Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
Article information
Abstract
Purpose
This study aimed to determine the treatment modality for prostatic abscesses according to size.
Materials and Methods
Twenty-five patients diagnosed with prostatic abscesses were retrospectively reviewed. All patients were treated with intravenous empirical and appropriate antibiotics according to culture results. They were grouped according to the size of the prostate abscess based on computed tomography results (group A, with prostate abscess ≤2 cm, n=10; group B, with prostate abscess size >2 cm, n=15), and their treatment modality and outcomes were compared.
Results
The prostatic abscess sizes were 1.31±0.37 and 3.49±1.06 cm for groups A and B, respectively. Prostate-specific antigen, prostatic volume, and comorbidity were not significantly different (p>0.05), whereas pelvic pain was significantly different (p=0.028). There was no difference in the microorganisms isolated from urine and blood culture, empirical antibiotics, and broad-spectrum antibiotics between the two groups (p>0.05). More patients in group B underwent transurethral abscess deroofing than those in group A (p=0.040). Patients in group B had a more extended hospitalization period and intravenous antibiotics duration than those in group A (p=0.024 and p=0.013, respectively). Group B had more cases of septic shock, intensive care unit admission, and mortality events than group A (p=0.024, p=0.001, and p=0.061, respectively). However, prostatic abscess recurrence and urological chronic complication did not significantly differ (p>0.05).
Conclusions
Appropriate use of antibiotics is crucial. This study shows that the treatment of patients with prostatic abscess >2 cm is more difficult, but transurethral abscess deroofing can lower mortality, prostatic abscess recurrence, and urological chronic complications.
INTRODUCTION
Prostate abscess is known to occur in 2% to 18% of patients with acute prostate infections without insufficient treatment [1,2]. Prostate abscess should be suspected if fever does not subside within 48 hours after a diagnosis of acute prostate inflammation and administration of appropriate empirical antibiotics. It is common in patients with immunodeficiency such as those with diabetes mellitus or human immunodeficiency virus infection, and risk factors include the previous use of catheters and history of urinary tract intervention such as prostate biopsy or surgery, old age, and comorbidities. Prostate abscesses are also found in patients diagnosed with abscesses of other organs, such as the lungs or liver [3-5]. The most common microbial strain in acute febrile prostate infections accompanied by prostate abscess is Escherichia coli. Infections due to Klebsiella pneumoniae and Pseudomonas aeruginosa have also been reported [1,5,6].
Fever and chills, voiding difficulties, lower urinary tract symptoms, and pelvic pain represent the majority of symptoms, accounting for 30 to 72%, 30%, 96%, and 20%, respectively. Prostate abscesses should be carefully differentiated from other lower urinary tract diseases because the symptoms extensively overlap [5]. A prostate abscess should be suspected when fluctuations are observed in the prostate on digital rectal examination. In addition to the aforementioned clinical judgment, a prostate abscess should also be suspected if hypoechoic shadows are observed on transrectal ultrasonography or low-density shadow lesions with rim enhancement on abdominal computer tomography (CT) scan, respectively [7-9].
To date, the three main treatment modalities for prostate abscess are appropriate antibiotic treatment, percutaneous drainage intervention, and prostate abscess drainage surgery [2,10]. With the introduction of transurethral abscess deroofing in the 1970s, the mortality rate from prostate abscess has decreased to 3-16% [11]. However, so far, the treatment modality for a prostate abscess is determined based only on clinical experience and a small number of clinical studies. Conservative management is only recommended for prostate abscess <1-2 cm, and appropriate antibiotics are administered based on complex urinary tract infections. Very few studies have analyzed the prognosis and treatment outcomes for prostate abscess >2 cm [1,11-14].
Thus, this study aimed to analyze the clinical characteristics of patients according to the size of the prostate abscess and to investigate the effectiveness of surgical drainage along with the administration of appropriate antibiotics.
MATERIALS AND METHODS
From April 2016 to October 2020, we retrospectively analyzed the medical records of 25 patients diagnosed with prostate abscesses and hospitalized. After obtaining approval from the Institutional Review Board (IRB number: 2210-012-119) of Pusan National University Hospital, we performed a retrospective chart review of data from all patients diagnosed with prostatic abscesses. All patients underwent blood and urine culture tests, and empirical antibiotics such as third generation cephalosporins (ceftriaxone or cefotaxime), fluoroquinolones (ciprofloxacin or levofloxacin), and/or carbapenems (ertapenem, meropenem, or imipenem) were injected intravenously. Antibiotics such as piperacillin/tazo-bac-tam, cefepime, and vancomycin were added or changed depending on the patient’s clinical features or culture test results [3-5,15]. If necessary, a request for consultation was made to the Department of Infectious Diseases and/or other departments.
An abdominal CT scan was performed to diagnose prostate abscesses in all patients. The length of the long axis of the prostate abscess was measured in the coronal and transverse sections, and the patients were divided into two groups according to the size of the prostate abscess: groups A and B included patients with prostate abscess size ≤2 cm and >2 cm, respectively. Based on medical records, age, comorbidity, urinary tract diversion method, blood test results, urine and blood culture test results, antibiotics change, intravenous or enteral antibiotic duration, intervention or surgery history, hospital day, event of septic shock and intensive care unit admission, mortality, recurrence of prostate abscess, and urological chronic complications (urinary incontinence, dysuria, chronic pelvic pain syndrome, etc.) were investigated.
Percutaneous catheterization was maintained in patients who underwent the procedure for 7 days, and the catheter was removed when it was no longer draining. All patients who underwent surgery underwent transurethral prostate abscess drainage using holmium laser (VersaPulse PowerSuite; Lumenis, Yokneam, Israel) and a 500-mm end-fire laser fiber (SlimLine 550; Lumenis). After the operation, the urethral catheter was maintained for 48 hours and then removed after uroflowmetry and post-void residual volume testing.
Statistical analysis was performed using SPSS version 27 (IBM Corp., Armonk, NY, USA). After performing the normality test on continuous variables, the student t-test was performed if normality was observed, and the Mann–Whitney U-test was performed if there was no normality. For nominal variables, the chi-square test and Fisher's exact test were performed. A p-value <0.05 was considered statistically significant.
RESULTS
Table 1 presents the patients’ characteristics. The average age of the patients did not significantly differ between the two groups (p=0.452). Meanwhile, the average size of the prostate abscess significantly differed between the two groups (p=0.0001). There were no significant differences in white blood cell count, absolute neutrophil fraction, absolute neutrophil count on complete blood count, C-reactive protein, prostate-specific antigen, and prostate size (p>0.05). The numbers of patients with diabetes, comorbidities other than diabetes, and previous urological procedures or surgery did not significantly differ between the two groups (p=0.688, p=0.345, and p>0.999, respectively). In group B, pelvic pain was significant (p=0.028), but there was no significant difference in voiding difficulties or lower urinary tract symptoms (p=0.358 and p=0.122, respectively). There was no statistical difference between the two groups in the rates of urethral catheterization and suprapubic cystostomy insertion performed for urinary tract diversion (p=0.345 and p=0.626, respectively). There was one case of consultation with another department in group A, whereas 11 consultations were requested in group B (p=0.004) (Table 1).
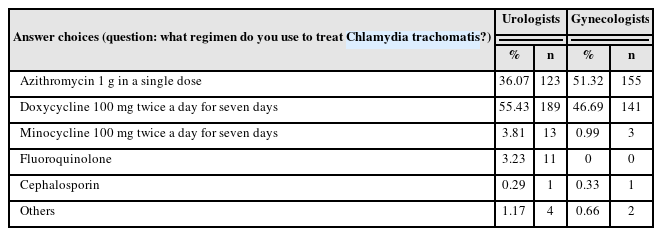
The microorganisms isolated from urine and blood cultures are shown in Table 2. In the urine culture test in group A, 70.0% (7/10) of the patients had no isolated strain, and the remaining patients had K. pneumoniae (10%, 1/10), E. coli (10%, 1/10), and P. aeruginosa (10%, 1/10). In the urine culture test in group B, 53.3% (8/15) of the patients had no isolated strain, and the remaining patients had K. pneumoniae (26.7%, 4/15), E. coli (6.7%, 1/15), P. aeruginosa (6.7%, 1/15), and Pseudomonas otitidis (6.7%, 1/15). In the blood culture test in group A, 90.0% (9/10) of the patients had no isolated strain and 10.0% (1/10) had K. pneumoniae. Meanwhile, in group B, 40.0% (6/15) of the patients had no isolated strain and 33.3% (5/15) had K. pneumoniae, 6.7% (1/15) had P. aeruginosa, and 6.7% (1/15) had P. otitidis.
The treatment modalities and outcomes are presented in Table 3. As for empirical antibiotics, third generation cephalosporins, fluoroquinolones, and carbapenems account-ed for 50.0% (5/10), 10.0% (1/10), and 40.0% (4/10), respectively, in group A, whereas they accounted for 60.0% (9/15), 20.0% (3/15), and 20.0% (3/15), respectively, in group B. In patients who were given empirical antibiotics that were maintained until discharge, cephalosporins, fluoroquinolones, and carbapenems accounted for 50.0% (7/14), 25.0% (1/4), and 100% (7/7), respectively. Broad-spectrum antibiotics were administered to 40.0% (4/10) of the patients in group A and 40.0% (6/15) of the patients in group B. Transurethral prostate abscess drainage was performed in two (20.0%) of 20 cases in group A and 12 (80.0%) of 15 cases in group B (p=0.040). Percutaneous drainage was performed in only one (10.0%) of 10 cases in group A.
The duration of hospitalization and intravenous antibiotic use significantly differed between the groups, with longer durations in group B (p=0.024 and p=0.013, respectively). Meanwhile, septic shock, intensive care admission, and mortality were reported in group B only, with septic shock showing a significant difference between the two groups (p=0.001). There was no recurrence of prostate abscess or urological chronic complications in either group (Table 3).
The use of broad-spectrum antibiotics accounted for 40.0% (10/25) of all patients. Table 4 shows the size of the prostate abscess, isolated microorganisms and the antibiotic susceptibility on urine and blood culture, and clinical features of 10 patients. Among them, four patients were started on a third-generation cephalosporin as an empirical antibiotic and then switched to carbapenems; of these patients, one (patient 17) had a pelvic fracture surgery and another (patient 21) showed susceptibility in culture result from the liver abscess aspiration, and their antibiotics were changed to cefepime (Table 4). Three patients were started on a third-generation cephalosporin as an empirical antibiotic and then switched to piperacillin/tazobactam. Two patients were started on fluoroquinolone as an empirical antibiotic; after extended-spectrum beta-lactamase–posi-tive E. coli was identified in patient 4, the antibiotic was changed to carbapenem; meanwhile, patient 16 showed susceptibilities to all antibiotics for Staphylococcus aureus in culture but was in the intensive care unit due to coronary occlusive disease and continued to show unstable vital signs; thus, a combination of carbapenem and vancomycin was administered based on clinical judgment. Moreover, patient 19, who had a concomitant lung abscess, was started on piperacillin/tazobactam and fluoroquinolone as empirical antibiotics. However, septic shock persisted, and he died despite the co-administration of carbapenem and vancomycin.
DISCUSSION
This study evaluated the clinical characteristics among patients according to the size of prostate abscesses and investigated the effectiveness of surgical drainage along with the administration of appropriate antibiotics. As seen in the cases in this study, prostate abscess is a severe urological disease that can lead to septic shock or death even with appropriate treatment after diagnosis. Therefore, when a prostate abscess is clinically suspected, abdominal CT or transrectal ultrasound should be performed at an early stage to quickly diagnose and select an appropriate antibiotic [1,5,7,12]. In addition, transurethral abscess surgery can prevent prostate abscess recurrence and/or chronic complications in the urinary system in patients with unstable vital signs or prostate abscess size ≥2 cm [10,16] (Table 3).
Generally, third-generation cephalosporin and fluoroquinolone are recommended as empirical antibiotics, but rapid administration of carbapenem was effective in some cases such as those that were progressing to sepsis and those that showed antibiotic susceptibility in the culture test; therefore, the analysis of treatment outcomes or prognosis is quite limited [6,15] (Table 2). According to a recently published study, prostate abscesses smaller than 1-2 cm can be treated with antibiotics alone; however, the duration of antibiotic use can be further reduced when it is accompanied by percutaneous drainage or surgical treatment [1]. Thus, in this study, prostate abscesses were classified according to a cutoff size of 2 cm, and factors, in terms of treatment modality and outcomes, were compared and analyzed, along with the appropriate use of antibiotics.
Transurethral abscess deroofing was performed in two patients in group A whose prostate abscess size was <2 cm because their urine and blood cultures were persistently positive, and their clinical course showed slow improvement in blood indicators such as leukocytosis and C-reactive protein levels. Patients in group A had a relatively shorter hospital stay and intravenous antibiotic use. Meanwhile, 11 patients in group B with prostate abscess size >2 cm progressed to septic shock, of whom five were admitted to the intensive care unit, and one death was reported, indicating that treatment of a large prostate abscess is relatively difficult. The only difference in the treatment modality between the two groups was transurethral prostate abscess surgery, which was performed relatively more often in group B (12/15 cases, 80.0%) than in group A (2/10 cases, 20.0%). In group B, the durations of hospitalization and intravenous antibiotics were longer due to intensive care unit admission and postoperative management, but there was no significant difference in long-term prognosis in terms of recurrence or chronic complications [13,17].
1. Limitations
As this study was conducted retrospectively, it was difficult to exclude selection bias between the two groups of patients in factors such as underlying medical history and age. In terms of antibiotics treatment, it is practically impossible to apply a standardized treatment; thus, there is a limitation in the strict evaluation of the treatment modality. Moreover, clear identification of patients’ chronic complications was difficult because subjective symptoms were tracked based on an outpatient visit [17-19]. This study is meaningful because it analyzed whether transurethral prostate abscess drainage improves treatment outcomes according to the size of the prostate abscess; nevertheless, future research on a well-organized, large-scale patient group is needed.
CONCLUSIONS
Prostate abscess is a serious disease of the urinary system, and timely diagnosis through the use of an abdominal CT scan or transrectal ultrasound along with blood test results and urine and blood culture test results is important. Prostate abscesses can be effectively treated with appropriate antibiotics and surgical treatment. In particular, if transurethral prostate abscess drainage surgery is actively considered in the treatment of patients with prostate abscesses larger than 2 cm, it may contribute to the reduction of septic shock and mortality and prevention of the recurrence of prostate abscesses and chronic urinary complications.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
G.K.L. participated in data collection, performed the statistical analysis, and wrote the manuscript. B.J.K. participated in the study design, helped to draft the manuscript. K.H.J., W.S.S., K.H.K., and H.K.H. read and approved the final manuscript.