Hemangioma Mistaken for Renal Cell Carcinoma in a Patient With End-Stage Renal Disease: A Case Report
Article information
Abstract
Hemangiomas are rare, benign vascular neoplasms that are more common in patients with end-stage renal disease. Here, we describe 2 cases of hemangioma misdiagnosed as renal cell carcinoma before renal transplantation. The key finding in our case was the misdiagnosis of hemangiomas as renal cell carcinoma based on computed tomography and magnetic resonance imaging in patients with end-stage renal disease. Because living transplantation was planned for our patients, we performed rapid surgical resection of the heterogeneously enhancing renal masses to avoid delays in transplantation. Our case highlights the importance of rapid surgical resection of enhanced renal masses to confirm diagnosis, thereby avoiding delays in patients scheduled for renal transplantation.
HIGHLIGHTS
This case report presents 2 cases of hemangioma misdiagnosed as renal cell carcinoma prior to renal transplantation. We performed radical nephrectomies of the heterogeneously enhancing renal masses to avoid delay in renal transplantation. Our case highlights the importance of rapid surgical removal of the enhancing renal masses to confirm the diagnosis, thereby avoiding delay in patients scheduled for transplantation.
INTRODUCTION
Although renal cell carcinoma (RCC) is the most common subtype of renal cancer in patients with end-stage renal disease (ESRD), vascular renal tumors are rare [1]. Several cases, however, are reported in patients with ESRD [2]. Although hemangiomas are benign vascular tumors, their radiological findings are similar to those of RCC. Previous studies reported incidental findings of anastomotic hemangiomas in the kidneys and adrenal glands [3-5]. We report 2 cases of hemangioma confirmed by histological examination after nephrectomy, which prevented a delay in the waiting period for living-donor kidney transplantation. The CARE (Consensus-based Clinical Case Reporting) guidelines were followed to conduct this case report.
CASE REPORT
1. Case 1
A 51-year-old male with ESRD undergoing hemodialysis with hemoglobulin 8.8 and creatinine 8.06 was prepared for kidney transplantation. Preoperative contrast-enhanced computed tomography (CT) revealed a 1.2-cm peripheral enhancing nodule in the right kidney (Fig. 1A). Additional magnetic resonance imaging showed a 1.2-cm T2-weighted slight high signal intensity nodule in the interpolar area of the right kidney with no diffusion restriction, no signal drop in the opposed phase, peripheral rim enhancement in the arterial phase, and centripetal enhancement in the portal/delayed phase. This suggested the possibility of renal cancer. Therefore, we planned to perform radical nephrectomy and to postpone the kidney transplantation. Surgery was performed by hand-assisted radical nephrectomy. The histology examination results showed 1.4- × 1.0 cmsized hemangioma, mixed capillary and cavernous type with renal interpolar area. (Fig. 2A and B). Additional immunostaining confirmed CD 31 (+), melanosome (-), CD 31 (-), CK (+), D2-40 (-). After pathology confirmation, the kidney transplantation was successful, with good kidney function and without any tumor recurrence.
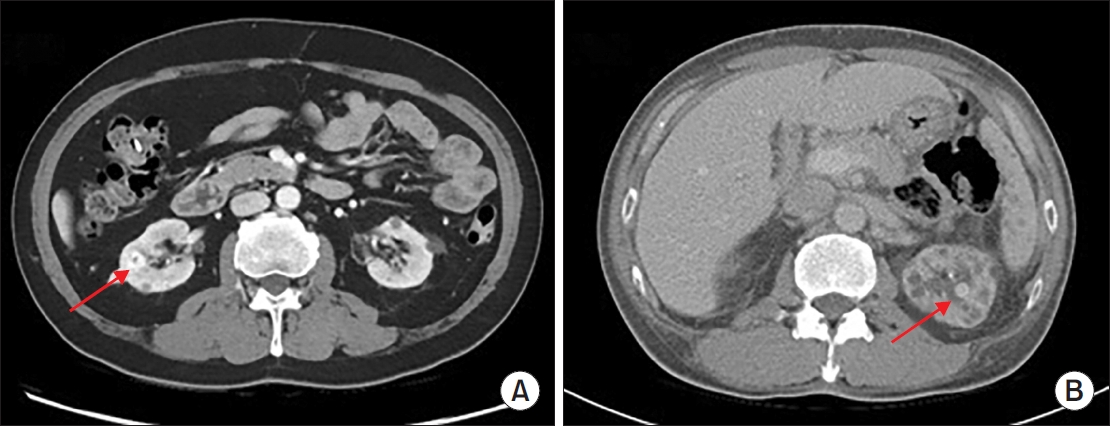
Abdominal computed tomography (CT) shows a 1.2-cm-sized tumor with contrast enhancement (arrow) in the right kidney (A) and a 1.4-cm-sized tumor with contrast enhancement (arrow) in the left kidney (B).
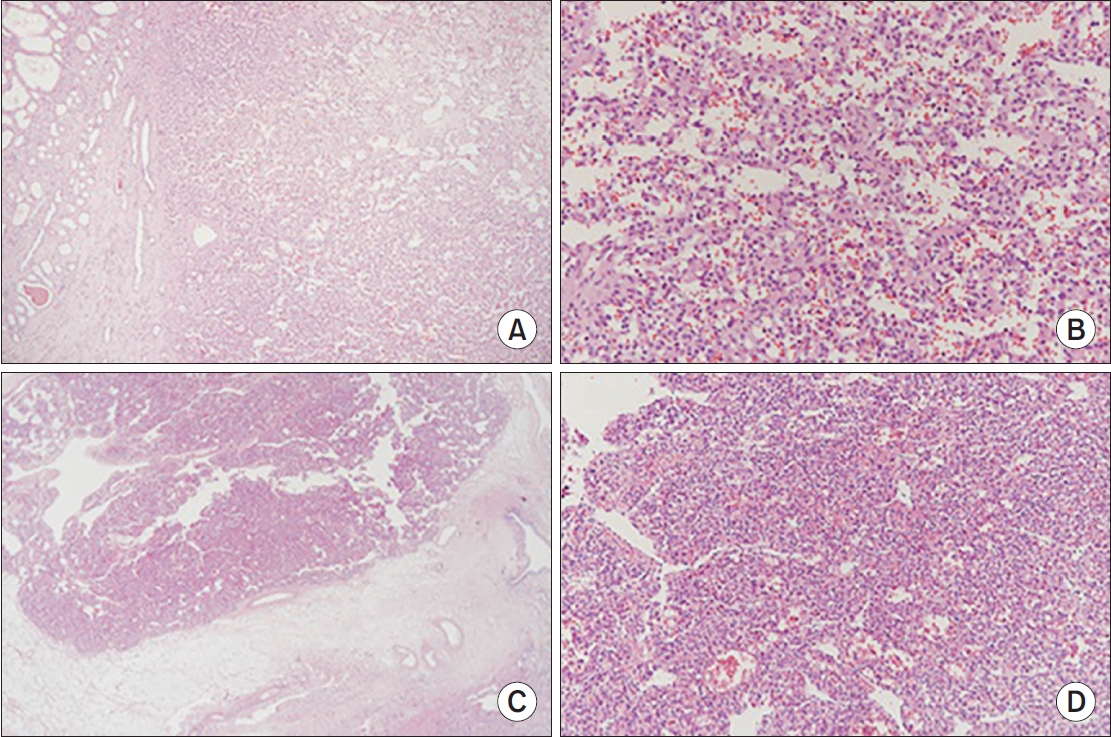
Microscopic features of hemangiomas. Haematoxylin and eosin staining revealed irregularly shaped angiomatous spaces lined with single-layered endothelial cells. Low-magnification (A, ×20) and high-magnification (B, ×100) of case 1. Low-magnification image (C, ×20) and high-magnification image (D, ×40) of case 2.
2. Case 2
A 49-year-old male patient underwent hemodialysis for hypertension, gastric cancer, and chronic renal failure. The patient underwent CT before the kidney transplantation. CT revealed an arterial phase-enhancing lesion, approximately 1.1 cm in sized, at the upper pole of the left kidney (Fig. 1B). Several cysts were observed around these lesions. Therefore, laparoscopic radical nephrectomy was performed first while kidney transplantation was temporarily postponed as in case 1. Biopsy results confirmed capillary hemangioma and polycystic kidney disease (Fig. 2C and D). Immunostaining was SMA (-), ACTIN (-), CD 31 (+), Melanosome (-).
DISCUSSION
Genitourinary hemangiomas are common and benign. Nephrectomy is not clinically indicated for benign vascular neoplasms. ESRD patients with hemangiomas can be immediately enrolled in living-donor kidney transplantation or deceased donor kidney transplantation [6-8]. However, the imaging findings of hemangiomas are similar to those of RCCs, including heterogeneous enhancement of the lesion on CT and hyperintensity on T2-weighted magnetic resonance imaging [9-11]. Subcutaneous biopsy of vascular lesions can be difficult because of the significant risk of bleeding; therefore, in most reported cases, anastomotic hemangiomas are diagnosed via nephrectomy.
Management of renal cancer diagnosed incidentally during medical workups for renal transplantation is controversial. The greatest concern for these patients is unnecessary delay in renal transplantation. Therefore, simultaneous radical nephrectomy and renal transplantation is recommended for these patients. Partial nephrectomy is recommended for small solitary RCCs because of its positive nephron-sparing effects. A recent review reported that the median size of renal hemangioma is 1.5 cm (range, 0.1–8.0 cm), with most hemangioma being <4 cm. According to current guidelines, radical nephrectomy is recommended for these patients for diagnosis or treatment. Several authors have reported cases of successful resection of hemangioma through partial nephrectomy [12,13]. Partial nephrectomy is also a good option for these cases. However, although partial nephrectomy is a procedure to preserve renal function, it was considered that the benefit would not be achieved in patients with ESRD [11]. We performed radical nephrectomy in both cases based on these criteria.
Here, we describe 2 cases of hemangioma misdiagnosed as RCC before renal transplantation. In the first case, a 51-year-old man with ESRD underwent hemodialysis and was scheduled for living-donor kidney transplantation. Preoperative contrast-enhanced CT and magnetic resonance imaging showed a 1.2-cm renal tumor in the right kidney. After radical nephrectomy, staining revealed irregularly shaped vascular spaces of varying sizes. After transplantation, good renal function was achieved and the tumor did not recur. In the second case, a 49-year-old man with ESRD underwent hemodialysis. Pretransplant CT showed a 1.1-cm renal tumor between the cysts in the left kidney. After radical nephrectomy, staining revealed irregularly shaped vascular spaces between the multiple cysts. The radiologic findings of the hemangioma were similar to those of RCC; therefore, pathologic confirmation was required to diagnose hemangioma and avoid delays in registration for renal transplantation. Our case highlights the importance of prompt surgical excision of an enhanced renal mass to confirm diagnosis and avoid delays in patients scheduled for renal transplantation.
Notes
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Research Ethics
This study was approved by the Institutional Review Board (IRB No. 2025-01-015). The patient provided informed consent for publication of this case.
Conflict of Interest
The authors have nothing to disclose.
Author Contribution
Conceptualization: JC; Data curation: JC; Formal analysis: JWL; Methodology: DGL; Project administration: HLL; Visualization: HLL; Writing - Original draft: HLL; Writing - review & editing: DGL, JWL.
