Is Preoperative Pyuria Associated with Postoperative Febrile Complication after Ureteroscopic Ureter or Renal Stone Removal?
Article information
Abstract
Purpose
The association between preoperative pyuria and postoperative febrile complications after ureteroscopic ureter or renal stone removal was examined.
Materials and Methods
From June 2014 to July 2016, 110 patients who underwent ureteroscopic ureter or renal stone removal by a single surgeon were evaluated. The patients were categorized as the “pyuria group” and “nonpyuria group.” The sex, age, stone laterality, stone location, stone size, preoperative urine culture results, and postoperative complications in each group were analyzed.
Results
The pyuria and nonpyuria groups were comprised of 55 patients each. The mean ages the pyuria and nonpyuria groups were 58.4±16.1 years and 54.4±13.2 years, respectively. There were respectively, 43 and 12 unilateral and bilateral stones in the pyuria group, and 53 and two in the nonpyuria group. The stone sizes of the pyuria and nonpyuria groups were 13.1±5.4 mm and 11.1±4.7 mm, respectively. The pyuria group contained more patients with bilateral stones and larger stones than the nonpyuria group. Five and two postoperative febrile complications were encountered in the pyuria group and the nonpyuria group, respectively. No significant difference in febrile complications was observed between the two groups. In logistic regression analysis, bilateral stones and larger stones were associated with pyuria.
Conclusions
In ureteroscopic stone removal surgery, preoperative pyuria was associated with bilateral and larger stones, but there were no associations with febrile complications.
INTRODUCTION
Ureteral and renal stones are a clinically important disease in the urological field because they can result in several complications, including pain, renal function deterioration, inflammation, and fever. Urinary obstruction with urinary stones is the most common cause of urosepsis [1,2]. Therefore, urinary stones need to be removed to prevent and relieve urinary obstructions, particularly to prevent infectious complications.
The management of kidney and ureteral stones has improved with endoscopic techniques, such as ureteroscopy (URS), which is the most common therapeutic procedure [3]. Several reports have revealed high success rates and low complication rates involved in undergoing ureteroscopic surgery for urinary stones [4-8]. De la Rosette et al. [7] analyzed 11,885 patients treated with URS between 2010 and 2012 using the Clinical Research Office of the Endourological Society (CROES) database, which collected data from 114 centers in 32 countries. The authors reported that the stone-free rate was 85.6%, with a postoperative complication rate of 3.5%; fever was the most frequent complication (2.8%).
Although ureteroscopic stone removal is a safe and effective technique, postoperative complications, particularly febrile urinary tract infection (UTI), can occur. Daels et al. [9] reported that certain risk factors, including diabetes mellitus, anticoagulation use, cardiovascular disease, or obesity, were associated with complications.
On the other hand, the factors associated with postoperative infectious complications after ureteroscopic stone removal have not been examined in detail [10]. Therefore, this study examined the association between preoperative pyuria and postoperative febrile complications after the ureteroscopic removal of ureter or renal stones.
MATERIALS AND METHODS
From June 2014 to July 2016, 114 patients, who underwent semirigid, flexible ureteroscopic ureter, or renal stone removal by a single surgeon (Seungsoo Lee), were evaluated. Four patients with anuria due to bilateral ureteral stones were excluded. The patients were categorized as the “pyuria group” and “nonpyuria group.” Sex, age, stone laterality (unilateral or bilateral), stone location (kidney, upper, mid, or lower ureter), stone size, preoperative urine culture results, and postoperative complications were analyzed. Pyuria was defined as the presence of six or more white cells per high-power field in a urine specimen. If a patient had multiple stones, the laterality, location, and the size of the largest stone were analyzed.
Statistical analyses were performed using IBM SPSS Statistics version 20.0 (IBM Corp., Armonk, NY, USA), and p-values <0.05 were considered significant. A student’s t-test and Pearson’s chi-square test were applied to assess the differences between the groups. Logistic regression analysis was applied to evaluate the factors related to pyuria.
RESULTS
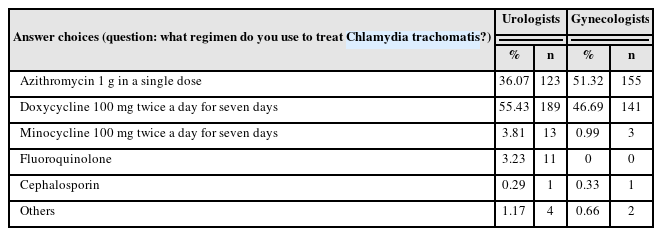
The pyuria group and nonpyuria group each comprised 55 patients: 34 males and 21 females in the pyuria group and 36 males and 19 females in the nonpyuria group. The mean age in the pyuria group and nonpyuria group was 58.4±16.1 years and 54.4±13.2 years, respectively. In the pyuria group, 43 patients had unilateral stones, and 12 had bilateral stones. In the nonpyuria group, there were 53 patients with unilateral stones and two with bilateral stones. The stones were located in the kidney, upper, mid, and lower ureter in 13, 28, 8, and 6 patients in the pyuria group, respectively, and 14, 23, 6, and 12 patients in the nonpyuria group, respectively. The largest stone size in the pyuria group and nonpyuria group was 13.1±5.4 mm and 11.1±4.7 mm, respectively (Table 1).
No statistical differences in sex, age, and stone location were observed between the two groups (p=0.692, p=0.157, and p=0.421, respectively). On the other hand, the stone laterality and size differed significantly between the two groups (p=0.004 and p=0.036, respectively). The pyuria group had more patients with bilateral stones and larger stones than the nonpyuria group (Table 1).
From the preoperative urine culture, uropathogens were identified in only six cases (10.9%) in the pyuria group and five cases (9.1%) in the nonpyuria group. In the pyuria group, Escherichia coli (non-extended-spectrum beta-lactamases [non-ESBL]) was identified in three cases, and E. coli (ESBL), Streptococcus agalactiae, and Staphylococcus epidermidis were identified in one case each. In the nonpyuria group, E. coli (non-ESBL), E. coli (ESBL), S. agalactiae, Enterococcus faecalis, and yeast-like cells were identified in one case each (Table 1).
Postoperative complications in the pyuria group were fever in five patients (9.1%), gastrointestinal problems in two patients (3.6%), ureteral injury in two cases (3.6%), cardiovascular complication in one patient (1.8%), and urinary retention in one case (1.8%). In the nonpyuria group, the complications were fever in two patients (3.6%), pain in two cases (3.6%), ureteral injury in two patients (3.6%), and bleeding in two cases (3.6%). No significant difference in febrile complications was observed between the two groups (p=0.241) (Table 2).
Logistic regression analysis revealed only stone laterality and stone size to be associated with preoperative pyuria. Bilateral stones and larger stones are tended to show preoperative pyuria (Table 3).
DISCUSSION
Ureteroscopic stone removal is the most widely used surgical treatment method because of its effectiveness and low complication rate. In addition, it has no specific contraindications and can be used for most patients with urinary stones [11]. Decompression for urinary obstruction with ureteroscopic stone removal is important for preventing or relieving urinary infection or urosepsis. On the other hand, postoperative fever is the most frequent complication of ureteroscopic surgery, and it is important to identify patients at risk of developing infectious complications from surgery [7,10,12].
Several studies have examined postoperative febrile UTI after ureteroscopic stone removal. Mitsuzuka et al. [10] reported that 18.3% of 182 patients had postoperative febrile UTI. Sohn et al. [13] analyzed 531 patients who underwent diagnostic URS or ureteroscopic stone removal and reported that 3.8% of patients had infectious complications. In the present study, seven (6.4%) out of 110 patients experienced postoperative fever.
Severe postoperative complications associated with fever, including sepsis, have also been reported, with patients having to undergo special therapies and interventions [10,11]. Fortunately, in the present study, all the postoperative complications were Grade I under the modified Clavien–Dindo grading system [14]. The patients who had fever were treated with medication, including nonsteroidal anti-inflammatory drugs or acetaminophen.
This study examined the relationship between preoperative pyuria and postoperative febrile complications. Mitsuzuka et al. [10] reported preoperative pyuria and acute pyelonephritis to be significant risk factors for postoperative febrile UTI. Moreover, the degree of preoperative pyuria was likely to be associated with postoperative febrile UTI. In the present study, however, pyuria was not associated with postoperative febrile UTI. Although there were more patients with postoperative fever in the pyuria group (five cases) than in the nonpyuria group (two cases), the difference was not statistically significant. In addition, pyuria in urinary stone patients does not always associate with UTI. Urinary stone disease at any level might increase the number of urinary leukocytes caused by stasis-induced ascending infection or localized mucosal inflammatory response [15].
Prophylactic antibiotic therapy may be an important factor for UTI. The use of prophylactic antibiotics in patients undergoing urologic procedures can reduce the incidence of postoperative infectious complications [16-19]. In the present study, all the patients had undergone pre- and postoperative antibiotic treatment. Most patients had cefmetazole (2nd cephalosporin), but other antibiotics were used if a patient had an allergic reaction to cephalosporin or if uropathogens and a resistance pattern were identified from the urine culture. The antibiotic agent, dose, and duration in each patient were not analyzed. Therefore, the difference in antibiotic regimen is one of the limitations in this report.
E. coli is the most common bacterial pathogen associated with urinary infections [20], and in this study, E. coli was also the most identified pathogen; among the six E. coli-identified specimens, two were ESBL.
Six or seven Fr double-J ureteral stents were inserted in the ureter at the end of each surgery. Ureteral stents were inserted in both ureters if a patient had bilateral ureteral stones. The stent was removed after 2 to 4 weeks postoperatively. Another potential limitation was the lack of an evaluation of ureteral stenting duration and laterality.
CONCLUSIONS
In ureteroscopic stone removal surgery, preoperative pyuria was related to bilateral stones and larger stones, but febrile complications were not associated with preoperative pyuria. With appropriate prophylactic antibiotics and postoperative care, ureteroscopic stone removal can be used for patients with preoperative pyuria.
ACKNOWLEDGMENTS
This study was supported by a 2017 research grant from Pusan National University Yangsan Hospital.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.