The Feasibility of Radical Prostatectomy for Medication Refractory Chronic Prostatitis/Chronic Pelvic Pain Syndrome
Article information
Abstract
Purpose
The purpose of this study was to compare the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) scores of patients with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) given pharmacological treatment with those who additionally had prostate cancer and underwent surgical treatment.
Materials and Methods
From January 2000 to March 2021, a total of 7,650 patients were diagnosed with chronic prostatitis (N41.1) at our hospital, of which 234 patients were additionally diagnosed with prostate cancer. After excluding patients with severe benign prostatic hyperplasia (>100 g)-related lower urinary tract symptoms or neurological and psychiatric abnormalities, or advanced prostate cancer, 52 patients undergoing pharmacological treatment with a combination of drugs and 20 patients who underwent radical prostatectomy due to additional prostate cancer were included in the analysis. The NIH-CPSI scores of the two groups were compared at the first outpatient visit, 3 months, and 6 months after the first visit. The p-values were calculated using the Mann-Whitney U test, and the Wilcoxon signed rank test.
Results
Patients who underwent radical prostatectomy for prostate cancer showed significant reductions in the voiding and quality of life scores in the NIH-CPSI, but not the pain score at 3 months. After 6 months, there was a significant decrease in the overall NIH-CPSI. On the other hand, in the group on pharmacological therapy, the decrease was statistically significant only in the voiding score at 6 months. However, in the surgery group, 3 patients were found to be suffering from urinary incontinence, and 7 patients from erectile dysfunction.
Conclusions
Radical prostatectomy, therefore, appears to be a promising treatment that can be carefully considered for patients with refractory CP/CPPS who do not receive adequate treatment and thus have a poor quality of life.
INTRODUCTION
Chronic prostatitis is a common condition experienced by nearly 50% of Korean adult males at least once in their lifetime [1]. Its characteristic symptoms include pain in the genitourinary tract and during ejaculation, which causes a decreased libido and impotence and significantly affects the quality of life (QoL) [2].
The National Institutes of Health (NIH) Category III prostatitis or chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is characterized by chronic pelvic pain and urinary symptoms in the absence of urinary tract infections. CP/CPPS is a debilitating condition that can affect men of all ages and results in a poor QoL. The etiology of CP/CPPS remains unclear and often requires a multimodal approach to management. Previous studies have shown that pharmacological treatment with a combination of drugs is not very effective in many patients [3]. Indeed, CP/CPPS is often refractory to pharmacological agents. Radical transurethral resection of the prostate in CP/CPPS has also given mixed results and is not the standard of care for patients with this condition [4]. None of the studies to date have investigated the feasibility of radical prostatectomy for medication refractory CP/CPPS.
In the present study, we identified the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) for patients with only CP/CPPS who were additionally diagnosed with prostate cancer and underwent radical prostatectomy. The aim was to analyze whether radical prostatectomy could be a treatment option in patients with refractory CP/CPPS. The data were reviewed retrospectively and indirectly.
This work was approved by the Institutional Review Board of Sungkyunkwan University School of Medicine, Samsung Medical Center (SCMC 2022-04-011).
MATERIALS AND METHODS
From January 2000 to March 2021, a total of 7,650 patients were diagnosed with chronic prostatitis (N41.1) at our hospital. Of these, 7,332 patients were CP/CPPS or NIH Category III prostatitis, of which 234 patients were additionally diagnosed with prostate cancer.
We identified 102 patients who took the NIH-CPSI survey at their first outpatient visit, and 3 and 6 months later, of which 70 patients were diagnosed with only CP/CPPS. A total of 30 patients underwent radical prostatectomy for prostate cancer. We excluded patients with severe benign prostatic hyperplasia (>100 g)-related lower urinary tract symptoms, neurological and psychiatric abnormalities, or advanced prostate cancer. Finally, for the study, we identified 52 patients undergoing pharmacological treatment and 20 patients who had undergone radical prostatectomy for prostate cancer.
The NIH-CPSI scores of the two groups were compared at the first outpatient visit, and 3 months and 6 months later. The p-values were calculated using the Mann–Whitney U-test and the Wilcoxon signed rank test. Since the number of patients was small, we did not analyze the differences between the methods.
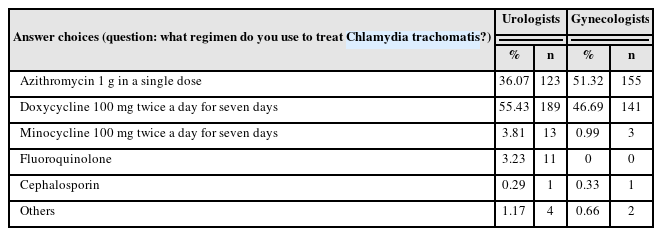
The patients on pharmacological treatment were treated with 5alpha-reductase inhibitors such as finasteride and dutasteride, pentosane polysulfate, alpha-blockers, various analgesics, and alprazolam. Statistical analysis was performed using PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA), and p<0.05 was used to signify statistical significance.
RESULTS
The average age of the 20 patients with CP/CPPS and prostate cancer who underwent surgery was 70.0 (64.5-72.0) years, the average prostate size was 38.0 (27.5-51.0) g, the prostate-specific antigen (PSA) was 7.2 (6.0.-8.2) ng/ml, and the preoperative NIH-CPSI showed a pain score of 9.0 (7.5-10.0), a voiding score of 6.5 (6.0-7.5), and a QoL score of 5.0 (4.0-5.0). Furthermore, 5 patients underwent laparoscopic surgery, 2 patients had open surgery, and 13 patients underwent robotic radical prostatectomy.
The average age of the 52 patients on pharmacological treatment was 43.0 (33.0-49.5) years, the average prostate size was 35.5 (23.0-42.5) g, and the PSA was 2.1 (1.5-3.1) ng/ml. Before medical treatment, the NIH-CPSI showed a pain score of 9.0 (7.0-10.0), a voiding score of 7.0 (6.0-7.0), and a QoL score of 4.0 (4.0-5.0). Since the surgical treatment group also had prostate cancer, statistical differences in age and PSA as compared to the group on drug treatment were expected. However, there was no statistically significant difference in the pain, voiding, and QoL scores before treatment (Table 1).
After 3 months of surgery, the NIH-CPSI showed a pain score of 7.0 (5.5-10.0), voiding score of 5.0 (4.5-6.0), and QoL score of 3.0 (2.5-4.0). There was a statistically significant decrease in the voiding and QoL scores (p=0.144, 0.011, <0.001).
The NIH-CPSI of the group on drug treatment, after approximately 3 months showed a pain score of 8.0 (8.0-10.0), voiding score of 6.5 (5.0-8.0), and QoL score of 4.0 (4.0-5.0). There was no statistically significant decrease in any of these scores (p=0.595, 0.257, 0.218). The NIH-CPSI within 6 months of the surgery showed a pain score of 4.5 (3.0-4.5), voiding score of 3.0 (2.0-4.5), and a QoL score of 2.0 (1.0-2.5). All three scores showed a statistically significant decrease (p<0.001, <0.001, <0.001).
On the other hand, the pain score of the group on drug treatment was 9.0 (8.0-10.0), the voiding score was 7.0 (6.0-8.0), and the QoL score was 4.0 (4.0-5.0); thus, only the voiding score showed a statistically significant decrease (p=0.245, 0.050, 0.135) (Table 2).
However, the results revealed that of the patients in the surgical group, 3 suffered from urinary incontinence after prostate surgery, and 7 patients suffered from erectile dysfunction. Among these patients, 3 showed biochemical recurrence, two received radiation therapy, and one received androgen-deprivation therapy.
Twelve out of the 52 patients in the drug treatment group showed refractory CP/CPPS, and, after 6 months, 10 patients were lost to follow up. Two out of 20 patients in the surgery group had refractory CP/CPPS but showed complete resolution after 6 months. The number of refractory CP/CPPS patients was small, so a direct comparison between the two groups was not conducted.
DISCUSSION
CP/CPPS is a heterogenous urological condition that manifests with varied clinical symptoms at presentation. CP/CPPS has been on the rise in recent years and the prevalence in adult Korean males has been reported to be in the range of 5-9% [5].
The etiology and exacerbating factors of CP/CPPS are believed to be a result of complex interactions between psychosocial, psychological, and neurological causes, in addition to inflammation, and infection. Hence, the present study was conducted for a more objective investigation, on CP/CPPS patients excluding those with neurological or psychiatric and infectious diseases, large prostates (>100 g), or advanced prostate cancer. Due to a poor understanding of the disease etiology, medical treatment involves the use of multiple agents. However, it is often refractory to therapy, which in turn severely impairs patient QoL. These patients are often surgically treated for better outcomes. Chopra et al. [6] had reported the results of robotic radical prostatectomy in 4 patients with drug-refractory CP/CPPS earlier. NIH-CPSI, International Prostate Symptom Score (IPSS), and Sex Health Inventory for Men (SHIM) surveys in these patients showed that all patients recovered from urinary incontinence within 6 months after surgery, with one patient showing an improvement of mild urethral stenosis afterward. In this study, lower urinary tract symptoms and pelvic/perineal pain were resolved in all 4 patients, but erectile dysfunction occurred in 3 patients. Krongrad and Shenghan [7] reported the initial results of laparoscopic prostatectomy in six severe CP/CPPS patients in phase 2 clinical trials. The results confirmed that, in all six patients, the CPSI score at the 6th month was statistically lower than the preoperative score.
In another study, Frazier et al. [8] reported the results of 5 patients who did not respond to analgesics and anti-biotics and underwent total prostatectomy. Of these, 3 patients had complete pain relief shortly after surgery, and in one patient pain dropped from 10 to 1. The other patient felt complete relief from pain after 4 months.
Previous studies have shown that significant symptom improvement was seen 4 to 6 months after surgery. In our study too, the voiding and QoL scores showed statistically significant decreases in the 3rd month. However, the decrease in pain did not reach a statistically significant level. In the 6th month, it was observed that the NIH-CPSI scores were lower in all areas compared to the preoperative scores.
However, in the drug treatment group, only the voiding score showed a statistical decrease after 6 months.
While previous studies targeted medical refractory CP/CPPS patients, our study was different as it targeted CP/CPPS patients, not only refractory patients.
In our study, propensity score matching was done to overcome the limitations of the differences in the patients’ backgrounds because of the retrospective nature of the study. The results of the analysis of the patient characteristics revealed that there was no statistical difference other than age and PSA, which inevitaly differed because of cancer patient. Propensity score matching was not carried out. In the surgical group, the size of the prostate was large, but there were no statistical differences. Since it is a retrospective study, there may have been a mistake in the data survey process.
The results of the present study confirmed that 3 patients showed urinary incontinence, and 7 patients complained of erectile dysfunction at the six-month follow-up; the exact details of the survey were, however, not confirmed. There were a lot of parts that we couldn't check on the charts. In addition to the NIH-CPSI score, we wanted to include an analysis of the scores of the International Index of Erectile Function, IPSS, and the SHIM, but these were not recorded and unavailable because ours was a retrospective survey.
In other studies, since surgery was performed for the treatment of CP/CPPS, the psychological impact of the surgery was possibly also reflected in the survey. However, in our study, patients did not undergo surgery for CP/CPPS treatment but underwent surgery for prostate cancer. Therefore, it is possible that the psychological impact had a smaller influence on this survey, but our study has the limitation of a lack of further analysis of the psychological effects.
In our study, the patient cohort was small, even though there were more patients than in previous studies. There was also a limitation in that long-term results were not confirmed because questionnaire administration after 6 months was limited.
The NIH-CPSI score was not recorded exactly at the end of 3 or 6 months, therefore the accuracy of the time of assessment is unclear.
CONCLUSIONS
Patients who underwent radical prostatectomy for prostate cancer showed significant reductions in the voiding and QoL scores, but not the pain score, as estimated by the NIH-CPSI at 3 months. After 6 months, there was a significant decrease in the overall scores. On the other hand, in the drug treatment group, the decrease was statistically significant only in the voiding score at 6 months. However, 3 out of 20 patients suffered from urinary incontinence, and 7 patients from erectile dysfunction after surgery. Radical prostatectomy can be carefully considered as an option for the management of patients with refractory CP/CPPS with a severely compromised QoL.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.