A Narrative Review of Syphilis Notification Systems in Korea: Change to Mandatory Surveillance System
Article information
Abstract
New cases of syphilis are clearly showing an increasing trend worldwide. However, in a sentinel surveillance system, the collection of information on disease outbreaks is limited, making it difficult to understand the overall outbreak situation and perform detailed analyses of patients' demographic characteristics and disease stages. In accordance with the revision of the Infectious Disease Prevention Act, syphilis was converted from a grade 4 infectious disease subject to sentinel surveillance to a grade 3 infectious disease subject to mandatory surveillance from January 1, 2024, with all medical institutions required to report syphilis diagnosis within 24 hours.
HIGHLIGHTS
As of January 1, 2024, in accordance with the revision of the Infectious Disease Control and Prevention Act, syphilis has been adjusted upwards from a level 4 to a level 3 infectious disease and converted to a mandatory surveillance system, obliging all medical institutions to report within 24 hours when syphilis is diagnosed.
INTRODUCTION
Syphilis is a systemic infection caused by transmission of Treponema pallidum mainly through sexual intercourse or vertically through pregnancy [1]. It is largely divided into congenital syphilis and acquired syphilis. Acquired syphilis is further divided into primary, secondary, tertiary, and latent syphilis [2,3]. If syphilis is not properly treated, patients infected with syphilis may exhibit various clinical symptoms [4], which can significantly increase disease morbidity, potentially affecting almost every organ in the body, even leading to death. Untreated maternal syphilis can also lead to fetal death and fatal congenital infection in newborns [5]. For these reasons, the Korea Disease Control and Prevention Agency is making efforts to manage syphilis by operating a national syphilis surveillance system.
CHANGES OF SYPHILIS SURVEILLANCE SYSTEM IN KOREA
The current infectious disease surveillance system is divided into a sentinel surveillance system and a mandatory surveillance system [6]. The sentinel surveillance system refers to the designation of medical institutions to regularly and continuously monitor infectious diseases of relatively low severity. It is difficult to conduct a full investigation for these diseases due to their high incidence rates. In the case of a sentinel surveillance of sexually transmitted infections (STIs), 572 centers, including clinics, hospitals, and public health centers with urology and obstetrics and gynecology services, must report the occurrence of STIs within 7 days of confirmation. Meanwhile, the mandatory surveillance system is operated by mandatory reporting agents such as doctors who report to the local public health center immediately or within 24 hours when a level 1 to 3 infectious disease occurs. This allows epidemiological investigation of individual patients and accurate identification of outbreak patterns.
As seen in the recent case of coronavirus disease 2019 infection, considering social chaos caused by infectious diseases, each country must establish efficient infectious disease control measures for the safety of the people [7,8]. The infectious disease surveillance system used for this cannot always be constant. It must be continuously updated in consideration of the occurrence of new infectious diseases, disappearance of existing infectious diseases, and development of new diagnostic methods. However, frequent changes to a surveillance system have the disadvantage of not being able to identify trends of infectious diseases due to limitations in using data from a previous system. Therefore, the updated surveillance system must be compared to the existing surveillance system to identify advantages and disadvantages and decide whether to maintain and supplement it or return to the previous system.
The syphilis surveillance system for Korea has changed several times over the years. After its introduction in 2001, a sentinel surveillance system was managed for sentinel surveillance until 2010. Following reorganization of a statutory infectious disease classification system in 2010, it was converted to mandatory surveillance until 2019 and the sentinel surveillance system for level 4 infectious diseases was restored from 2020 [9]. However, the incidence of syphilis has recently been increasing in Japan, Taiwan, and China, where surveillance for syphilis is mandatory [10-22]. As human and material exchanges between countries expand, syphilis might become imported into Korea. Thus, there is a need to strengthen the surveillance system and prepare for it in advance.
As of January 1, 2024, in accordance with the revision of the Infectious Disease Control and Prevention Act, syphilis has been adjusted upwards from a level 4 to a level 3 infectious disease and converted to a mandatory surveillance system, obliging all medical institutions to report within 24 hours when syphilis is diagnosed [23]. Due to this process of change, when researchers simply compare syphilis incidence by year, errors in interpreting results may occur due to differences in the number of cases reported by different surveillance systems by year. Thus, results need to be interpreted with caution.
SYPHILIS DIAGNOSIS AND REPORTING
The scope of reporting for syphilis surveillance has been expanded to 5 types, including early latent syphilis which is likely to be transmitted, tertiary syphilis that can progress to a severe disease, and the current 3 types (primary, secondary, and congenital syphilis). When its transition is made to mandatory surveillance, all discovered syphilis cases will be reported, making it possible to objectively investigate the overall incidence of syphilis in the country. Through epidemiological investigations, a wide range of information, including demographic characteristics of individual patients, stage of disease, main symptoms, exposure routes, and contact persons will be collected. More specific measures for syphilis prevention and management are expected to be developed through this. Methods for diagnosing and reporting syphilis are as described below (Fig. 1).
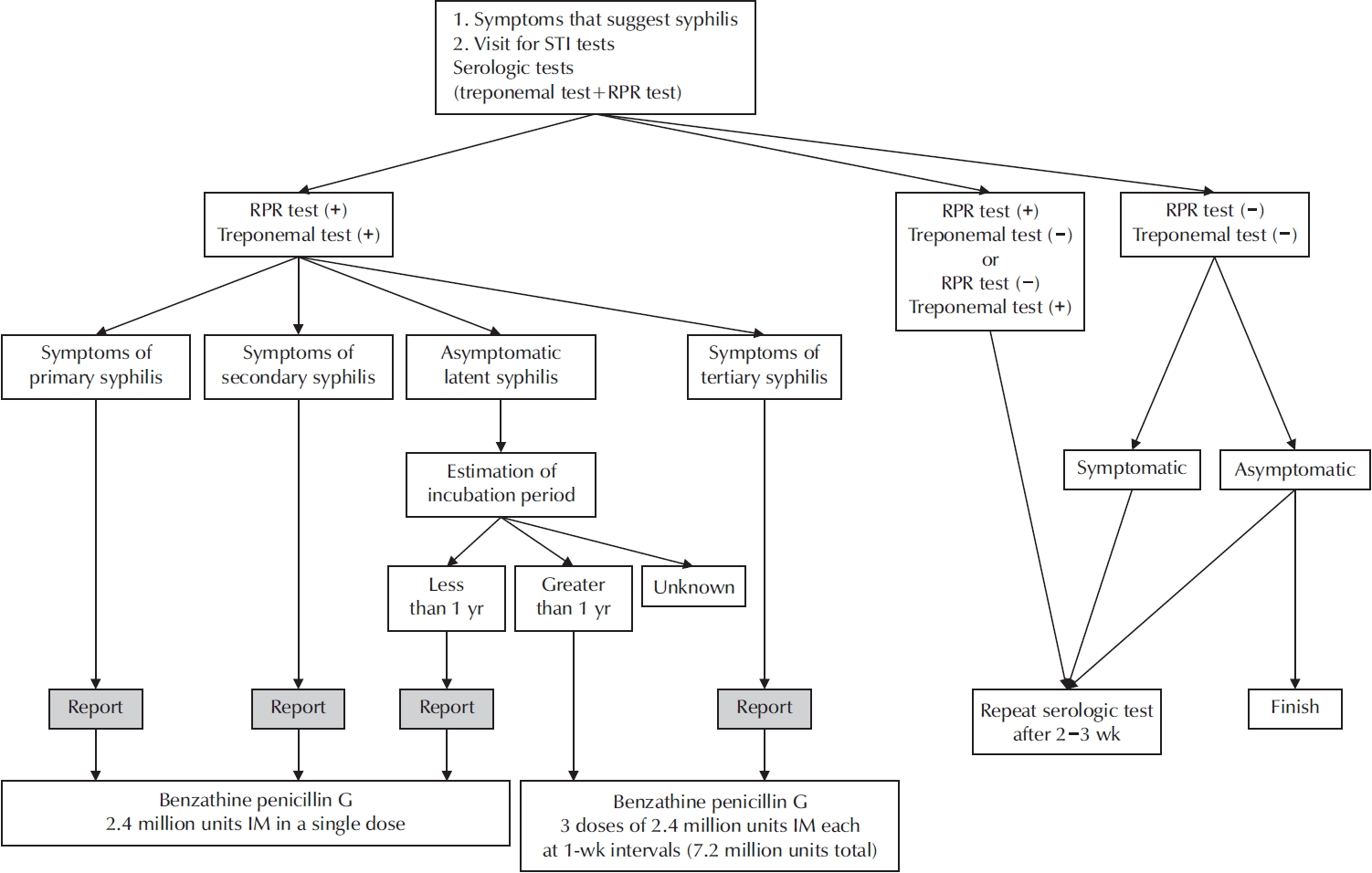
Methods for diagnosing and reporting syphilis. STI, sexually transmitted infection; RPR, rapid plasma reagin; IM, intramuscular injection.
To confirm the diagnosis of syphilis, both treponemal and nontreponemal serological tests must be performed. Treponemal serologic tests (enzyme immunoassays, chemiluminescence immunoassays, T. palidum particle agglutination assay, fluorescent treponemal antibody absorption test, and so on) can be used to detect antibodies to T. palidum antigens by enzyme immunoassay immunofluorescence or particle agglutination. These tests usually remain reactive for most of patients’ lives after treatment, although some people treated in early stages may revert to a serologically negative state [24,25].
Commonly used nontreponemal serologic tests include venereal disease research laboratory (VDRL) and rapid plasma reagin (RPR) tests [25]. The RPR test adds carbon particles to a kit containing aggregated antigens. When antigens aggregate, a black mass is formed. On the other hand, the VDRL test requires the examiner to observe the process of antigen aggregation under a microscope [26,27]. Because an antigen agglutination reaction can be easily confirmed with naked eyes using a kit, more RPR tests are performed. However, when diagnosing neurosyphilis, the VDRL test is used because it has a higher accuracy than the RPR test [28].
Nontreponemal testing reflects disease activity in syphilis. It can be used to determine responses to treatment, recurrence, and/or reinfection. For this testing, it is necessary to dilute the patient's serum and perform a quantitative test (e.g., RPR 1:2 positive, RPR 1:4 positive) [26]. Automated tests that report RPR test results quantitatively without serum dilution have been developed [29]. However, if the antibody titer is high, such as in patients with an early syphilis, the antigen-antibody reaction might be disrupted and the value may actually be low (Prozone phenomenon). Therefore, it is desirable to obtain a quantitative value through serum dilution [30].
CONGENITAL SYPHILIS DIAGNOSIS AND REPORTING
In Korea, we provide support for early detection of congenital syphilis through prenatal examination. Although congenital syphilis is a disease that can be completely cured through early detection and treatment, it still occurs continuously and requires intensive management [5,31,32]. Congenital syphilis infection occurs mainly through the placenta in the uterus, although it can also occur during childbirth in rare cases. Transmission to the fetus during pregnancy can occur at any stage of syphilis [32,33], with the risk being much higher in cases of primary or secondary syphilis, especially if the mother is infected with syphilis in the third trimester of pregnancy [34,35].
Congenital syphilis is generally classified as an early or late congenital syphilis. Early symptoms normally appear within 2 years of life, while late symptoms appear after 2 years of life [25]. Most infants with congenital syphilis show early symptoms. However, some do not show active clinical symptoms at birth or early in life. Fetuses of mothers infected with syphilis are at an increased risk of premature birth and stillbirth. Newborns infected with syphilis may develop symptoms such as hearing loss, hydrocephalus, optic nerve atrophy, and mental retardation [36-38].
Congenital syphilis is diagnosed according to the following criteria. Both confirmed and probable diagnoses have been reported (Fig. 2). Because approximately half of all newborns with congenital syphilis have normal initial tests, any suspicion of active syphilis during pregnancy should be thoroughly investigated. If the mother is at risk for active syphilis, she should be treated and monitored for response to treatment and the newborn should be tested after birth. After birth, both maternal and infant sera are tested simultaneously [39]. Umbilical cord blood should not be used as it might be contaminated by maternal blood [40]. Both treponemal and nontreponemal tests should be performed for both maternal and infant sera. Infant serum treponemal testing should be performed for immunoglobulin M (IgM). This is because immunoglobulin G antibodies are transmitted from mother to fetus through the placenta, whereas IgM antibodies are not transmitted from the mother. Thus, IgM testing should be performed for infant serum trepone-mal testing to determine syphilis infection [38,40,41].
CONCLUSIONS
New cases of syphilis are showing a clear trend of increasing worldwide. However, in a sentinel surveillance system, collection of information on disease outbreaks is limited, making it difficult to understand the overall outbreak situation and perform detailed analyses of patients' demographic characteristics and disease stages. Accordingly, it is important to expand the scope of syphilis surveillance to the entire population, accumulate sufficient statistical data needed for analysis, and identify characteristics and causes of syphilis through epidemiological investigation. Close cooperation between medical staff and the government is needed to end future syphilis outbreaks in Korea.
Notes
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors have nothing to disclose.
Acknowledgments
We appreciate the contributions of our colleagues who assisted in editing this manuscript.
Author Contribution
Conceptualization: SJL, JBC; Visualization: JBC; Writing - original draft: JBC; Writing - review & editing: SJL, JBC.

