-
Impact of Antibiotics on the Efficacy of Immune Checkpoint Inhibitors in Metastatic Urothelial Carcinoma
-
Do Gyeong Lim, Ho Yeon Lee, Ho Seok Chung, Eu Chang Hwang, Seung Il Jung, Dong Deuk Kwon
-
Urogenit Tract Infect 2023;18(3):75-81. Published online December 31, 2023
-
DOI: https://doi.org/10.14777/uti.2023.18.3.75
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: Emerging evidence has suggested that prior or concurrent antibiotic (ATB) use may be associated with a poor response to immune checkpoint inhibitors (ICIs) in patients with some solid tumors. This study examined the effects of ATB use on the oncological outcomes of patients receiving ICIs for mUC.
Materials and Methods: Patients receiving ICIs for mUC between 2018 and 2020 were assessed retrospectively. Those with over three cycles of atezolizumab or pembrolizumab were included. ATB use, defined as ≥ three days within 60 days before or three months after ICI administration, was compared between groups for oncological outcomes.
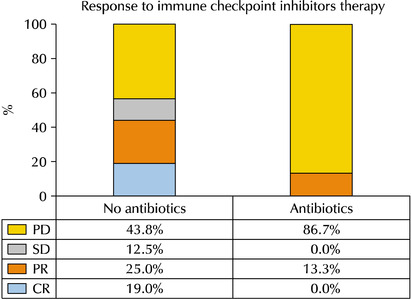
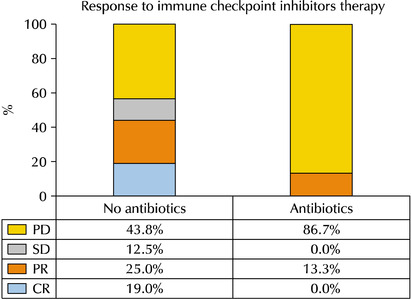
Results: Thirty-one patients were examined. The ATB-use and no-ATB-use groups consisted of 15 (48.4%) and 16 patients (51.6%), respectively. The ATB-use group showed a lower disease control rate (56.3% vs. 13.3%, p=0.023) than the no-ATB-use group. The objective response rate in the ATB-use group was lower than the no-ATB-use group, but the difference was statistically insignificant (43.7% vs. 13.3%, p=0.113). The ATB-use group had shorter progression-free survival (median three vs. six months, log-rank p=0.045) and shorter overall survival (median three vs. 14 months, log-rank p=0.023) than the no-ATB-use group. The most commonly used antibiotics were fluoroquinolones (46.7%), cephalosporins (40.0%), non-cephalosporin beta-lactams (6.7%), and nitrofurantoin (6.7%).
Conclusions: ATB may be associated with poorer oncological outcomes in patients with mUC who received ICI therapy. Hence, further research will be needed to understand the relationship between the modulation of ATB-related dysbiosis and gut microbiota composition with the oncological outcomes in patients with mUC.
-
Performance of the Sysmex UF-1000i System in Screening for Significant Bacteriuria in Patients with Bladder Cancer Who Received Bacillus Calmette-Guérin Treatment
-
Tae Hee Kim, Seung Il Jung, Myung Soo Kim, Hyun-Jung Choi, Ho Seok Chung, Eu Chang Hwang, Dong Deuk Kwon
-
Urogenit Tract Infect 2020;15(2):38-46. Published online August 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.2.38
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: Diagnosing urinary tract infections by urine culture is time-consuming during a Bacillus Calmette-Guérin treatment. Because the urine culture results take time to collect, patients are treated presumptively, or Bacillus Calmette-Guérin is discontinued before the results. This study evaluated the ability of the Sysmex UF-1000i system to examine the urine bacterial count and determine if it could be used to predict a positive culture.
Materials and Methods: 180 patients who underwent transurethral resection for bladder tumors and received intravesical Bacillus Calmette-Guérin treatment between January 2017 and July 2018 were evaluated prospectively. For patients who received an intravesical Bacillus Calmette-Guérin treatment, urine flow cytometry, and urine cultures were assessed weekly during the treatment period.
Results: During Bacillus Calmette-Guérin instillation, 44, 146, and 27 patients had bacteriuria, pyuria, and positive urine nitrite, respectively. Multivariate analysis indicated that the predictors associated with bacteriuria included the urine flow cytometry results of >100 bacteria/µl (odds ratio, 22.73; p<0.001) and positive urine nitrite (odds ratio, 5.67; p=0.012) at the time of sampling for positive urine culture. The area under the receiver operative characteristic curve for diagnosing bacteriuria by urine flow cytometry was 0.825. A urine flow cytometry cutoff value of >100 bacteria/µl resulted in a sensitivity and specificity of 75% and 90.91%, respectively. Using the cutoff of >1,000 bacteria/µl, the sensitivity and specificity were 50% and 94.85%, respectively.
Conclusions: Rapid urinary tract infection diagnosis using Sysmex UF-1000i can be used to determine whether to treat an infection and to avoid unnecessary Bacillus Calmette-Guérin discontinuation and urine culture tests.
-
Citations
Citations to this article as recorded by  - Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
Ali Bourgi, Omar Ghanem, Camille Brocail, Franck Bruyère
Surgical Infections.2025; 26(6): 390. CrossRef
-
1,877
View
-
2
Download
-
1
Crossref
-
Rates and Risk Factors of Bacteriuria in Patients with Bladder Cancer Who Underwent Treatment with Bacillus Calmette-Guérin
-
Seong Jong Eun, Myung Soo Kim, Seung Il Jung, Hyun-Jung Choi, Ho Seok Chung, Eu Chang Hwang, Dong Deuk Kwon
-
Urogenit Tract Infect 2020;15(2):47-53. Published online August 31, 2020
-
DOI: https://doi.org/10.14777/uti.2020.15.2.47
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study evaluated the rate and predictors of bacteriuria in patients who underwent transurethral resection of bladder tumor (TURBT) and Bacillus Calmette-Guérin (BCG) treatment.
Materials and Methods: We prospectively evaluated 266 patients who underwent TURBT and intravesical BCG treatment between January 2017 and September 2019. Urinalysis and urine culture were performed at the baseline, one to two weeks after TURBT and weekly during the BCG treatment period. The primary outcomes were the bacteriuria rates in BCG-treated patients, while the secondary outcomes were the risk factors of bacteriuria during BCG treatments.
Results: Of the 266 patients, the rate of bacteriuria was 4.5% before TURBT, 5.3% in the postoperative period, and 24.4% in the BCG treatment period. After BCG instillation, urinalysis showed that 204 and 38 patients tested positive for pyuria and nitrite, respectively. Multivariate analysis indicated that the risk factors associated with bacteriuria during BCG treatment included age (odds ratio [OR]: 1.06; p=0.003), sex (female) (OR, 5.41; p=0.007), diabetes mellitus (DM) (OR, 2.82; p=0.023), postoperative bacteriuria (OR, 8.08; p=0.032), bacterial counts>100/µl in urine flow cytometry (OR, 29.72; p<0.001), and positive urine nitrite test (OR, 6.20; p=0.001) at the time of positive urine culture sampling.
Conclusions: Approximately 25% of the patients suffered from bacteriuria during intravesical BCG treatment. Old age, female sex, DM, and postoperative bacteriuria were found to be the risk factors of bacteriuria during BCG treatment. Predictive factors could aid in clinical decisions during BCG treatments as well as decisions on BCG discontinuation.
-
Citations
Citations to this article as recorded by  - Is There Always a Need to Perform Urine Culture before Bacillus Calmette–Guérin Instillation for Bladder Cancer?
Ali Bourgi, Omar Ghanem, Camille Brocail, Franck Bruyère
Surgical Infections.2025; 26(6): 390. CrossRef - MESANE KANSERİ ve ÜRİNER STOMASI OLAN HASTANIN EVDE BAKIMI
Neşe İşcan Ayyıldız
Paramedik ve Acil Sağlık Hizmetleri Dergisi.2024; 5(1): 31. CrossRef - Mesane Kanserinde İntravezikal Bacille Calmette- Guerin (BCG) Uygulaması ve Hemşirenin Sorumlulukları
Ayla YAVUZ KARAMANOĞLU, Ali Ersin ZÜMRÜTBAŞ
Adnan Menderes Üniversitesi Sağlık Bilimleri Fakültesi Dergisi.2023; 7(1): 256. CrossRef
-
3,704
View
-
13
Download
-
3
Crossref
-
Perioperative Risk Factors Related to Systemic Inflammatory Response Syndrome after Percutaneous Nephrolithotomy
-
Ho Seok Chung, Seung Il Jung
-
Urogenit Tract Infect 2019;14(1):9-13. Published online April 30, 2019
-
DOI: https://doi.org/10.14777/uti.2019.14.1.9
-
-
 Abstract Abstract
 PDF PDF
- Percutaneous nephrolithotomy (PCNL) has become the standard treatment for large and complex kidney stones since its introduction in 1976. On the other hand, postoperative complications are not rare and can be quite significant. Of these complications, postoperative infectious complications, such as systemic inflammatory response syndrome (SIRS), remain a seminal event and a possible cause of perioperative mortality. Several recent studies have found a number of factors that increase the risk of SIRS after PCNL. These include preoperative factors (patient’s characteristics) and factors associated with the intraoperative and postoperative findings. The present study describes the perioperative risk factors of SIRS after PCNL. These findings can help decrease the incidence of infectious complications, including SIRS, in patients undergoing PCNL.
-
Citations
Citations to this article as recorded by  - Can we predict the incidence of high-grade Clavien-Dindo complications in patients with forgotten encrusted stents undergoing endourologic management?
Praanjal Gupta, Ramanitharan Manikandan, Lalgudi Narayanan Dorairajan, Kodakattil Sreenivasan Sreerag, Sidhartha Kalra, Swapnil Singh Kushwaha
Asian Journal of Urology.2024; 11(1): 99. CrossRef
-
869
View
-
0
Download
-
1
Crossref
-
Optimal Modified Extended Antibiotic Prophylaxis for Prostate Biopsy: The Addition of Two Intravenous Doses of Amikacin to Ciprofloxacin
-
Seong Hyeon Yu, Seung Il Jung, Myung Soo Kim, Ho Seok Chung, Dong Deuk Kwon
-
Urogenit Tract Infect 2018;13(3):72-78. Published online December 31, 2018
-
DOI: https://doi.org/10.14777/uti.2018.13.3.72
-
-
 Abstract Abstract
 PDF PDF
- Purpose: This retrospective study was undertaken to investigate whether increasing amikacin dosage for ciprofloxacin prophylaxis in patients with fluoroquinolone (FQ)-resistant rectal flora reduce infectious complications after transrectal ultrasound-guided prostate biopsy (TRUSPB).
Materials and Methods: A total of 430 patients with FQ-resistant rectal flora based on rectal swab cultures were divided into two groups. Patients in both groups were administered ciprofloxacin (400 mg, intravenous [IV], twice daily) on the same day as TRUSPB and one day after biopsy. However, whereas group 1 patients (n=202) were administered a single injection of amikacin (1g, IV) one hour before TRUSPB, patients in group 2 (n=228) were administered two injections of amikacin (1g, IV) before one hour TRUSPB and again on the day after TRUSPB.
Results: Of the 430 study subjects, 129 (30.0%) showed extended-spectrum beta-lactamase (ESBL) positivity. The overall incidence rate of infectious complications was 2.8% (12/430). Infectious complication rates were 4.0% (8/202) in group 1 and 1.3% (3/228) in group 2 (p=0.075). Urinary tract infection and acute prostatitis were more frequent in group 1 (3.5% vs. 0.4%, p=0.029). Infectious complication rates in ESBL negative patients were 3.4% (5/145) in group 1 and 1.3% (2/156) in group 2, whereas those in ESBL positive patients were 7.0% (4/57) in group 1 and 1.4% (1/72) in group 2.
Conclusions: Increasing the dosage of amikacin for ciprofloxacin prophylaxis reduce infectious complications in patients with FQ-resistant rectal flora and to be more effective in ESBL positive patients with FQ-resistant rectal flora.
|