Rates and Risk Factors of Bacteriuria in Patients with Bladder Cancer Who Underwent Treatment with Bacillus Calmette-Guérin
Article information
Abstract
Purpose
This study evaluated the rate and predictors of bacteriuria in patients who underwent transurethral resection of bladder tumor (TURBT) and Bacillus Calmette-Guérin (BCG) treatment.
Materials and Methods
We prospectively evaluated 266 patients who underwent TURBT and intravesical BCG treatment between January 2017 and September 2019. Urinalysis and urine culture were performed at the baseline, one to two weeks after TURBT and weekly during the BCG treatment period. The primary outcomes were the bacteriuria rates in BCG-treated patients, while the secondary outcomes were the risk factors of bacteriuria during BCG treatments.
Results
Of the 266 patients, the rate of bacteriuria was 4.5% before TURBT, 5.3% in the postoperative period, and 24.4% in the BCG treatment period. After BCG instillation, urinalysis showed that 204 and 38 patients tested positive for pyuria and nitrite, respectively. Multivariate analysis indicated that the risk factors associated with bacteriuria during BCG treatment included age (odds ratio [OR]: 1.06; p=0.003), sex (female) (OR, 5.41; p=0.007), diabetes mellitus (DM) (OR, 2.82; p=0.023), postoperative bacteriuria (OR, 8.08; p=0.032), bacterial counts>100/ml in urine flow cytometry (OR, 29.72; p<0.001), and positive urine nitrite test (OR, 6.20; p=0.001) at the time of positive urine culture sampling.
Conclusions
Approximately 25% of the patients suffered from bacteriuria during intravesical BCG treatment. Old age, female sex, DM, and postoperative bacteriuria were found to be the risk factors of bacteriuria during BCG treatment. Predictive factors could aid in clinical decisions during BCG treatments as well as decisions on BCG discontinuation.
INTRODUCTION
Bladder cancer is the sixth most prevalent cancer and the most common urogenital malignancy [1,2]. Following a transurethral resection of the bladder, adjuvant intravesical immunotherapy with Bacillus Calmette-Guérin (BCG) is the standard treatment in patients with high-risk, non-muscle- invasive bladder cancer. This treatment reduces the risk of disease recurrence, delays progression, and improves the overall survival [1,3,4]. On the other hand, BCG therapy is potentially associated with a significant risk of localized or systemic adverse events, such as mycobacterial infections [5]. Urinary tract infection (UTI) is considered a risk factor for BCG complications. Hence, symptomatic UTI is an absolute contraindication to this therapy [3]. Therefore, many urologists believe that BCG therapy should be performed only in patients with sterile urine [6]. Some experts believe that bacterial cystitis traumatizes the barrier, allowing BCG to reach the bloodstream [7].
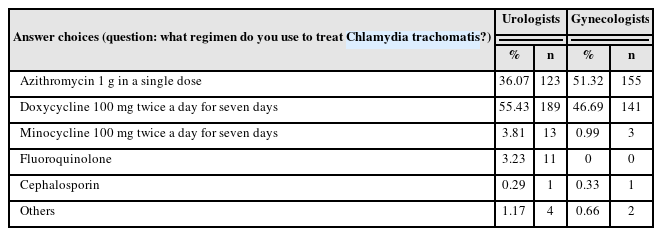
A urine culture is time-consuming. Hence, based on pyuria, many urologists administer prophylactic antibiotics before and after BCG treatment to prevent acute UTI or bacterial sepsis. On the other hand, while the clinical benefit is unclear, this antimicrobial treatment delays the adjuvant oncological treatment and potentially contributes to an increase in bacterial antibiotic resistance [8]. Simul-ta-neously, pyuria on the day of BCG instillation (without a positive urine culture test) appears to be one of the most common reasons for the delay of BCG immunotherapy, which may reduce the clinical efficacy of the treatment.
Therefore, detecting bacteriuria and identifying the risk factors can be helpful in BCG treatment. Accordingly, this study evaluated the bacteriuria rates and risk factors in patients who underwent a transurethral resection of bladder tumors (TURBT) and BCG treatment.
MATERIALS AND METHODS
1. Ethics Statement
The Institutional Review Board of the Chonnam National University Hwasun Hospital (IRB no. CNUHH-2018-007) approved this ongoing pattern of care study in bladder cancer patients receiving intravesical BCG, permitting the collection of prospective data on these patients. All study procedures were performed in accordance with the Declaration of Helsinki guidelines.
2. Patients and Samples
Two hundred sixty-six patients who underwent TURBT and intravesical BCG treatment between January 2017 and September 2019 were evaluated prospectively. Urinalysis and urine culture were performed at the baseline and one to two weeks after TURBT. In patients who also underwent intravesical BCG treatment, the urinalysis and urine culture were performed weekly during the BCG treatment period. Patients diagnosed with muscle-invasive urothelial carcinoma post-TURBT and those with a clinical stage of T3 or T4 were excluded. Midstream urine specimens were collected in sterile containers for urinalysis and culture. These specimens were placed in 10 ml urine sediment centrifuge tubes and sent to the laboratory for chemical analysis and laser flow cytometry (Sysmex UF-1000i; Sysmex, Kobe, Japan). Sysmex UF-1000i analysis was performed within 30 minutes after collection (standard urinalysis in the hospital was performed with Sysmex UF-1000i and one chemistry analyzer). The results of the sediment analysis are presented in terms of units per ml and units per high power field. The primary outcomes were the rates of pyuria and bacteriuria (≥105 CFU/ml in midstream urine) in the BCG-treated patients. The secondary outcomes were the risk factors of bacteriuria during the BCG treatments. For preventative antibiotic treatment, 1 g of ciprofloxacin was administered one week before the BCG treatment, but the prophylactic use of antibiotics is not recommended in a BCG treatment. Physicians should use discretion in the management of symptoms during BCG therapy and the prophylactic use of antibiotics in patients with a high risk of infection because the use of antibiotics might reduce the incidence of side effects. In the present study, discon-tinuance of BCG depended mostly on the patients’ com-plaints and physician’s decisions if there were major side effects.
3. Statistical Analysis
The baseline characteristics are presented as frequencies (percentages) for categorical variables and median (interquartile range [IQR]) for continuous variables. The baseline patient demographics were analyzed using descriptive statistics. The data were compared using a Mann–Whitney U-test and Kruskal–Wallis analysis for the quantitative variables and a chi-test for the categorical variables. Univariate and multivariate logistic regression analyses were performed to assess the respective effects of each variable on the occurrence of bacteriuria. The results of standard urine culture staining, microscopic sediment analysis, nitrite test, and UF-1000i flow cytometry results were compared. Using receiver operating characteristic (ROC) curves, bacteriuria on the Sysmex UF-1000i, the diagnostic performance of the method was also evaluated by determining the sensitivity, specificity, positive predictive value, and negative predictive value. A p-value <0.05 was considered statistically significant. All statistical analyses were conducted using IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Of the 266 patients included, 232 (87.2%) were males, and the median age was 70 years (IQR, 63-78 years). Appro-ximately 229 patients underwent only BCG induction therapy, whereas 31 patients underwent induction and maintenance BCG therapy. During BCG instillation, prophylactic and therapeutic antibiotics were administered to 75 (28.2%) and 31 (11.7%) patients, respectively. The discontinuation rate of BCG instillation was 59 (22.2%) (Table 1).
Bacteriuria was observed in 12 patients (4.5%) in the baseline state, 14 (5.3%) in the postoperative period, and 65 (24.4%) in the BCG treatment period. After BCG instillation, urinalysis revealed pyuria in 204 patients (76.7%) and nitrite (+) in 38 patients (14.3%) (Table 2, Fig. 1).

Purpose: This study evaluated the rate and predictors of bacteriuria in patients who underwent transurethral resection of bladder tumor (TURBT) and Bacillus Calmette-Guérin (BCG) treatment.
The pyuria test had a low specificity (28.36%), whereas the nitrite test had high specificity (94.53%) but low sensitivity (41.54%). Urine flow cytometry showed high sensitivity, particularly when bacterial counts of more than 100/ml were used as the cut-off values; a cut-off value of >100 CFU/ml resulted in a sensitivity and specificity of 93.85% and 72.14%, respectively (Table 3).
Multivariate analysis indicated that the risk factors associated with bacteriuria during the BCG treatment included the age (odds ratio [OR], 1.06; p=0.003), sex (female) (OR, 5.41; p=0.007), DM (OR, 2.82; p=0.023), immediate postoperative bacteriuria (OR, 8.08; p=0.032), bacterial counts >100/ml in urine flow cytometry (OR, 29.72; p<0.001), and positive urine nitrite test (OR, 6.20; p=0.001) at the time of sampling the positive urine culture. Prophylactic antibiotics were not associated with bacteriuria after the BCG treatment (p=0.62) (Table 4).
The ROC curves were used to detect bacteriuria by urine flow cytometry when <105 CFU/ml was chosen as the gold standard definition for negative cultures. The area under the ROC curve for the diagnosis of bacteriuria by post-BCG urine flow cytometry was 0.888 (Fig. 2).

Conclusions: Approximately 25% of the patients suffered from bacteriuria during intravesical BCG treatment. Old age, female sex, DM, and postoperative bacteriuria were found to be the risk factors of bacteriuria during BCG treatment. Predictive factors could aid in clinical decisions during BCG treatments as well as decisions on BCG discontinuation.
DISCUSSION
In this study, the overall incidence of culture-documented UTI was 4.5% in the preoperative period and 5.3% in the postoperative period. The incidence increased to 24.4% during the BCG treatment period. The age (OR, 1.06; p=0.003), sex (female) (OR, 5.41; p=0.007), DM (OR, 2.82; p=0.023), postoperative bacteriuria (OR, 8.08; p=0.032), bacterial counts >100/ml in urine flow cytometry (OR, 29.72; p<0.001), and positive urine nitrite test (OR, 6.20; p=0.001) at the time of sampling the positive urine culture were found to be independent risk factors for bacteriuria during the BCG treatment.
BCG is a potent intravesical biological agent that decreases the recurrence and progression rates of high-grade urothelial carcinoma. Although safe, intravesical BCG can cause fever, influenza-like symptoms, and rarely, BCG sepsis. Active UTI can promote intravasation, leading to infectious complications. Abnormal urinalysis or UTI is considered a contraindication to intravesical BCG [3].
UTIs are considered a risk factor for BCG complications, and symptomatic UTIs are an absolute contraindication to the therapy [9]. The association between UTI and the safety of BCG therapy was poorly studied, and the evidence in this field is limited. Many urologists consider sterile urine to be a necessary condition for intravesical BCG instillation. Moreover, they believe that bacterial cystitis traumatizes the barrier for the BCG to reach the bloodstream [7].
The antimicrobial treatment during BCG treatment delays adjuvant oncological treatment and potentially contributes to the increase in bacterial resistance to antibiotics, but the clinical benefit is unclear [10].
Herr et al. [11] reported that the instillation of BCG into bladder cancer patients with asymptomatic bacteriuria (ABU) did not result in sepsis or a reduced response. Although the best-practice guidelines have outlined the use of antimicrobial therapy around the time of urological surgery [9], there are no consensus guidelines that address the prevention of infection-related complications arising from intravesical chemotherapy or intravesical biological therapy [6].
Multivariate analysis showed that prophylactic antibiotics were not associated with bacteriuria after the BCG treatment (p=0.62). If the findings are replicated, a urine culture to detect bacteriuria and prophylactic antibiotics may be unnecessary in asymptomatic patients with bladder cancer.
ABU is common in patients with bladder cancer undergoing induction BCG therapy. Intravesical BCG immunotherapy in bladder cancer patients with ABU remains controversial. There is no evidence to support the routine treatment of ABU in patients scheduled for intravesical BCG instillations due to bladder cancer [10].
Asymptomatic patients (with bacteriuria detected by flow-cytometry) can be excluded safely from antibiotic therapy during BCG instillation [10,12,13], and routine urine analysis can be omitted safely before BCG instillation. On the other hand, symptomatic UTI is considered a risk factor of BCG complications, and symptomatic UTI is an absolute contraindication to BCG therapy [9].
There is insufficient evidence on whether irritative bladder symptoms (e.g., cystitis or pyuria on urinalysis) are sufficient to decide on whether to pursue antibiotic therapy and postpone or continue BCG treatment. These symptoms might not indicate UTI because mild to moderate irritative urinary symptoms are common in cases of a recent transurethral resection and in situ carcinoma. Irritative symptoms, such as urgency and frequency, are commonly observed in patients who undergo TURBT and subsequent intravesical therapy [14].
Many patients receiving BCG treatment have lower urinary tract symptoms, such as dysuria, frequency, urgency, and hematuria, which cannot be differentiated from UTI symptoms. Although symptomatic UTIs remain a contrain-dication for BCG therapy, bacteriuria could not be assessed on the day of the BCG treatment.
According to this study, a urine flow cytometry result of >100 bacteria/ml (OR, 29.72; p<0.001) at the time of sampling for a positive urine culture was a predictor for bacteriuria. These results could be determined before urine cultures. Therefore, the Sysmex UF-1000i system can be used to accurately predict a positive urine culture and avoid unnecessary BCG discontinuation and urine cultures. Severe dysuria or fever with bacteriuria (detected on flow-cyto-metry) before the BCG treatment might indicate symptomatic UTI. Therefore, proper pre-treatment evaluation is indi-cated. On the other hand, pyuria and irritative urinary symptoms without bacteriuria (i.e., not detected on flow-cytometry) might not indicate symptomatic UTI. In this case, antibiotic treatment or postponing the BCG treatment is not recommended. The results of this study suggest that the automated urine sediment analyzers UF-1000i may be used as effective screening tools for symptomatic UTI by measuring the bacterial content of urine samples.
Various cut-off points of the bacterial count have been reported in UTI screening. When urine cultures growing at >105 CFU/ml were used as a reference, the bacterial count of 100/ml, as the cut-off, resulted in a sensitivity and specificity of 96.5% and 86.7%, respectively [15]. Giesen et al. [16] reported the optimal cut-off bacterial count of 288.9/ml with a sensitivity and specificity of 89% and 79%, respectively. Recent meta-analysis reviewed recent studies to determine the capabilities of Sysmex UF-1000i to detect bacteriuria in UTI screening [17]. The pooled sensitivity and specificity were 87% and 60%, respectively, for bacteriuria. The area under the curve was 0.93 for bacteriuria.
In this study, urine flow cytometry showed high sensitivity, particularly when bacterial counts of more than 100/ml were used as the cut-off values. A cut-off value of >100 CFU/ml resulted in a sensitivity and specificity of 93.85% and 72.14%, respectively. The area under the ROC curve for the diagnosis of bacteriuria by urine flow cytometry was 0.88.
In the general population, the white blood cell (WBC) count and bacterial measurements by UF-1000i are useful indicators in UTI screening [17]. On the other hand, the WBC measurements by the UF-1000i are not useful indicators in UTI screening in patients with bladder cancer who have undergone treatment with BCG.
Based on the study findings, urinalysis should be considered in patients with a risk factor of bacteriuria during the BCG treatment. Bacteria resistance to antibiotics is a severe problem, and the risk factors or flow cytometry cannot predict the bacterial sensitivity to antibiotics. Symptomatic patients with bacteriuria detected by flow-cytometry should undergo urine culture, and antibiotic therapy should be considered before BCG instillation.
This study had several limitations. The study was limited by a small number of patients treated by one surgeon in a single center. Another study limitation is that the current study was prospective; it was not randomized to prophylactic antibiotic treatments. There were insufficient guidelines about bacteriuria patients in BCG treatment. Therefore, there is no consensus on the optimal management of symptoms and the use of antibiotics in patients who received BCG therapy. Additional prospective studies will be needed to evaluate the managements further according to the risk factors of post-BCG bacteriuria and the results of urine flow cytometry.
CONCLUSIONS
Approximately 25% of the patients suffered from bacteriuria during the intravesical BCG treatment. Old age, female, DM, and postoperative bacteriuria were the risk factors of bacteriuria after the BCG treatment. Prophylactic antibiotics are not recommended for the prevention of bacteriuria following the BCG treatment. Urine flow cytometry could help in a bacteriuria diagnosis in BCG-treated patients. The predictive factors and prediction of UTIs by urine flow cytometry could aid in clinical decisions during the BCG treatments and on BCG discontinuation.
ACKNOWLEDGMENTS
This study was supported by a grant (HCRI 19017) from the Chonnam National University Hwasun Hospital Institute for Biomedical Science.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
S.J.E. participated in data collection and wrote the manuscript. H.J.C. participated in data collection. M.S.K. participated in the study design and performed the statistical analysis. H.S.C. and E.C.H. performed the statistical analysis. S.I.J. participated in the study design and coordination and helped to draft the manuscript. D.D.K. participated in coordination. All authors read and approved the final manuscript.