-
Impact of Microbial Infection on Sperm Parameters of Seminal Bacteria in Asymptomatic Subfertile Males
-
Sae Byuk Chang, Tae Jin Kim, Tae Heon Kim, Seung-Ryeol Lee, Young Kwon Hong, Dong Soo Park, Sun-Mi Cho, Dong Hyeon Lee, Young Dong Yu
-
Urogenit Tract Infect 2023;18(3):82-92. Published online December 31, 2023
-
DOI: https://doi.org/10.14777/uti.2023.18.3.82
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Purpose: This study examined the effects of asymptomatic bacteriospermia on the semen quality of subfertile males. The types of bacteria and their antibiotic susceptibility were also analyzed.
Materials and Methods: Semen was collected and analyzed from 510 subfertile males. One hundred and seventy-nine males showed bacteriospermia, while 331 males did not. The bacterial species, sperm parameters, hormone levels, underlying disease, and lifestyle patterns were compared between the two study groups.
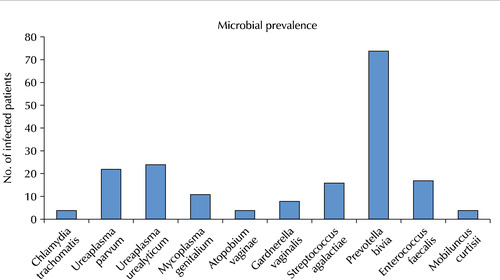
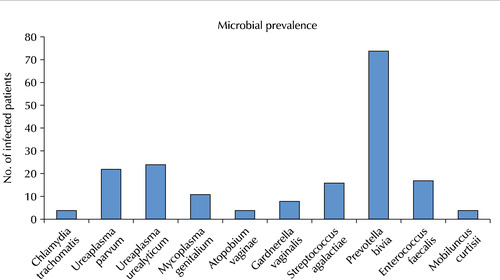
Results: The bacteriospermic males showed significantly higher rates of leukocytospermia (p=0.001) and deoxyribonucleic acid (DNA) fragmentation than the non-bacteriospermic males. Sperm motility was significantly lower in the bacteriospermic males than in non-bacteriospermic males. The most common seminal bacterial species were Prevotella bivia (P. bivia, 41.3%) and Ureaplasma urealyticum (U. urealyticum, 13.4%). U. parvum showed the highest recurrence rates (31.8%) three months after the initial antibiotic treatment. Regarding the sperm parameters of bacteriospermic males, the sperm concentration, total motility, progressive motility, leukocytospermia, and DNA fragmentation were improved significantly after the initial antibiotics treatment. Multivariate logistic regression analyses revealed P. bivia, U. urealyticum, and U. parvum to be associated with the decreased motility and increased DNA fragmentation of spermatozoa. P. bivia was also associated with a decreased sperm concentration (p=0.002) and vitality (p=0.013).
Conclusions: Bacteriospermia decreased the sperm concentration, motility, normal morphology, and vitality. P. bivia is the most commonly observed bacteria in subfertile males. Appropriate antibiotic therapy of seminal bacteria species had a strong positive impact on improving the semen parameters.
-
Changes of Interleukin-1β in the Prostate Secretions of Chronic Nonbacterial Prostatitis Patients
-
Hana Yoon, Dong Hyeon Lee
-
Korean J Urogenit Tract Infect Inflamm 2011;6(1):48-53. Published online April 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: To measure changes in prostate cytokine secretion in chronic non-bacterial prostatitis (NBP) patients and examine the clinical usefulness of these changes in differentiating the pathophysiologic mechanism of NBP and subsequent selection of treatment modalities. Materials and Methods: Sixty male patients were diagnosed with chronic NBP, and a control group comprised of 30 male patients without clinical evidence of NBP were enrolled in this study. Prostate secretion (centrifuged VB3) was analyzed at the initialdiagnosis and 8 weeks after treatment initiation. Patients who showed more than 10 white blood cells (WBCs)/high power field (HPF) 8 weeks after treatment initiation were categorized into group A. Group B patients had less than 3 WBCs/HPF. Group B was further subclassified into two groups according to presence of symptoms after treatment: Bp (symptom-persisted) and Br (symptom-resolved). IL-1β, C3, C4, IgG were measured and the results were analyzed. Results: There were significant differences in the IL-1β level in the control group compared to group A, Bp and Br (p<0.05). C3, C4, IgG showed higher levels in groups A and B than in the control group, albeit without statistical significance (p>0.05). Conclusions: Elevated IL-1β in group Bp suggests that chronic NBP patients who did not respond to treatment could exhibitclinical manifestations of autoimmune reactions rather than infection of external origin. We suggest that a more advanced diagnostic technique using cytokine at the initial stage of disease manifestation tohelp clinicians avoid unnecessary antibiotic treatment and manage the condition more effectively."
-
The Effect of Inflammatory Histological Extent of Prostate on the Lower Urinary Tract Symptoms in Benign Prostatic Hyperplasia Patients
-
Seong Ju Lee, Dong Hyeon Lee, Young Yo Park, Bongsuk Shim, Woon-Sup Han
-
Korean J Urogenit Tract Infect Inflamm 2011;6(1):54-60. Published online April 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- "Purpose: to investigate for clinical correlation between inflammatory histological findings of the prostate and lower urinary tract symptoms in benign prostatic hyperplasia patients. Materials and Methods: A total of 274 patients whose prostate-specific antigen (PSA) was higher than 4.0 ng/dl, had underwent prostate biopsy. International prostate symptom score questionnaire, uroflowmetry, and transrectal ultrasonography were also performed. Patients were divided into 3 groups and granted points according to the extent of lymphocytic infiltration: 0 point for patients with normal findings; 1 point for patients with lower than 50% of lymphocytic infiltration; 2 points for patients with higher than 50% of lymphocytic infiltration or secretor destruction by neutrophil infiltration findings. We quantified the extent of inflammation by using total prostatitis pathology score and classified 0-5 points, 6-10 points, 11-15 points, higher than 16 points into grade 1-4, respectively. Results: Of the 274 patients, 71 who diagnosed with prostate cancer from their biopsy were excluded. Of the remaining 203 patients, 106 (52.21%) were classified grade 1, 57 (28.08%) were grade 2, 31 (15.27%) were grade 3, and 9 (4.43%) were grade 4. There were 142 patients (69.96%) in the group with core 2, which means severe inflammation, and 61 patients (30.04%) in the group without core 2. In addition, prostate volume, storage symptoms score and total scores in IPSS and quality of life were significantly higher in the group with core 2. Conclusions: Lower urinary tract symptoms deteriorated as prostatic inflammation became severe. However, further studies are required to determine correlation more accurately."
|