology examination of the lesion indicated von Brunn’s nests.
-
Predictive Parameters of Testicular Salvage of Pediatric Testicular Torsion: A 6-Year Experience of a Single Center
-
Seungsoo Lee, Bu Kyung Park, Moon Kee Chung, Jae Min Chung, Sang Don Lee
-
Urogenit Tract Infect 2016;11(1):25-29. Published online April 30, 2016
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: We evaluated parameters associated with testicular salvage in boys with testicular torsion.
Materials and Methods: During 2009-2014, 19 boys younger than 18 years old underwent emergency surgery for testicular torsion in our hospital. Age, chief complaint, laterality of the torsion, physical appearance, ultrasonographic results, duration between the onset of symptoms and hospital visit, duration between the onset of symptoms and start of surgery, intraoperative appearance, surgical method (orchiopexy or orchiectomy), and any postoperative complications were analyzed retrospectively. Cases were categorized according to salvageable testes (n=14) or unsalvageable testes (n=5) groups based on testes viability.
Results: The mean age was not significantly different between the two groups. All patients were diagnosed using color Doppler ultrasonography of the scrotum. Six (42.9%) boys in the salvageable testes group and all five in the unsalvageable testes group were transferred from other clinics or hospitals (p=0.026). The mean duration between the onset of symptoms and hospital visit was 925 minutes in the salvageable testes group and 3,488 minutes in the unsalvageable testes group (p=0.042), and the mean duration between the onset of symptoms and start of surgery was 1,131 minutes in the salvageable testes group and 3,777 minutes in the unsalvageable testes group (p=0.042).
Conclusions: There was a high possibility that orchiectomy was required if surgery was delayed. However, even when a boy is admitted to the hospital more than 24 hours after the onset of symptoms, the testis can still be viable provided the surgery is performed as quickly as possible.
-
Characteristics of Patients Who Visited the Emergency Room after Prostate Biopsy: Single Center Retrospective Study
-
Seung Chan Jeong, Seungsoo Lee, Jae Min Chung, Sang Don Lee
-
Urogenit Tract Infect 2015;10(2):120-125. Published online October 31, 2015
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose: To educate patients and prevent biopsy-related complications, it is helpful to understand the causes for visiting the emergency room (ER). Therefore, we want to analyze the causes and factors of complications that cause patients to visit the ER after prostate biopsy.
Materials and Methods: We conducted a study of in-patients who visited the ER of Pusan National University Yangsan Hospital after prostate biopsy from December 2008 to July 2015. Age, postoperative interval before visiting the ER, Charlson comorbidity index (CCI) score, symptoms in ER, prostate size, pathologic result, and number of biopsy cores were analyzed retrospectively.
Results: Among all 1,694 cases of patients who had undergone prostate biopsies during a 7-year period, only 37 patients (2.2%) visited the ER. Diabetes mellitus (DM) is the most common underlying disease among patients with accompanying infection-related symptoms compared to patients with accompanying non-infection- related symptoms (p<0.001). In univariate analysis, DM (p=0.004) and CCI score (p=0.030) were statistically significant risk factors for infection, but only DM was significant in multivariate analysis (p=0.004). Prostate size (p=0.044) was a significant risk factor for acute urinary retention (AUR) in univariate analysis, but not statistically significant in multivariate analysis. CCI score was a statistically significant risk factor for bleeding (p=0.005 [univariate], 0.035 [multivariate]).
Conclusions: AUR after transrectal ultrasound-biopsy is the most common reason for visiting the ER. CCI score showed correlation with bleeding and DM showed correlation with infection. Consideration of risk factors of complications after prostate biopsy will be helpful to the patients in the treatment and prevention of complication.
-
Is Postoperative Prophylactic Antibiotics Necessary for Pediatric Scrotal and Inguinal Outpatient Surgeries?
-
Seungsoo Lee, Chang Soo Park, Sung Hye Jo, Sang Don Lee
-
Korean J Urogenit Tract Infect Inflamm 2014;9(2):111-114. Published online October 31, 2014
-
-
-
 Abstract Abstract
 PDF PDF
- Purpose
Excess usage of antibiotics can cause complications of antibiotics and rise of antibiotic-resistant strains. However, guidelines for antibiotic prophylaxis differ between countries. We evaluated necessity of postoperative prophylactic antibiotics for pediatric patients who underwent scrotal and inguinal outpatient surgeries. Materials and Methods: From April 2011 to April 2014, 725 patients (mean age, 30.5±21.6 months) who underwent outpatient surgery (hydrocelectomy, orchiopexy, orchiectomy, and inguinal herniorrhaphy) were evaluated. In group 1 (556 cases), each patient had intravenous antibiotic prophylaxis only preoperatively. In group 2 (169 cases), each patient had intravenous antibiotic prophylaxis pre- and post-operatively. In group 1 and group 2, we analyzed postoperative complications including wound dehiscence, fever, skin erythema, pain, pus, and diarrhea with medical records. Results: In group 1 and group 2, mean age was 30.4±21.7 months (5.0-108.0 months) and 30.8±21.2 months (7.0-108.0 months), respectively. In group 1 and group 2, the mean operative time was 29.6±2.4 minutes and 29.7±2.5 minutes, respectively. The differences of mean age and mean operative time were not statistically significant (p=0.82 and p=0.77, respectively). Nine patients in group 1 and two patients in group 2 had postoperative complications. The difference between two groups was statistically insignificant (p=0.69). According to age and operation, the differences of postoperative complications were not statistically significant. However, in patients under 2 years old, more complications tended to occur in group 1 than in group 2. Conclusions: Postoperative prophylactic antibiotics may not be necessary for pediatric scrotal and inguinal outpatient surgeries.
|