Impact of Antibiotics on the Efficacy of Immune Checkpoint Inhibitors in Metastatic Urothelial Carcinoma
Article information
Abstract
Purpose
Emerging evidence has suggested that prior or concurrent antibiotic (ATB) use may be associated with a poor response to immune checkpoint inhibitors (ICIs) in patients with some solid tumors. This study examined the effects of ATB use on the oncological outcomes of patients receiving ICIs for mUC.
Materials and Methods
Patients receiving ICIs for mUC between 2018 and 2020 were assessed retrospectively. Those with over three cycles of atezolizumab or pembrolizumab were included. ATB use, defined as ≥ three days within 60 days before or three months after ICI administration, was compared between groups for oncological outcomes.
Results
Thirty-one patients were examined. The ATB-use and no-ATB-use groups consisted of 15 (48.4%) and 16 patients (51.6%), respectively. The ATB-use group showed a lower disease control rate (56.3% vs. 13.3%, p=0.023) than the no-ATB-use group. The objective response rate in the ATB-use group was lower than the no-ATB-use group, but the difference was statistically insignificant (43.7% vs. 13.3%, p=0.113). The ATB-use group had shorter progression-free survival (median three vs. six months, log-rank p=0.045) and shorter overall survival (median three vs. 14 months, log-rank p=0.023) than the no-ATB-use group. The most commonly used antibiotics were fluoroquinolones (46.7%), cephalosporins (40.0%), non-cephalosporin beta-lactams (6.7%), and nitrofurantoin (6.7%).
Conclusions
ATB may be associated with poorer oncological outcomes in patients with mUC who received ICI therapy. Hence, further research will be needed to understand the relationship between the modulation of ATB-related dysbiosis and gut microbiota composition with the oncological outcomes in patients with mUC.
INTRODUCTION
Urothelial carcinoma (UC) is one of the most common types of malignancy worldwide [1]. Approximately 30% of UC patients have muscle-invasive, advanced, or metastatic disease at the time of diagnosis [2]. Immunotherapy, particularly the use of immune checkpoint inhibitors (ICIs), has become a common treatment option for many solid tumors, including cases of bladder cancer [2].
ICIs that target the programmed cell death-1 (PD-1) protein and programmed cell death-ligand 1 (PD-L1) protein have changed the therapeutic landscape and are currently the standard treatment options in patients with metastatic urothelial cancer [2]. Despite its successful use, the efficacy of ICIs in metastatic urothelial carcinoma (mUC) varies significantly from patient to patient. Standardized and reproducible biomarkers are also clinically important requirements for optimal therapeutic options. On the other hand, the available individual biomarkers do not exhibit sufficient ability and reproducibility to predict the response to ICI-based immunotherapy in a patient. Moreover, the reported effect of immunotherapy alone is only 25-30% [3].
Therefore, for many clinicians, identifying the factors influencing the efficacy of ICIs in tumor immunotherapy is a new challenge that has become a widely discussed topic. Several studies have demonstrated the decisive influences of human gut microbiota on ICI therapies [4,5]. Antibiotics (ATB) alter the diversity and composition of the gut microbiome, which in turn modify their metabolic capacity [6]. Some studies have suggested the possible adverse effects of ATB on anticancer immunotherapy [4]. In large retrospective studies, antibiotic exposure was associated with a reduced clinical benefit of ICIs in renal and lung cancer patients. Such influence could be because ATB cause significant alterations in the gut microbiome. On the other hand, the impact and predictive role of antibiotic exposure in cancer patients receiving immunotherapy remains controversial, and reports pertaining to urological cancers are rare.
The current study hypothesized that the ATB-induced modulation of the gut microbiota may be associated with a poor response to ICIs. Nevertheless, the data on the association between ATB use and the clinical outcomes of ICIs are limited, particularly in Korean patients with genitourinary cancer.
In the present study, a retrospective analysis was performed to examine the influence of ATB on the clinical outcomes of ICI treatment in Korean patients with mUC.
MATERIALS AND METHODS
The clinical data collected from 31 mUC patients treated with ICIs at the Chonnam National University Hwasun Hospital between January 2018 and December 2020 were examined retrospectively. Patients who had received more than three cycles of ICI therapy with either atezolizumab or pembrolizumab were included. Antibiotic use (oral and intravenous) was defined as a minimum of three days of use in the 60 days before ICI administration or a minimum three-day use within the three months before disease progression after ICI administration. The choice of ATB was based on the clinical and radiological focus of the infection at presentation and subsequently modified based on the response and culture reports.
The oncological outcomes of the ATB-use group and the no-ATB-use group were compared. The response was assessed using a radiological methodology according to the Response Evaluation Criteria in Solid Tumors version 1.1. The response assessment was done two or three months after the commencement of ICI therapy or at any symptoms/signs of clinical progression, whichever was earlier.
1. Statistical Analysis
The continuous variables are reported as the mean and standard deviation, and the categorical variables are reported as frequencies (%). Kaplan-Meier curves were generated for the progression-free survival (PFS) and overall survival (OS). A comparison of the PFS and OS among groups was achieved using a log-rank test. The relationships between the groups were compared using a Chi-squared test, Fisher’s exact test, or Student’s t-test. Statistical analyses were performed using SPSS software ver. 23.0 (SPSS Inc.). All p-values were two-sided; the statistical significance criterion was p<0.05.
2. Ethical Approval
The institutional review board (IRB) of the Chonnam National University Hwasun Hospital approved the study protocol (IRB approved protocol: No. CNUHH-2021-094). The study was carried out in accordance with the Declaration of Helsinki and the Ethical Guidelines for Clinical Studies. Patients were not solicited for informed consent, given the retrospective nature of our study. All patient data were processed in anonymity and de-identified prior to analysis.
RESULTS
Thirty-one patients with mUC who received ICI therapy were included. The ATB-use group consisted of 15 patients (48.4%), and the no-ATB-use group had 16 patients (51.6 %).
The mean age was similar in the two groups (75 vs. 72, p=0.936). There were 13 males (86.7%) in the ATB-use group and 11 males (68.8%) in the no-ATB-use group. A comparison of the two groups (ATB-use group vs. no-ATB-use group) revealed 13 patients (86.7%) vs. 11 patients (68.8%) diagnosed with bladder cancer and two patients (13.3%) vs. five patients (31.2%) diagnosed with upper tract urothelial cell carcinoma (UTUCC) (p=0.394). Regarding the PD-L1 parameter, 12 pati-ents (80.0%) were <5% and three patients (20.0%) were >5% in the ATB-use group, whereas nine patients (56.3%) were <5% and seven patients (43.8%) were >5% in no-ATB-use group. The number of patients who used atezolizumab was 15 (100%) in the ATB-use group and 13 (81.0%) in the no-ATB-use group (Table 1).
The disease control rate (DCR) is the percentage of patients with advanced or metastatic cancer who achieved a complete response, partial response, or stable disease as a response to ICI.
The ATB-use group showed a decreased DCR (56.3% vs. 13.3%, p=0.023) compared to the no-ATB-use group (Fig. 1). In the ATB-use group, progressive disease (PD) and partial response (PR) accounted for 86.7% and 13.3%, respectively. By contrast, PD, stable disease (SD), PR, and complete response (CR) accounted for 43.8%, 12.5%, 25.0%, and 19.0%, respectively, in the no-ATB-use group.

Best overall response to immune checkpoint inhibitor therapy. The antibiotics (ATB) use group showed an inferior disease control rate (56.3% vs. 13.3%, p=0.023) to the no ATB use group. PD: progressive disease, SD: stable disease, PR: partial response, CR: complete response.
The overall response rate (ORR) is defined as the proportion of patients with a partial or complete response to therapy; it does not include stable disease and is a direct measure of the tumoricidal activity of a drug. The ORR in the ATB-use group was lower than the non-ATB-use group, but the difference was statistically insignificant (43.7% vs. 13.3%, p=0.113).
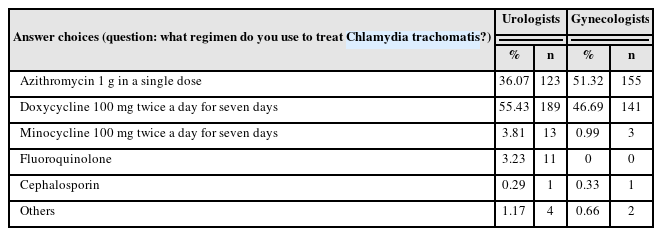
The ATB-use group had shorter PFS (median three vs. six months, log-rank p=0.045) and shorter OS (median three vs. 14 months, log-rank p=0.023) (Fig. 2). The PFS and OS were similar in the two groups. The most commonly used ATB were fluoroquinolones (46.7%), cephalosporins (40.0%), non-cephalosporin beta-lactams (6.7%), and nitrofurantoin (6.7%) (Table 2).

Progression-free survival (A) and overall survival (B) in patients with metastatic urothelial carcinoma treated with immune checkpoint inhibitors (ICIs) therapy according to antibiotics use.
DISCUSSION
Several studies have suggested that antibiotic use can have a significant impact on the immunotherapeutic outcomes of cancer patients. Some studies reported that the use of ATB has a negative effect on clinical outcomes in patients with non-small cell lung cancer (NSCLC), renal cell carcinoma (RCC), or melanoma who were treated with ICIs [7]. On the other hand, the impact and predictive role of antibiotic exposure in cancer patients receiving immuno-therapy remains controversial, and reports pertaining to urological cancers are rare.
This study examined whether ATB influence the treatment outcome of mUC patients treated with ICIs. The ATB were used to treat urinary tract infection or neutropenic fever, or as a prophylactic before urologic procedures (e.g., percutaneous nephrostomy and ureteral stent insertion). The present study revealed poorer survival in patients who received ATB during ICI. Therefore, antibiotic treatment for cancer patients can be a negative prognostic factor of ICI therapy.
T-lymphocytes are central regulators of the adaptive immune system response, which play an important role in detecting and eliminating cancer cells. T-cell activation relies on a second costimulatory or coinhibitory signal provided by additional surface molecules of antigen-pre-senting cells and occurs in a series of steps. PD-1, PD-L1 (PD-1 ligand), and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) are all coinhibitory molecules, which act as immune checkpoints that weaken the immune response to prevent autoimmune diseases. On the other hand, coinhibitory ligands and receptors are often overexpressed on cancer and stromal cells within the tumor microenvironment, so they help cancer cells avoid immune-mediated destruction [8]. Monoclonal antibodies against CTLA-4, PD-1, and PD-L1 are ICIs that help release the patient’s immune responses against the tumors.
The patients’ response to ICIs varies widely from individual to individual [9]. The efficacy of ICIs appears to be related to the patient’s gut microbiome, which interacts closely with the immune system.
In 2015, Sivan et al. [10] published the first study on the association between the treatment efficacy of ICIs and the gut microbiome composition. The effectiveness of tumor immunotherapy can be enhanced by beneficial gut microbiome composition [11]. A study using a mouse model reported that the efficacy of ICI therapy on tumors was reduced when the gut microbiome composition, such as the presence of Bacteroides fragilis, was disrupted. Routy et al. [12] analyzed 249 cancer patients treated with ICIs and found that the proportion of Akkermansia muciniphila in the microbial composition was high in cancer patients responding well to ICIs. Moreover, the OS and PFS of patients who received ATB were shorter than those who did not [12]. According to a study that analyzed the gut microbiome, the clinical benefit of anti-PD-1/PD-L1 therapy correlated with Bifidobacterium, Akkermansia muciniphila, and Rumino-coccaceae, and the clinical benefits of anti-CTLA-4 therapy was associated with B. fragilis, B. thetaiotaomicron, and Burkholderiales [13].
The advent of new high-throughput microbiologic techni-ques, such as DNA sequencing, has shown that antibiotic treatment impairs the composition and functioning of the human microbiome [14]. Disturbances in the gut microbiota associated with antibiotic use have been shown to promote conditions such as obesity, diabetes, inflammatory bowel disease, allergies, and asthma [15,16].
The use of broad-spectrum ATB can reduce the proportion of Bifidobacterium (Actinobacteria), Alistipes (Bactero-idetes), and four genera from the phylum Firmicutes (Faecalibacterium, Oscillospira, Ruminococcus, and Diali-ster). Some of these gut microbiotas are important for immunotherapy. The gut microbiome requires approxi-mately four weeks to recover sufficiently after antibiotic exposure [6]. In general, ATB clinically disrupt the gut microbiota, and the link between ATB and immunotherapy efficacy has been a contested topic in recent years [17-19].
Nevertheless, the overall effect of ATB on the survival of cancer patients receiving ICI treatment is unclear because the actual effect of ATB does not match the effects of ICIs [20]. This study examined the effects of antibiotic use on ICI treatment outcomes in patients with mUC to solve the above clinical problems. The first retrospective study attempting to determine the effects of ATB on the clinical efficacy of PD-1 or PD-L1 blockade (second-line or higher) included 249 patients with NSCLC, RCC, and UC [21]. In a recent single-site retrospective study that enrolled 291 cases of advanced cancer, Tinsley et al. [22] reported that, as an independent prognostic factor, antibiotic treatment adversely affected the PFS and OS in patients treated with ICIs. Subgroup analysis showed that patients who continued to receive antibiotic treatment had poorer clinical outcomes than other patients [22]. On the other hand, Sen et al. [23] found that administering ATB during or before ICI therapy was not associated with PFS in patients with advanced cancers and that only antibiotic administration within 30 days of the onset of ICI therapy had a negative effect on the OS. According to a recent meta-analysis, the worse OS (hazard ratio [HR], 1.76; 95% confidence interval [CI], 1.41-2.19; p<0.00001) and PFS (HR, 1.76; 95% CI, 1.47-2.12; p<0.00001) were significantly correlated with the admini-stration of ATB [24]. In addition, the most negative effect was reported when ATB were used within six weeks of starting immunotherapy [25].
The factors that influence the prognostic role of ATB include a variety of other factors, such as the reason for antibiotic use, type of antibiotic, type of administration, duration of treatment, and single or multiple drug combi-nations. Ciprofloxacin had a significant and highly reversible effect on the gut microbiota, whereas nitrofurantoin had minimal effects. The effects of ciprofloxacin on the gut microbiota composition persist for approximately one month after treatment [6]. Nitrofurantoin is characterized by good absorption from the small intestine, rapid excretion via the kidneys, and inactivation in most body tissues [26]. This explains the slow emergence of resistance and minimal collateral damage caused by nitrofurantoin [27,28]. In contrast, even a single dose of ciprofloxacin results in high fecal concentrations of the active drug [29,30]. Therefore, ATB that cause less collateral damage, such as nitrofurantoin, are more appropriate for patients requiring immunotherapy than broad-spectrum ATB, e.g., ciprofloxacin. Nevertheless, more research is needed in this area.
The study findings support a poor prognosis when antibiotic-exposed cancer patients are treated with ICIs. Nevertheless, this study had several limitations. First, it was a retrospective study conducted at a single tertiary-care center in a specific region of Asia. Second, the duration and type of antibiotic used may have caused differences in the urinary tract microbiome. Third, the study was conducted with a relatively small group of patients. A larger group will be needed to obtain more accurate results. On the other hand, this study is valuable because statistically significant results were derived for mUC. Further research will determine the correlation between ATB and immuno-therapy for other kinds of urological cancer.
CONCLUSIONS
The use of ATB may be associated with poorer oncological outcomes in patients with mUC who receive ICI therapy. Further research will be needed to understand the relationship between modulation of ATB-related dysbiosis and gut microbiota composition with the oncological outcomes in patients with mUC.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This study was supported by a Grant (HCRI 22003) from the Chonnam National University Hwasun Hospital Institute for Biomedical Science.
AUTHOR CONTRIBUTIONS
S.I.J. participated in research conception and design. H.Y.L., S.I.J. participated in data acquisition. E.C.H., S.I.J. participated in data analysis and interpretation. E.C.H. participated in statistical analysis. H.Y.L., S.I.J. participated in manuscript writing. D.G.L., H.S.C., E.C.H., and D.D.K. participated in review and editing. All authors approved the final manuscript.