Diagnostic Utility of the Sysmex UF-5000 Flow Cytometer in Acute Bacterial Prostatitis: A Retrospective Pilot Study
Article information
Abstract
Purpose
To evaluate the diagnostic performance of the Sysmex UF-5000 flow cytometer in detecting acute bacterial prostatitis (ABP) compared to standard urine culture.
Materials and Methods
This retrospective study analyzed 45 urine samples from patients with a clinical diagnosis of ABP. Each sample was evaluated using the UF-5000 to measure red blood cells (RBC), white blood cells (WBC), and bacterial counts, and the results were compared with those from standard urine culture and Gram staining. Receiver operating characteristic curves were generated, and sensitivity, specificity, positive predictive value (PPV), and negative predictive value were determined. Concordance between Gram classification by the UF-5000 and conventional Gram staining was also evaluated.
Results
Of the 45 patients, 84.4% had positive urine cultures. The bacterial count parameter demonstrated the highest diagnostic performance (area under the curve [AUC]=0.79; sensitivity, 89.5%; PPV, 91.9%), outperforming WBC (AUC=0.76) and RBC (AUC=0.55). The Gram classification flag showed an overall concordance of 85.7% with conventional Gram staining, with a concordance rate of 88% for Gram-negative organisms.
Conclusions
The Sysmex UF-5000 exhibited good concordance with urine culture for patients with ABP, particularly through the bacterial count parameter. Although it does not replace culture, the UF-5000 may serve as a rapid adjunctive tool to support early clinical decision-making in suspected ABP cases.
HIGHLIGHTS
The Sysmex UF-5000 presents a rapid and automated alternative to conventional diagnostic methods for acute bacterial prostatitis (ABP). Among the urinary parameters it measures, bacterial counts showed high concordance with culture-positive cases, suggesting its usefulness as an adjunct tool for early clinical assessment. By providing immediate, quantitative results, the UF-5000 may support timely decision-making in suspected ABP cases and reduce dependence on delayed urine culture results.
INTRODUCTION
Acute bacterial prostatitis (ABP), an acute infectious condition of the prostate, is characterized by sudden onset of fever, pelvic pain, dysuria, and systemic signs of inflammation. ABP is considered a urological emergency due to its potential for serious complications including sepsis, prostatic abscess, and transition to chronic bacterial prostatitis if not treated promptly or appropriately [1,2].
Diagnosis of ABP traditionally relies on a combination of clinical findings, digital rectal examination, urinalysis, and urine culture [3]. Among these, urine culture remains the gold standard for confirming bacterial etiology, with thresholds typically set at ≥ 10⁵ colony-forming units (CFU)/mL [4,5]. However, urine culture requires 48 to 72 hours to yield results, potentially delaying definitive treatment. Moreover, empirical antibiotic administration prior to specimen collection might render cultures falsely negative and complicate clinical decisions [6,7].
Automated urine flow cytometry has emerged as a promising adjunct tool for rapid and standardized analysis of urinary particles [8,9]. Sysmex UF-5000 is a third-generation flow cytometer capable of measuring red blood cells (RBCs), white blood cells (WBCs), epithelial cells, and bacteria simultaneously through fluorescence and light scattering technologies. Unlike dipstick testing or manual microscopy, UF-5000 provides quantitative and objective data with rapid turnaround time, typically within minutes [10].
Previous studies have validated the performance of UF-5000 in diagnosing urinary tract infections (UTIs), demonstrating high accuracy in detecting bacteriuria and pyuria, with potential to reduce unnecessary urine cultures [10-17]. While its use in routine UTI screening has been widely studied, data regarding its application in diagnosing ABP, a condition in which early detection is especially critical to prevent complications, are limited.
Thus, the present study aimed to evaluate the diagnostic performance of Sysmex UF-5000, specifically its bacterial, leukocyte, and erythrocyte parameters, in patients diagnosed with ABP. We compared these parameters against urine culture results to assess whether flow cytometric analysis could serve as a rapid and reliable diagnostic adjunct in this clinical context.
MATERIALS AND METHODS
1. Study Design and Population
This was a retrospective, single-center study conducted at a tertiary care hospital in Korea. It aimed to evaluate the diagnostic performance of the Sysmex UF-5000 urine flow cytometer in detecting ABP compared with conventional urine culture. Patients who were clinically diagnosed with ABP between January 2023 and December 2023 were identified through electronic medical records. A total of 45 urine samples from adult male patients were included.
Inclusion criteria were: (1) clinical suspicion of ABP based on fever, pelvic or perineal pain, and lower urinary tract symptoms; (2) urine sample submitted for both UF-5000 analysis and urine culture; and (3) urine analysis performed within 2 hours of sample collection. To ensure accurate differentiation of ABP from other febrile UTIs such as acute pyelonephritis, additional diagnostic features were reviewed. These included: (1) elevated serum prostate-specific antigen levels in the absence of known prostate cancer; (2) prostate tenderness on digital rectal examination, when available, inflammatory markers such as leukocytosis and elevated C-reactive protein, and radiological findings consistent with prostatic inflammation on computed tomography, when performed. Patients with clinical or radiologic features suggestive of upper UTIs like flank pain, costovertebral angle tenderness, and hydronephrosis, those with clearly documented prior antibiotic use before urine collection, or incomplete data were excluded.
2. Sample Collection and Processing
Midstream urine samples were obtained using a clean-catch method. All specimens were submitted for simultaneous analysis using a Sysmex UF-5000 and standard urine culture. UF-5000 analysis was performed within 2 hours of sample collection to minimize cellular degradation and bacterial overgrowth.
The UF-5000 flow cytometer can automatically quantify various urinary components using fluorescence flow cytometry and hydrodynamic focusing. Parameters evaluated in this study included: RBC count (/µL), WBC count (/µL), and bacterial count (/µL). In addition, the UF-5000 provides an automated Gram classification flag categorizing bacteria as Gram-positive, Gram-negative, mixed (both Gram-positive and -negative), or unknown based on optical scatter patterns.
3. Urine Culture and Microbiological Analysis
Urine cultures were performed using calibrated loop plating on blood agar and MacConkey agar, followed by incubation for 24–48 hours. Significant bacteriuria was defined as ≥10⁵ CFU/mL. Extended-spectrum β-lactamase (ESBL) production was recorded where applicable. Gram staining results were recorded for all culture-positive samples. Cases with unknown or unclassified Gram status were excluded from concordance analysis.
4. Data Collection and Variables
Demographic and clinical information, including age and history of diabetes mellitus, were collected. Laboratory parameters included UF-5000 RBC, WBC, and bacteria values, Gram classification flags, and corresponding urine culture results. The primary outcome was the diagnostic accuracy of UF-5000 parameters for predicting culture-positive ABP.
5. Statistical Analysis
Descriptive statistics were used to summarize baseline characteristics. Receiver operating characteristic (ROC) curve analysis was performed to assess the diagnostic performance of each UF-5000 parameter. Area under the curve (AUC), optimal cutoff values, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated.
Concordance between the UF-5000 Gram classification flag and Gram staining results was evaluated, excluding samples with unclassified or missing data. The overall concordance rate and subgroup rates for Gram-positive and Gram-negative organisms were determined. All analyses were performed using IBM SPSS Statistics ver. 26.0 (IBM Corp., USA). A p-value of less than 0.05 was considered statistically significant.
RESULTS
1. Patient Characteristics
A total of 45 patients with clinically diagnosed ABP were included in this study (Supplementary Table 1). Their mean age was 68 years. Seventeen patients (37.8%) had a history of diabetes mellitus. Among all samples, 38 (84.4%) yielded positive urine culture results and 34 (75.6%) had a bacterial count of ≥10⁵ CFU/mL. Escherichia coli (n=23) was the most commonly isolated pathogen, followed by Klebsiella pneumoniae (n=4) and other Gram-negative bacteria (n=6). Four samples showed Gram-positive organisms. ESBL-producing organisms were identified in 5 of 13 tested isolates (38.5%).
2. Diagnostic Accuracy of UF-5000 Parameters
Diagnostic performances of 3 urinary parameters (RBC, WBC, and bacteria) measured by the Sysmex UF-5000 are summarized in Table 1. Among them, the bacterial count parameter showed the highest diagnostic accuracy, with a sensitivity of 89.5%, a specificity of 57.1%, a PPV of 91.9%, and an NPV of 50.0%. The optimal bacterial count threshold was determined to be 56.
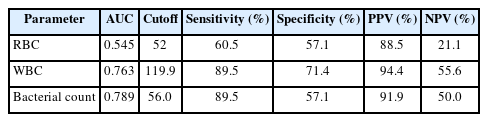
Diagnostic performance of UF-5000 urinary parameters for predicting culture-positive acute bacterial prostatitis
The WBC parameter also demonstrated good diagnostic capability, with a sensitivity of 89.5%, a specificity of 71.4%, a PPV of 94.4%, and an NPV of 55.6%. In contrast, the RBC parameter exhibited limited discriminatory power with a relatively low NPV (21.1%) despite a moderately high PPV (88.5%).
3. ROC Curve Analysis
ROC curve analysis was performed to assess the discriminative ability of each UF-5000 parameter in predicting culture-positive ABP. The ROC curve for the bacterial count parameter showed the highest diagnostic performance, with an AUC of 0.789, indicating good ability to differentiate between culture-positive and culture-negative cases (Fig. 1A). The WBC parameter also showed reasonable discriminative power with an AUC of 0.763, while the RBC parameter demonstrated limited diagnostic value (AUC=0.545) with performance approaching the diagonal line of no discrimination (Fig. 1B and C). These comparisons are visualized in Fig. 1D.
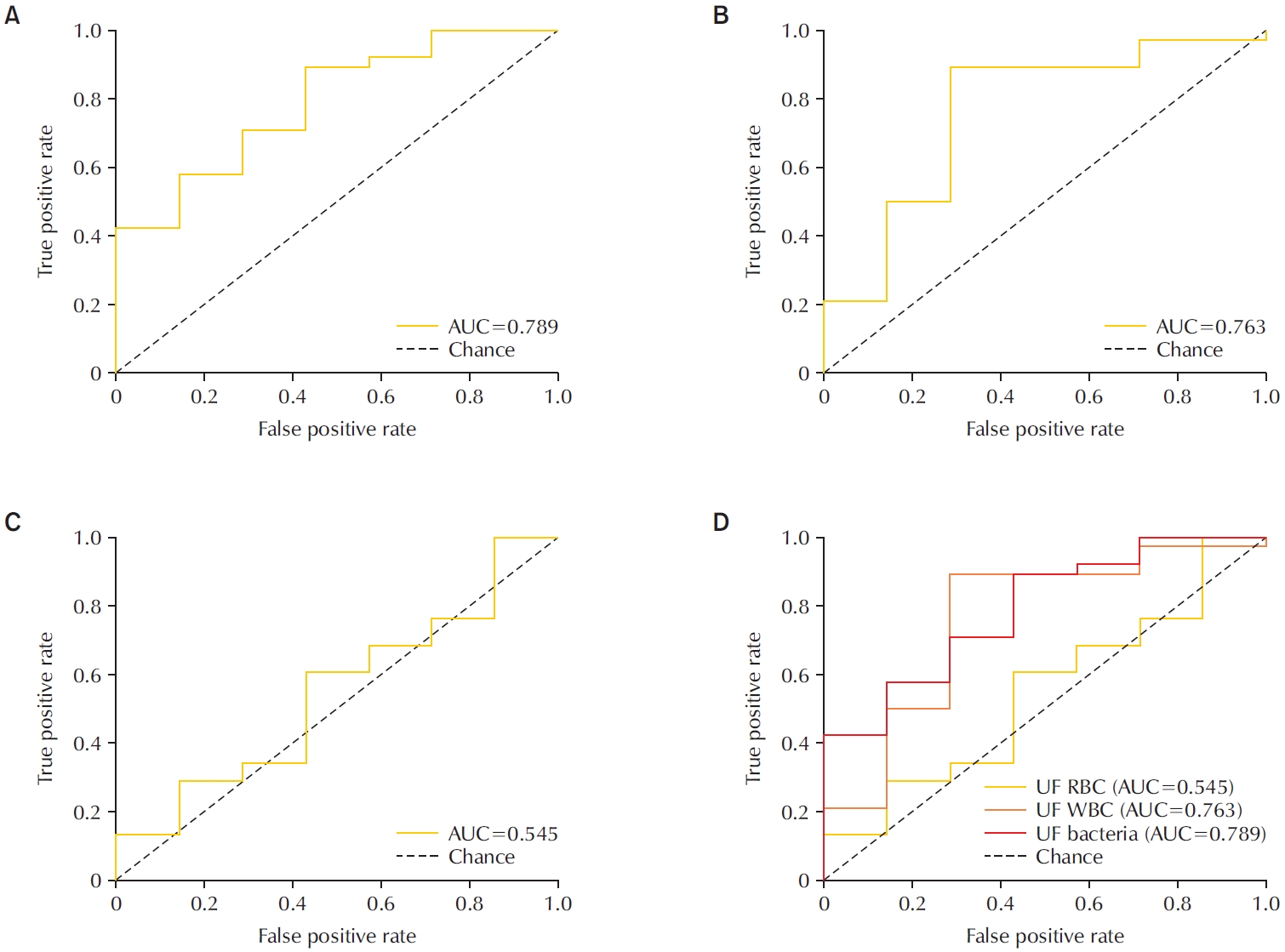
Receiver operating characteristic (ROC) curves for UF-5000 urinary parameters in predicting culture-positive acute bacterial prostatitis. (A) ROC curve for the UF-5000 bacterial count parameter (area under the curve [AUC]=0.789). (B) ROC curve for the UF-5000 WBC parameter (AUC=0.763). (C) ROC curve for the UF-5000 RBC parameter (AUC=0.545). (D) Combined ROC curves comparing the diagnostic performance of RBC, WBC, and bacterial count parameters. RBC, red blood cell; WBC, white blood cell.
4. Concordance With Gram Staining
Among the 37 samples with classifiable Gram staining results, concordance between the UF-5000 Gram flag and standard Gram staining was observed in 85.7% of cases. The concordance rate was higher for Gram-negative bacteria (88.0%) than for Gram-positive organisms (66.7%), as shown in Fig. 2. Nine samples with unclassified Gram status were excluded from this analysis.
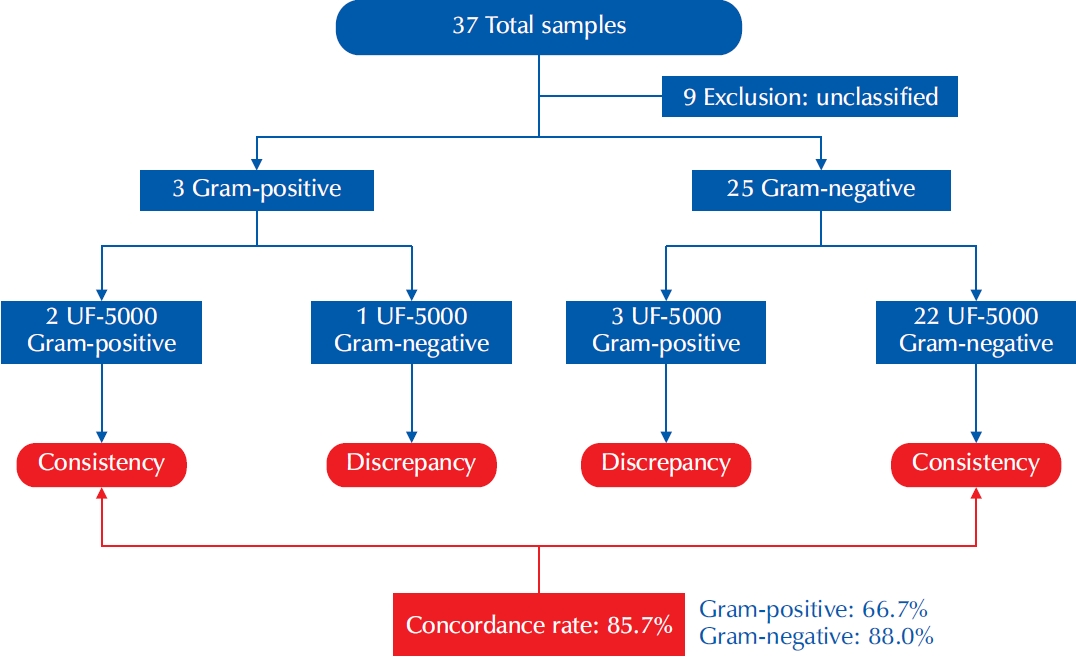
Concordance between UF-5000 Gram classification and conventional Gram staining results in patients with acute bacterial prostatitis. The flowchart illustrates the concordance and discrepancy between Gram stain results obtained by conventional urine culture and the Sysmex UF- 5000 flow cytometer. Of the 37 total samples analyzed, 9 were excluded due to unclassified Gram status.
DISCUSSION
In this study, we assessed the diagnostic performance of the Sysmex UF-5000 flow cytometer in detecting ABP. Among RBC, WBC, and bacterial parameters, the bacterial count parameter demonstrated the highest diagnostic accuracy with an AUC of 0.79, a high sensitivity (89.5%), and a high PPV (91.9%). While not reaching the threshold for excellent discrimination, this level of performance suggests meaningful clinical utility, particularly in settings requiring rapid decision-making.
ABP is often a clinical diagnosis supported by laboratory evidence of infection and inflammation. However, standard urine culture, the gold standard for diagnosis, requires 48 to 72 hours for results. It might be negatively impacted by prior antibiotic use [4-7]. The ability to rapidly detect bacteriuria using automated flow cytometry, especially in febrile patients with suggestive symptoms, could reduce diagnostic delays and improve antimicrobial stewardship.
Our results aligned with prior studies demonstrating that UF-5000 could accurately quantify urinary bacteria and leukocytes and differentiate between infected and non-infected samples [13-17]. The inclusion of RBC and WBC in our analysis was intended to assess whether commonly reported urinalysis parameters from the UF-5000 hold predictive value in ABP. Although both are nonspecific inflammatory markers and may be elevated in noninfectious urologic conditions [18,19], WBC count showed moderate diagnostic performance (AUC=0.76), likely reflecting neutrophil recruitment to the prostate during infection. In contrast, RBC count demonstrated poor performance (AUC=0.55), supporting prior observations that hematuria lacks diagnostic specificity in ABP [20].
The concordance analysis between UF-5000 Gram classification and traditional Gram staining revealed an overall agreement of 85.7%, with a concordance rate of 88.0% for Gram-negative organisms and 66.7% for Gram-positive organisms. These results reinforce the reliability of the UF-5000 in detecting E. coli and Klebsiella species that comprise the majority of ABP pathogens [3,21]. However, the lower concordance observed for Gram-positive organisms may reflect the limitations of scatter-based signal differentiation in coccoid forms. This challenge has been noted in previous studies [16,22], and future advances in software algorithms or combined molecular approaches may be needed to improve Gram-positive classification accuracy.
Several recent studies have investigated the application of the Sysmex UF-5000 in the broader context of UTI screening [10,12-15]. Kim et al. [13] have demonstrated that the UF-5000 can achieve over 90% accuracy in predicting bacteriuria in outpatient settings, employing cutoff values comparable to those identified in our study . In emergency settings, rapid results from flow cytometry can reduce unnecessary cultures and optimize empiric antibiotic selection [23].
Despite its strengths, this study has several limitations. It was retrospective in nature. In addition, it was conducted at a single center with a relatively small sample size. The low proportion of Gram-positive infections might have limited the assessment of concordance in that subgroup. Moreover, antibiotic use prior to urine sampling was not fully accounted for, potentially affecting both urine culture and UF-5000 results. Lastly, clinical outcomes associated with UF-5000-based decision-making were not assessed, underscoring the need for future prospective studies.
CONCLUSIONS
The Sysmex UF-5000 flow cytometer demonstrated high concordance with standard urine culture in patients already diagnosed with ABP, with the bacterial count parameter showing the strongest correlation. While it does not replace conventional microbiological methods, its ability to provide rapid, quantitative information may support early risk assessment and aid clinical decision-making in suspected cases of ABP particularly in emergency or outpatient settings.
Given the study population included only patients with confirmed ABP, further prospective studies involving a broader spectrum of febrile UTIs are warranted to evaluate the UF-5000’s diagnostic value and its potential role in distinguishing ABP from other UTI subtypes.
Notes
Funding/Support
This study received funding from Sysmex Corporation, which was involved in the study design but had no role in data collection, analysis, or interpretation of the results.
Research Ethics
This study was performed in accordance with ethical principles of the Declaration of Helsinki. It was approved by the Institutional Review Board (IRB) of the Catholic University of Korea (IRB approval number: HC23RIDI0075). Since anonymized and de-identified information was used for analysis, the need for informed consent was waived by the IRB.
Conflict of Interest
The authors have nothing to disclose.
Author Contribution
Conceptualization: JWL, JBC; Data curation: YKH, HIP, JBC; Formal analysis: YKH, HIP, JBC; Methodology: JWL, JBC; Project administration: JWL; Visualization: JBC; Writing - original draft: YKH, JBC; Writing - review & editing: YKH, JWL, JBC.
Supplementary Material
Supplementary Table 1 is available at https://doi.org/10.14777/uti.2550022011.
Supplementary Table 1.
Complete patient characteristics (N=45)
