Differences in Urine Microbiome of Acute Cystitis and Chronic Recurrent Cystitis in Women
Article information
Abstract
The diagnosis of urinary tract infection (UTI) relies on urine culture tests to identify aerobic or anaerobic urinary tract pathogens. This method has limitations in identifying anaerobic bacteria, and there is uncertainty in identifying all bacteria. A new next-generation sequencing (NGS) method has gradually helped overcome these limitations, and the microorganisms present in the human urinary tract are gradually being revealed. This review introduces studies on the microbiome analyzed using NGS of urine from patients with acute cystitis and recurrent UTIs and discusses whether NGS may reveal the pathophysiology of the disease.
INTRODUCTION
Urinary tract infection (UTI) is one of the most common infections, with more than 150 million patients yearly [1]. Women have six times the incidence of UTI than men and a 50% or more chance of experiencing UTI during their lifetime [2]. In patients who had a UTI once, 20–40% experience recurrence, including 25–50% of these patients who will have repeated recurrence [3,4].
Acute uncomplicated cystitis, the most common type of UTI, is characterized by inflammation of the lower urinary tract by a specific pathogen, showing symptoms in the lower urinary tract. The disease is diagnosed based on the presence of pyuria in the urine test or culture of urinary tract pathogens in the urine culture test. Acute uncomplicated cystitis has a relatively well-established diagnosis and treatment and shows a good response to treatment, notwithstanding the problem of increased antibiotic resistance over time. On the other hand, in recurrent UTIs, the causative bacteria are often not identified accurately in traditional urine culture tests. In particular, there is no standard treatment in cases of negative urine culture tests [5]. As a result, patients with recurrent UTIs suffer from decreased quality of life due to repeated symptoms, increased antibiotic resistance after frequent use of antibiotics, and increased medical costs.
When a patient visits the hospital for symptoms, urine and culture tests are performed. Once the results show findings of pyuria or bacteriuria, the general treatment involves the prescription of antibiotics. If the patient satisfies the diagnostic criteria for recurrent UTI, it is generally recommended to investigate the causative factor. On the other hand, in tertiary medical institutions, most cases show no improvement after antibiotic treatment at primary and secondary hospitals. Although some patients show improvement in symptoms, the patients visit tertiary hospitals to find the cause and correct or prevent recurrence. In the former case, urine and urine culture tests at tertiary institutions show no abnormal findings, which lead to confusion in treatment. No specific causative factor is often identified in the latter, even after various tests. As a result, it is often difficult to determine if the patient is diagnosed with recurrent UTI or another non-infectious disease, such as bladder pain syndrome. In particular, medical personnel face challenges in suggesting an adequate solution to patients with no specific causative factors and who experience frequent recurrence of UTI. Moreover, the medical personnel question whether it is correct to define the frequent recurrence of acute cystitis as recurrent UTI according to the current diagnostic criteria or the underlying pathophysiology of the two diseases is the same. There may be clear differences in the urine and urinary tract of patients with recurrent uncomplicated cystitis and patients with recurrent UTI, which might be due to the differences in the immune system or urine microbiome, in addition to the anatomical vulnerability of the host.
The diagnosis of UTI relies on urine culture tests to identify aerobic or anaerobic urinary tract pathogens. On the other hand, there are limitations in identifying anaerobic bacteria and uncertainty in identifying all bacteria [6,7]. A new next-generation sequencing (NGS) method has gradually helped overcome these limitations, and microorganisms present in the human urinary tract are gradually being revealed [8].
This review introduces studies on the microbiome analyzed using NGS of urine from patients with acute cystitis and recurrent UTIs and discusses whether NGS may reveal the pathophysiology of the disease.
MAIN BODY
1. Urine Microbiome of Healthy Individuals
The Human Genome Project from 1990 to 2003 completed the analysis of the human DNA sequence [9], which was expected to contribute greatly to the identification and treatment of diseases. On the other hand, the human DNA sequence was much simpler than expected, with approximately only 20,000 genes, a number similar to that of fruit flies. Furthermore, there were limitations in explaining the complex physiological and pathological mechanisms of humans only by identifying the human genes. As a result, after the completion of the Human Genome Project, the concept of "superorganisms" emerged, which involved understanding the various wholes, including microorganisms and their genes existing or coexisting in the human body, as a single life phenomenon [10]. Subsequently, in 2008, the Human Microbiome Project was started in the U.S. to identify the genetic list of microorganisms in the human body. As a result, studies on the microbiome were published in Nature in 2010 and Science in 2012. In 2015, a special edition on the microbiome was published in Nature. In 2016, Nature Microbiology was established, suggesting that the microbiome is a key topic of interest in medicine and biology. Through many studies, the human microbiome plays a role in the absorption of nutrients, regulation of drug metabolism, regulation of the immune system, regulation of brain/behavioral development, and prevention of infectious diseases in the human body.
Unfortunately, the Human Microbiome Project did not include the urinary tract and the bladder for two main reasons. First, urine has been traditionally misunderstood as being sterile until it reaches the urethra, as conventional culture techniques did not detect any microorganisms. Following the development of molecular biology technology, 16S rRNA sequencing revealed numerous microorganisms in the urine from the bladder [11-13]. Second, the urine passes through the urethra for excretion from the body. In this process, the urine is contaminated by the urethral flora. Hence, it does not accurately reflect the microbiome of pure urine in the bladder. As a result, urine had to be collected directly from the bladder through a clean catheter or puncture of the suprapubic region, which was limited in healthy patients for ethical reasons.
Although the urinary tract system was not included in the Human Microbiome Project, studies on the urine micro-biome using NGS are increasingly performed with more diverse findings. When the fundamental reference values for the urine microbiome of healthy individuals are completed, studies on the urine microbiome of patients with diseases may be subsequently conducted, which can change the paradigm of the understanding of disease pathophysiology. Nevertheless, for the reasons described previously, only a limited number of studies investigated the urine microbiome of healthy people (Table 1) [6,11-20]. The studies had different gender of patients, sample sizes, urine collection methods, and techniques. Despite this, lactobacillus and streptococcus were commonly reported in all studies. These two microorganisms are lactic acid bacteria found in the genitourinary system and other parts of the body with well-known roles in protection against pathogens [21].
2. Urine Microbiome of Patients with Acute Uncomplicated Cystitis
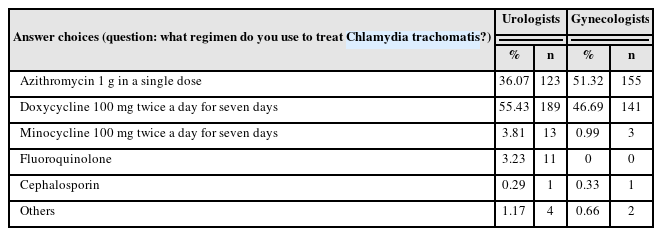
Acute uncomplicated cystitis is a sudden inflammatory condition of the bladder mainly caused by uropathogenic Escherichia coli (UPEC) or other Enterobacteriaceae [22]. According to standardized culture-dependent diagnostic tests reported over several decades, acute cystitis infections are caused mainly by gram-negative bacteria, and UPEC is responsible for approximately 80% of all acute cystitis in women aged 18–39 years. Other infections are caused by different members of Enterobacteriaceae and some gram-positive bacteria, such as Staphylococcus, Enterococcus, and Streptococcus. Furthermore, Mycoplasma species, Candida species, and Trichomonas vaginalis are also causative strains of cystitis [23,24]. Table 2 lists six studies on the urine microbiome of patients with acute uncomplicated cystitis [25-29].
3. Urine Microbiome of Patients with Recurrent UTI
In 2021, a study analyzed the urine microbiome of patients with recurrent UTI and acute uncomplicated cystitis [30]. Adult female patients diagnosed with cystitis were divided into two groups by the recurrence of cystitis, and urine culture test and the NGS results were compared between the two groups. Urine culture tests showed positive findings in seven out of 42 patients (16.7%), and NGS detected microorganisms in 29 out of 42 patients (69.0%), showing high sensitivity. This was consistent with other studies, in which urine culture tests showed a high false-negative rate of 70–90%, and NGS for urine analysis had a false-negative rate of less than 20% [6,19,31]. Urine NGS showed a higher sensitivity than conventional urine culture tests in both groups. On the other hand, urine NGS had a higher sensitivity in the acute uncomplicated cystitis group than in the recurrent cystitis group (72.7% vs. 67.7%, p=0.094). This suggested potential differences in the bacterial diversity and microbiome patterns between the two groups. The high sensitivity of NGS in recurrent UTI may help identify anaerobic or atypical bacteria that are normally not identified in urine culture tests, and as NGS is not significantly affected by the use of antibiotics, it may be a useful tool for the treatment of patients with recurrent UTI in tertiary hospitals. In addition, the results of NGS can be obtained relatively quickly within 24 hours compared to existing urine culture tests which often require three to four days of culture period.
Alpha diversity analysis was used to determine the distribution of different microorganisms present in a sample (Fig. 1). The microbiome diversity measured by the Shannon index was significantly higher in the recurrent UTI group than in the acute uncomplicated cystitis group (p=0.007). The beta diversity was assessed using weighted UniFrac distances to determine if the two groups had different microbial communities. The findings showed that the two groups had significantly different microbiome compositions (p=0.004) (Fig. 1). After analyzing the diversity, the differences in specific microbial genera were assessed between acute uncomplicated cystitis and recurrent UTI. Fig. 2 shows the relative abundance of the top 100 microbial species in a heat map. Single strains were detected predominantly in the acute uncomplicated cystitis group. This observation contrasted with the recurrent UTI group that showed various species in addition to Enterobacteriaceae. The results were analyzed according to the ratio of the species detected in each group (Fig. 3). Proteobacteria and Gammaproteobacteria were detected more frequently in the acute uncomplicated cystitis group than in the recurrent UTI group. On the other hand, Phylum Bacteroidetes, Class Bacteroidia, Order Bacteroidales, Family Prevotellaceae, and Phylum Firmicutes were detected at higher rates in the recurrent cystitis group than in the acute uncomplicated cystitis group.

(A) Pairwise alpha diversity com-parisons of urine microbiota between two cystitis groups. Boxplot of Shannon index shows significant differences between two cystitis (p=0.007). (B) Principal coordinate analysis of the urine microbiota based on weighted UniFrac distances between two cystitis groups shows significant differences in the microbial composition. Adapted from the article of Yoo et al. J Clin Med 2021;10:1097 [30].

LEfSe analysis showing the bacterial taxa that were significantly different in abundance between the two cystitis groups. The taxa enriched in the acute uncomplicated cystitis group are shown in red with negative linear discriminant analysis (LDA) scores, and the recurrent cystitis group is shown in green with positive LDA scores. Adapted from the article of Yoo et al. J Clin Med 2021;10:1097 [30].
Lastly, probable urinary tract pathogens found in urine culture tests and urine NGS were summarized (Table 3). In the urine culture test, E. coli was the main urinary tract pathogen detected in the acute uncomplicated and recurrent cystitis groups. In urine NGS, in addition to E. coli, Pseudomonas, Acinetobacter, Bradyrhizobium, and Enterobacteriaceae were detected in the acute uncomplicated cystitis group. In contrast, Sphingomonas, Staphylococcus, Streptococcus, and Rothia were also identified in the recurrent cystitis group.
When associating these findings with treatment, simple acute cystitis should be treated promptly with antibiotics. In cases of recurrent cystitis, antibiotic use needs to be carefully decided. In particular, in patients with recurrent cystitis, inadequate use of antibiotics without proper identification of the causative bacteria may worsen dysbiosis.
Recently, studies have also investigated microbiome regulation to reduce dysbiosis. In some studies, probiotics improved UTI, but there is a lack of appropriate evidence [32,33]. In addition, recurrent UTI was reportedly improved after fecal transplantation in kidney transplant patients [34]. A recent study reported that Lactobacillus has protective effects against urinary tract pathogens limited to women [35].
CONCLUSIONS
Acute uncomplicated cystitis and recurrent UTI have different microbiome diversity and patterns. Hence, the two conditions must be approached from different perspectives. Increased microbiome diversity was only observed in the recurrent UTI group and may be associated with recurrent UTI. Acute uncomplicated cystitis can be viewed as a transient infection caused by a specific causative organism. In contrast, dysbiosis plays a more critical role in the pathophysiology of recurrent UTIs.
FUNDING
No funding to declare.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.