-
Effect of Residual Stone Fragments on Patient-Reported Quality of Life after Endoscopic Kidney Stone Surgery
-
Sang Hee Lee, Jun-Koo Kang, Jae-Wook Chung, Yun-Sok Ha, Jun Nyung Lee, Seock Hwan Choi, Hyun Tae Kim, Tae-Hwan Kim, Eun Sang Yoo, Tae Gyun Kwon, Bum Soo Kim
-
Urogenit Tract Infect 2024;19(2):31-39. Published online August 31, 2024
-
DOI: https://doi.org/10.14777/uti.2024.19.2.31
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
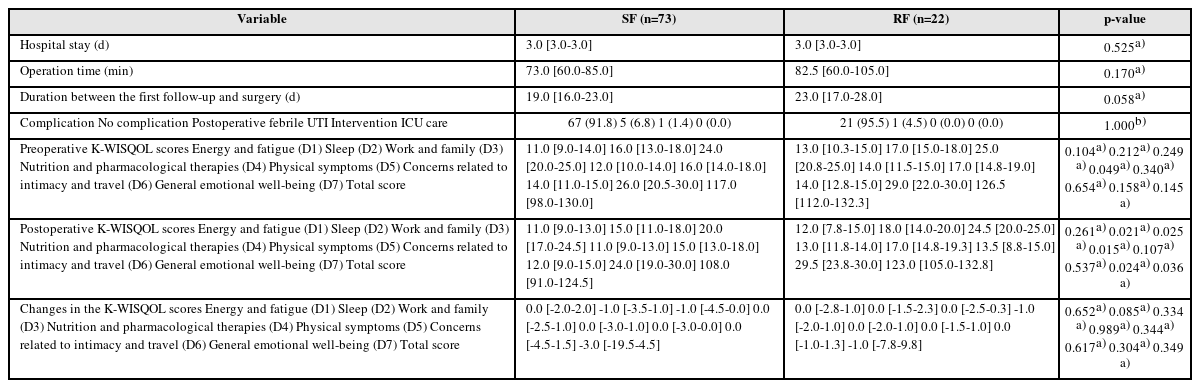
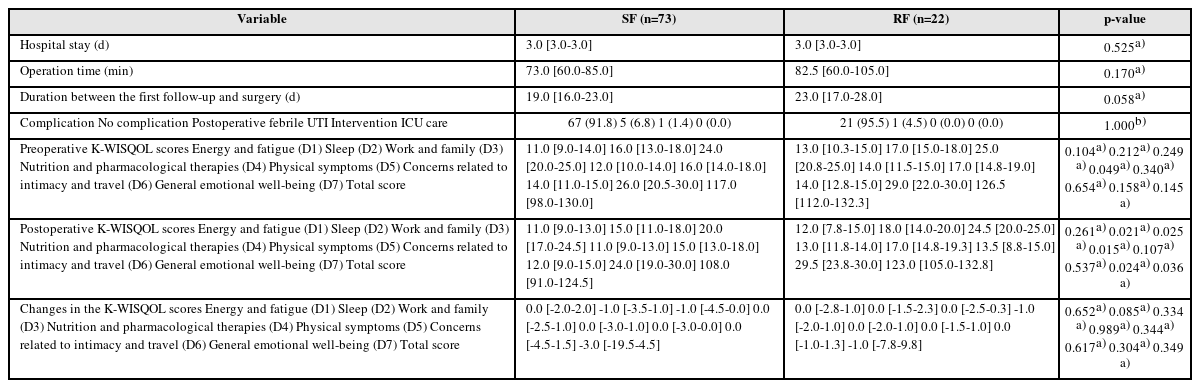
- Purpose: This study examined the effects of residual fragments (RF) on the patient-reported quality of life (QOL) after kidney stone surgery, such as retrograde intrarenal surgery (RIRS) and percutaneous nephrolithotomy (PCNL), using the Korean version of the Wisconsin Stone Quality of Life Questionnaire (K-WISQOL).
Materials and Methods: The medical records of 156 patients who underwent RIRS or PCNL and completed the preoperative and postoperative K-WISQOL from January 2021 to September 2023 were analyzed retrospectively. The patients were divided into RIRS and PCNL groups by the surgical method. The participants completed the K-WISQOL within four weeks before and after treatment. The patients’ baseline characteristics, surgical outcomes, and K-WISQOL scores were compared according to the presence of RF in each surgical group.
Results: Of the 156 patients, 95 underwent RIRS, and 61 underwent PCNL. In the RIRS group, the patients’ baseline characteristics and surgical outcomes were similar in the stone-free (SF) and RF subgroups. The changes in all K-WISQOL domain scores and total scores were similar in the two subgroups. In the PCNL group, the RF subgroup had a significantly higher proportion of staghorn stones, a significantly larger mean stone diameter and significantly longer operation time than those of the SF subgroup. But, the changes in all K-WISQOL domain scores and total scores were not significantly different between the two subgroups, as observed in the RIRS group.
Conclusions: This study showed that the presence of RFs after endoscopic kidney surgery did not affect the short-term patient-reported QOL regardless of the surgical methods.
-
Is Routine Voiding Cystourethrogram Necessary Following Endoscopic Subureteral Injection for Primary Low-Grade Vesicoureteral Reflux?
-
Jun-Koo Kang, Min Ji Park, Min Hyun Cho, Jun Nyung Lee
-
Urogenit Tract Infect 2024;19(1):10-15. Published online April 30, 2024
-
DOI: https://doi.org/10.14777/uti.2024.19.1.10
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
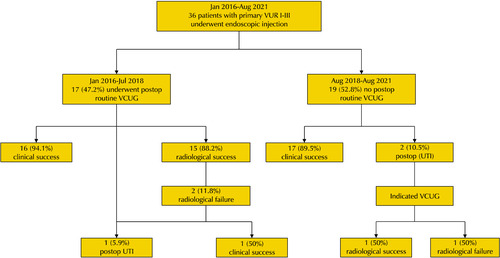
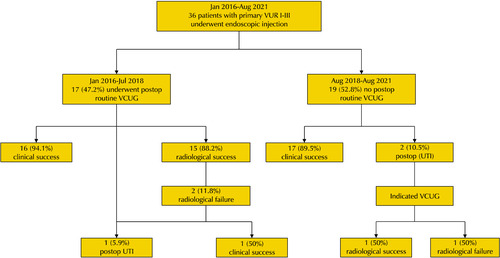
- Purpose: An endoscopic subureteral injection (EI) using a bulking agent is a highly successful surgical procedure, particularly for low-grade vesicoureteral reflux (VUR). Despite the serious adverse effects, routine voiding cystourethrogram (VCUG) to determine radiographic success after EI remains controversial. This study evaluated the necessity of routine postoperative VCUG in children with primary low-grade VUR.
Materials and Methods: From January 2016 to August 2021, children who underwent EI for primary low-grade (I-III) VUR with a history of febrile urinary tract infection (fUTI) were analyzed retrospectively. From January 2016 to July 2018, routine VCUG following EI was performed on all children. Thereafter, postoperative VCUG was performed only if indicated. Clinical success was defined as no fUTI during a 12-month follow-up, and radiographic success was defined as the disappearance of VUR on postoperative VCUG. The clinical and radiographic outcomes in both groups were compared.
Results: Thirty-six children were analyzed in this study. Three children (8.3%) experienced postoperative fUTI. In the routine group, clinical and radiographic success was observed in 16/17 (94.1%) and 15/17 (88.2%), respectively. Two children in the routine group experienced radiographic failure. Among these, one child showed clinical success, and the other underwent additional EI due to clinical failure. Of the indicated group, clinical failure was observed in 2/19 (10.5%). Of them, persistent VUR was identified in one child.
Conclusions: Clinical and radiologic success after EI for primary low-grade VUR is high, and routine VCUG for confirming radiographic success has a limited impact on the clinical course.
-
Successful Treatment of Seminal Vesicle Abscess with Rectal Fistula after Rectal Decompression: Report of a New Case
-
Jae-Wook Chung, Yun-Sok Ha, Jun Nyung Lee, Hyun Tae Kim, Eun Sang Yoo
-
Urogenit Tract Infect 2016;11(3):114-117. Published online December 31, 2016
-
-
-
 Abstract Abstract
 PDF PDF
- Seminal vesicle abscess is a rare urologic disease. Herein, we report our experience of the first case of a 41-year-old male patient with neurogenic bladder who underwent successful treatment of seminal vesicle abscess with rectal fistula after rectal decompression. Only a simple insertion of the rectal tube with intravenous antibiotics was able to remove the seminal vesicle abscess with rectal fistula without any percutaneous, transvesical, or transurethral drainage of the abscess. Rectal decompression should be considered in advance as a treatment of seminal vesicle abscess with rectal fistula before performing any invasive abscess drainage or fistulectomy.
-
Median Raphe Cysts of the Scrotum and Perineum Presenting with Recurrent Infection
-
Jun Nyung Lee, Hyun Tae Kim, Sung Kwang Chung
-
Korean J Urogenit Tract Infect Inflamm 2014;9(2):119-121. Published online October 31, 2014
-
-
-
 Abstract Abstract
 PDF PDF
- Median raphe cysts of the perineum are rare congenital anomalies of the male genitalia, which form during embryological development, and can be found in the midline from the distal penis to the perineum. However, the incidence of median raphe cyst is likely under-reported and under-recognized. We report on the case of a median raphe cyst extending from the scrotum to the perineum with recurrent infection and purulent discharge in a 28-year-old man, which first developed at the age of 5 years. We believe it is important that urologists recognize median raphe cysts and have knowledge of their management in order to provide appropriate information to patients.
|